15 Hidden Atorvastatin Side Effects Your Doctor May Not Have Time to Mention (But You Deserve to Know Before Your Next Refill)
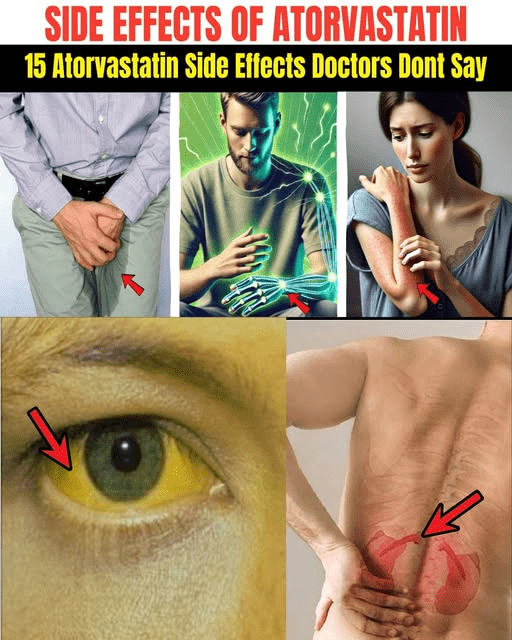
Atorvastatin and Its Less Commonly Discussed Side Effects: What Patients Should Know
Atorvastatin is one of the most widely prescribed statins worldwide and plays an important role in lowering low-density lipoprotein cholesterol (LDL-C) and reducing cardiovascular risk. Large clinical trials have demonstrated its effectiveness in preventing heart attacks and strokes. However, like all medications, atorvastatin is associated with a range of potential side effects that may not always be fully discussed during routine clinical visits, often due to time constraints or the need to prioritize major benefits.
Understanding these effects allows patients to participate more actively in shared decision-making and to recognize when symptoms warrant medical attention.
Commonly Reported Musculoskeletal Effects
Muscle-related symptoms are among the most frequently reported adverse effects of statins. These include muscle pain (myalgia), weakness, and cramps, particularly in the legs. Real-world observational studies suggest that muscle symptoms may affect more patients than originally reported in randomized trials (bold: American Journal of Cardiology). The mechanism is thought to involve interference with muscle energy metabolism, partly through reduced levels of coenzyme Q10.
Joint pain and stiffness have also been reported and may resemble osteoarthritis, making it difficult for patients and clinicians to distinguish drug-related symptoms from age-related changes.
Fatigue, Cognitive, and Mood-Related Symptoms
Some individuals taking atorvastatin report persistent fatigue, reduced exercise tolerance, or a general sense of low energy. This effect may be related to impaired mitochondrial function in muscle cells (bold: Journal of Clinical Lipidology).
Cognitive complaints such as memory lapses or “brain fog” have been documented in post-marketing surveillance. In response, the U.S. Food and Drug Administration added label information noting that certain cognitive effects have been reported and are typically reversible after discontinuation (bold: FDA Drug Safety Communication).
Mood changes, including irritability or depressive symptoms, have also been described, although evidence remains mixed and causality is not firmly established.
Metabolic and Neurological Considerations
Statin therapy has been associated with a modestly increased risk of new-onset type 2 diabetes, particularly in individuals with pre-existing risk factors. Large meta-analyses estimate a relative risk increase of approximately 9–12%, especially at higher doses (bold: The Lancet; JAMA). Despite this, cardiovascular benefits generally outweigh the risk for most patients.
Less commonly, peripheral neuropathy—manifesting as tingling, numbness, or burning sensations in the hands or feet—has been reported. Although rare, symptoms may persist if not addressed promptly (bold: Neurology).
Liver and Serious Muscle Injury Risks
Mild elevations in liver enzymes occur in a small percentage of patients and are usually reversible with dose adjustment or discontinuation. Routine monitoring is recommended, particularly during the first year of therapy (bold: Mayo Clinic Guidelines).
The most serious but rare complication is rhabdomyolysis, a condition involving rapid muscle breakdown that can lead to acute kidney injury. The Mayo Clinic emphasizes that severe muscle pain accompanied by dark urine or profound weakness requires immediate medical evaluation (bold: Mayo Clinic – Statin Side Effects Overview).
What Patients Can Do
Patients should not stop atorvastatin abruptly without consulting a healthcare professional. Instead, experts recommend:
-
Reporting new or persistent symptoms promptly
-
Discussing dose adjustments or alternative lipid-lowering strategies
-
Considering laboratory monitoring (creatine kinase, liver enzymes, glucose markers) when clinically indicated
In many cases, side effects can be managed through dose reduction, switching to another statin, or combining lower-dose statin therapy with non-statin medications.
Conclusion
Atorvastatin remains a highly effective medication for reducing cardiovascular risk, but awareness of its potential side effects is essential. While most adverse effects are mild and reversible, some require careful monitoring and timely medical attention. Informed patients who communicate openly with their healthcare providers are best positioned to balance the benefits of cholesterol reduction with quality of life and long-term safety.
News in the same category

Discover How Baking Soda Could Transform Your Skin’s Appearance in Minutes – Even After 70!

What Happens When You Add Just 2 Garlic Cloves a Day to Your Routine – Even After 50!

13 Subtle Signs Your Kidneys May Need Attention

Stop Shaving? Exploring Popular Home Remedies for Hair Removal

Discover the Hidden Power of Ginger Oil: Why Women Over 65 Are Seeing Thicker, Darker Hair Naturally

Top 10 Foods That May Help Reduce Frequent Nighttime Urination (Nocturia)

Why Toothpaste and Baking Soda Aren’t the Answer for Wrinkles and Dark Spots – And What Might Help Instead

Top Superfoods That Could Support Your Kidney Health in Just 30 Days – The Natural Boost You’ve Been Missing!
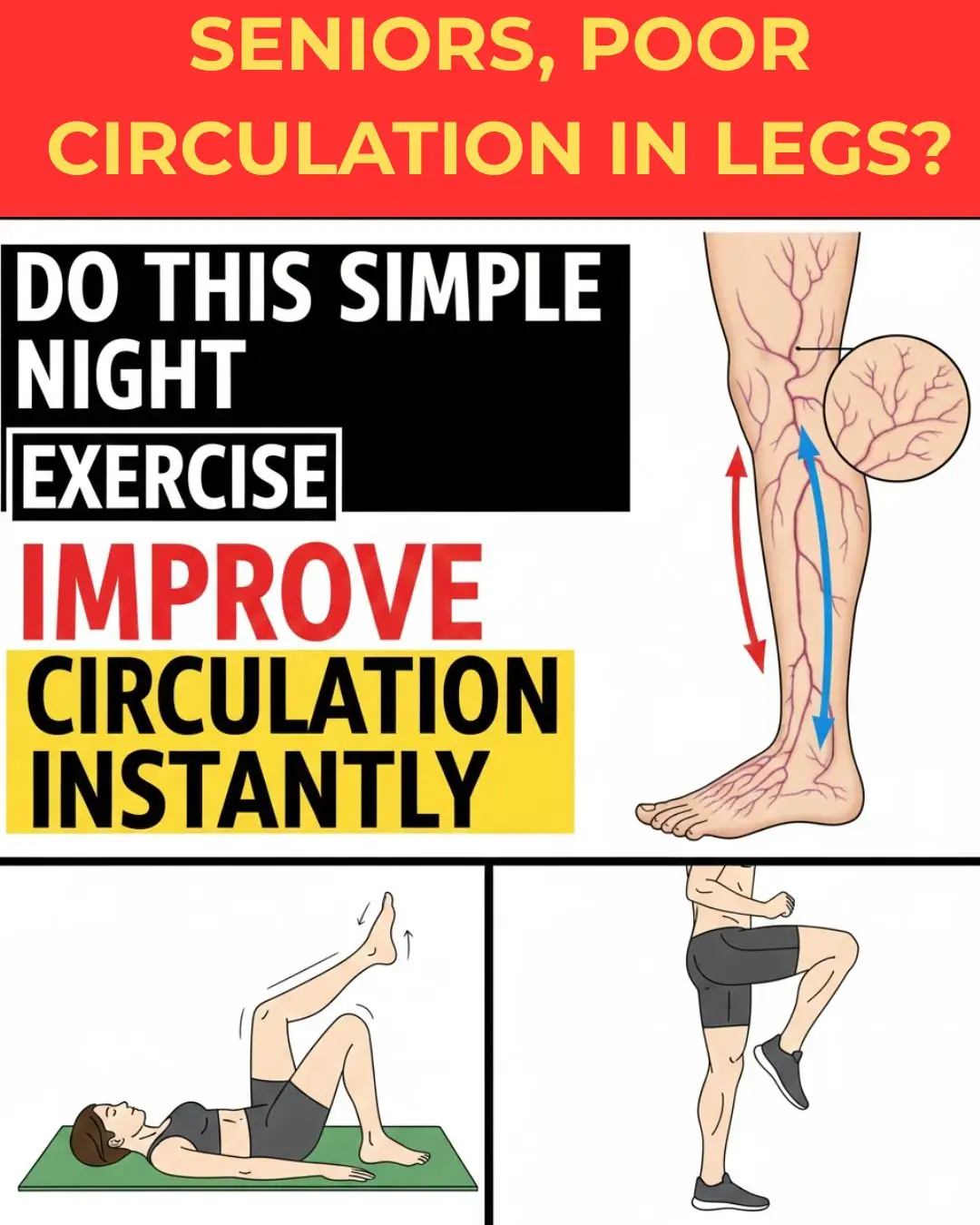
Top 10 Simple Exercises to Improve Circulation & Blood Flow in Your Feet and Legs (Seniors Must Try!)
Cancer Hates These 6 Seeds: Seniors, Add Them Daily for Natural Antioxidant Support!

Seniors, Rub THIS 2-Ingredient Kitchen Mash on Your Face Tonight & Wake to Skin 15 Years Fresher

Transform Your Mornings: Discover the Power of 7 Days of Healthy Smoothies

Discover the Hidden Power of Cloves: Could This Simple Spice Help Your Skin Glow Like Never Before?

Top 3 Nutrients Seniors Need to Stop Leg Cramps and Restore Strength: Reclaim Your Steady Steps Today!

12 Surprising Potential Benefits of Moringa Seeds You Might Not Hear About – But Research Suggests They’re Worth Knowing!

Discover the Timeless Secret of a 95-Year-Old Chinese Doctor: How He Stays Vibrant and Healthy

Bananas, Garlic, and Dates: The Powerful Health Combo
News Post
Which Fruits Should Cancer Patients Avoid and Which Should They Eat?
Advancing Clinical Excellence in IgA Nephropathy

3 types of fruits that are cheap in Vietnamese markets but are considered "pure gold" to protect health

Found this weird skin on my son's ear this morning. Doc appt is a week away. What can I do?

My nana taught me this hack to get rid of dark circles in 5 mins with 0 work. Here’s how it works
What To Know About Chronic Kidney Failure

Could Your Magnesium Supplement Be Causing Side Effects?

Why Thick Toenails Happen, And How To Get Rid of Them

The military sleep method that can help you fall asleep in just two minutes
Garlic with Olive Oil Over 50: The Irreversible Body Reaction Everyone’s Talking About

Discover How Baking Soda Could Transform Your Skin’s Appearance in Minutes – Even After 70!

What Happens When You Add Just 2 Garlic Cloves a Day to Your Routine – Even After 50!

13 Subtle Signs Your Kidneys May Need Attention

Stop Shaving? Exploring Popular Home Remedies for Hair Removal

Discover the Hidden Power of Ginger Oil: Why Women Over 65 Are Seeing Thicker, Darker Hair Naturally

Top 10 Foods That May Help Reduce Frequent Nighttime Urination (Nocturia)

Why Toothpaste and Baking Soda Aren’t the Answer for Wrinkles and Dark Spots – And What Might Help Instead
James Webb Space Telescope Reveals Hidden Mid-Infrared Flares from the Milky Way’s Central Black Hole
New Vision Correction Technique Reshapes the Cornea Without Surgery