Could a Nearly Universal Virus Be the Root Cause of Lupus
Lupus is often considered a puzzling illness because it can affect nearly every system in the body, producing symptoms that vary widely from person to person. New research from Stanford Medicine is helping to clarify this complexity by uncovering a strong connection between lupus and the Epstein–Barr virus (EBV). EBV is extremely common—more than 95 percent of adults around the world carry it, often without even knowing.
Typically, EBV becomes dormant after the initial infection and remains silent for the rest of a person’s life. However, scientists have now discovered that the virus can influence the immune system in surprisingly specific ways. These changes mirror the immune patterns seen in lupus, suggesting that EBV may help trigger the long-term inflammation and autoimmune attacks that define the disease.
This discovery represents a major milestone in lupus research. Rather than relying on theories about environmental triggers or vague immune dysfunctions, researchers can now observe a direct biological sequence of events that may initiate the disease. This also raises the possibility that future therapies could target the virus itself, rather than simply suppressing the immune system.
For individuals living with lupus, this connection offers a clearer understanding of what might be unfolding inside their bodies. In the sections below, we explore how EBV alters immune cells, why only certain people are affected, and what lifestyle choices may help support a healthier immune environment.
A Closer Look at Lupus
Lupus, formally known as systemic lupus erythematosus (SLE), is a chronic autoimmune disease. In autoimmune conditions, the immune system mistakenly attacks the body's own tissues. In lupus, this attack may involve the joints, skin, kidneys, blood cells, lungs, heart, or even the brain.
Symptoms vary greatly. Many people experience persistent fatigue, joint pain, fevers, or the well-known butterfly-shaped facial rash. Inflammation can also affect deeper organs such as the kidneys or nervous system, sometimes leading to serious complications. This wide range of symptoms makes lupus notoriously difficult to diagnose and manage.
Women develop lupus far more often than men. Researchers suspect that hormonal differences—particularly involving estrogen—may influence this imbalance, although no single explanation has been confirmed. Genetics also play an important role. Individuals with certain immune-related genes appear to be more prone to the disease, especially when these genes increase the likelihood of autoreactive immune cells.
Current treatments focus on calming the immune system with medications such as corticosteroids, immunosuppressants, or biologics. While these therapies help reduce symptoms, they do not cure the disease because they do not eliminate the underlying trigger. This is why the new findings about EBV are especially meaningful.
How EBV and Lupus May Be Connected
Epstein–Barr virus is best known for causing mononucleosis, though most infections occur in childhood and often go unnoticed. Once in the body, the virus hides inside B cells—immune cells responsible for producing antibodies.
For decades, scientists suspected a link between EBV and lupus, but the exact mechanism remained unclear. Using advanced technology, researchers analyzed hundreds of thousands of immune cells from people with lupus and healthy individuals. They discovered a striking pattern: EBV-infected cells were significantly more common in those with lupus.
More importantly, the virus seemed to preferentially infect a specific type of B cell called an autoreactive B cell. These cells are inherently risky because they can attack the body if activated. EBV appears to “reprogram” them, pushing them from a quiet, dormant state into a highly active one.
This activation sparks a cascade of immune responses. The infected cells release signals that attract additional immune cells, escalating inflammation throughout the body. Over time, this chaotic activity contributes to the unpredictable symptoms characteristic of lupus.
How EBV Alters Immune Behavior
A key player in this process is a viral protein called EBNA2. When EBV infects a B cell, EBNA2 flips on several human genes involved in inflammation. These genes then activate additional pathways, forming an interconnected network of inflammatory responses.
As infected B cells transform, they interact more strongly with helper T cells. These T cells encourage the recruitment of more autoreactive B cells, further expanding the pool of problematic immune cells. Even immune cells that are not infected by the virus respond to these signals, joining the growing wave of inflammation.
Eventually, the immune system becomes overwhelmed by cells that can no longer distinguish between healthy tissue and harmful invaders. This leads to the production of autoantibodies—especially antibodies that target the nucleus of human cells—which is one of the defining features of lupus.
This process illustrates how a normally silent virus can reshape immune function. Although EBV lives harmlessly in most people, under certain circumstances it may nudge the immune system toward autoimmune disease.
Why Only Some People Develop Lupus
If nearly everyone carries EBV, why do only a few develop lupus? Researchers believe the answer lies in several interacting factors.
1. Viral Variations
Not all EBV strains are the same. Some variants may be more capable of altering B cells or triggering immune imbalance.
2. Genetic Susceptibility
Individuals with immune system genes that increase autoreactive B cells have more “vulnerable” cells for EBV to infect. Without these genetic traits, the virus is more likely to remain harmless.
3. Viral Reactivation
Although EBV often remains dormant, it can reactivate periodically. These episodes may trigger bursts of inflammation that push the immune system toward autoimmunity.
4. Lifestyle and Environmental Factors
Chronic stress, hormonal shifts, infections, and other environmental triggers may weaken immune regulation, creating conditions where EBV can exert its influence more strongly.
Researchers believe that lupus emerges when these factors combine in the right (or wrong) way—virus, genes, environment, and immune function intersecting at the perfect moment.
What This Means for Future Treatment
The new findings offer several hopeful possibilities:
• EBV-targeted vaccines:
If EBV plays a direct role in lupus, preventing the infection could reduce the risk of developing autoimmune disease. Several early-phase vaccines are currently in development.
• Removing EBV-infected cells:
Stanford researchers are exploring therapies that specifically eliminate EBV-infected B cells, which may help control lupus without broadly suppressing the immune system.
• Improved diagnostic tools:
New tests that measure EBV activity inside immune cells may help diagnose lupus earlier or predict disease progression more accurately.
• Broader impacts on autoimmune disease research:
Scientists are also examining whether EBV contributes to conditions like multiple sclerosis or rheumatoid arthritis. Understanding these viral connections could pave the way for more targeted, effective therapies across several diseases.
Natural Ways to Support Immune Health
While research moves forward, certain lifestyle habits can help support overall immune balance. These strategies do not cure lupus, but they may enhance well-being and complement medical treatment.
Stress Management:
Chronic stress disrupts immune function and can worsen inflammation. Gentle yoga, deep breathing, meditation, or even short daily walks can help calm the body.
Adequate Sleep:
Seven to nine hours of restful sleep each night strengthens immune resilience. Maintaining consistent sleep routines and limiting screen time before bed can improve sleep quality.
Balanced Nutrition:
A diet rich in whole foods—fruits, vegetables, lean proteins, and healthy fats—supports immune regulation. Omega-3 fatty acids found in fish, walnuts, and flaxseeds may help reduce inflammation.
Gut Health:
Fermented foods like yogurt, kefir, or kimchi add beneficial bacteria to the digestive system. Fiber from vegetables and whole grains nourishes these microbes, supporting immune function.
Regular Physical Activity:
Low-impact exercises such as walking, stretching, or swimming can boost energy, improve mood, and support metabolic and immune health.
These practices, while simple, can help create a stronger foundation for overall wellness.
Looking Ahead With Knowledge and Optimism
The discovery that EBV can reshape immune cells in ways that resemble lupus marks an important step forward in understanding this complex disease. It provides scientific clarity, showing that lupus is not random or mysterious but rooted in identifiable biological processes.
For patients and families, this insight brings reassurance and a better sense of what is happening inside the body. For researchers, it opens new doors to therapies that address the earliest stages of autoimmune disease rather than merely managing symptoms.
Although much remains to be learned, the link between EBV and lupus brings renewed hope. As research continues, vaccines, targeted therapies, and improved diagnostics may one day transform how lupus is prevented, detected, and treated. With each discovery, the path toward long-term relief and better quality of life becomes more promising than ever.
News in the same category


Stop Counting Calories — The “100g Protein Rule” That Boosts Energy and Crushes Cravings

10 Supplement Combinations You Should Never Take Together
🦴 This Could Be the Vitamin Your Body Is Missing When Your Legs and Bones Hurt

Goosegrass (Eleusine indica) and Stomach Pain: Can It Help or Hurt? The Complete Guide
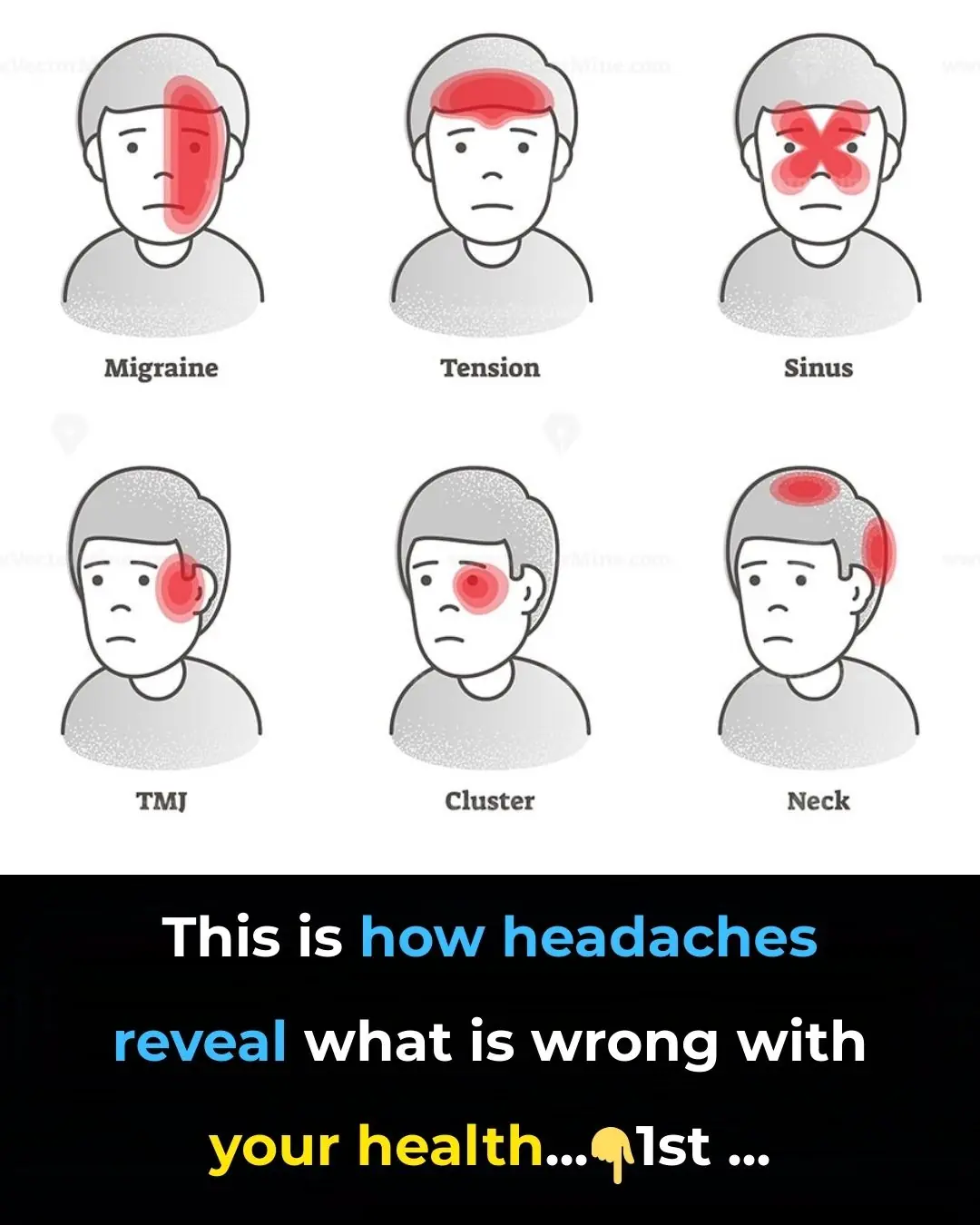
This is How Headaches Reveal What is Wrong With Your Health

The natural kitchen mix people use to break down stubborn plaque buildup
10 Amazing Health Benefits of Dates (and Why You Need To Start Eating Them!)

The Surprising Truth: Wooden Boards Kill Bacteria Better Than Plastic

Cell Therapy Begins Human Trials to Reverse Spinal Cord Injury
Overripe Bananas Could Help Fight Cancer Naturally

Chinese Scientists Created a ‘Bone Glue’ That Repairs Fractures in Minutes With a Single Injection
Castor Oil for Peripheral Neuropathy Relief: A Natural Remedy Worth Trying?
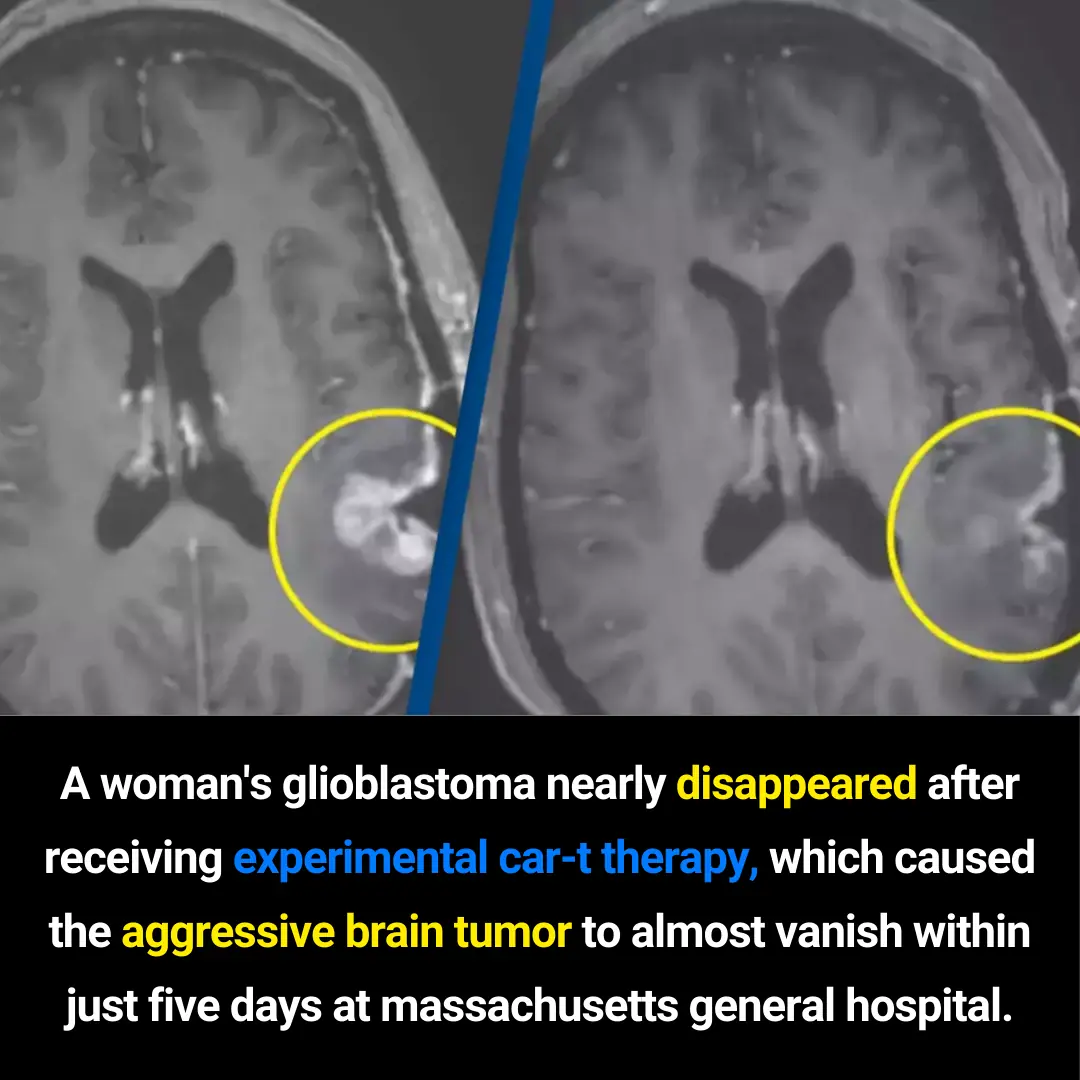
The New Science Behind Killing Cancer

Beware: U.S Salmon May be Crawling with Japanese Tapeworm, Say Scientists
How to Use Guava for Eye Comfort | Natural Remedies for Healthy Eyes

Top 10 foods that improve blood circulation in legs

Orthopedist’s Secret: How to Support Natural Cartilage Repair in Just 24 Hours
15 visible signs of low thyroid you can see – don’t ignore #7!
News Post
Meet the First Woman Graduate From Howard University Law School, Charlotte E. Ray
Beating Seasonal Depression: 8 Directories To Help You Find An Affordable Black Therapist

Hip-Hop Pioneer Rakim Launches New ‘Notes’ Fintech Platform to Empower Independent Artists
New ‘Eddie’ Documentary About Comedy Legend Eddie Murphy Is Coming to Netflix
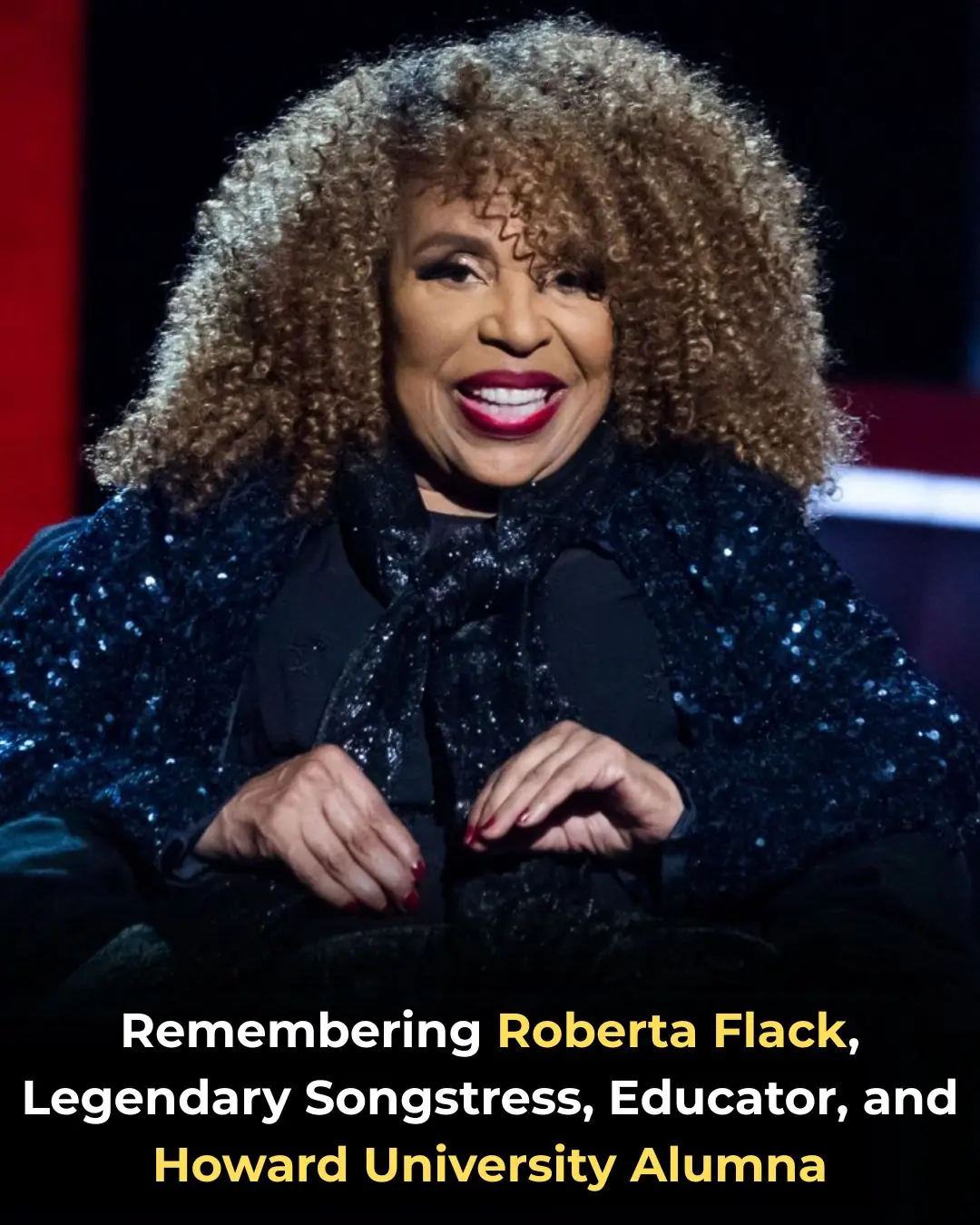
Remembering Roberta Flack, Legendary Songstress, Educator, and Howard University Alumna

New CBS Show ‘The Gates’ Marks Return of Predominantly Black Cast to Daytime Soaps for First Time in Three Decades

4 Inspiring Things You Never Learned About W.E.B. Du Bois

6 Inspiring Achievements That Black Women Accomplished First

Afrobeats Star Tems Joins San Diego FC Major League Soccer Ownership Group
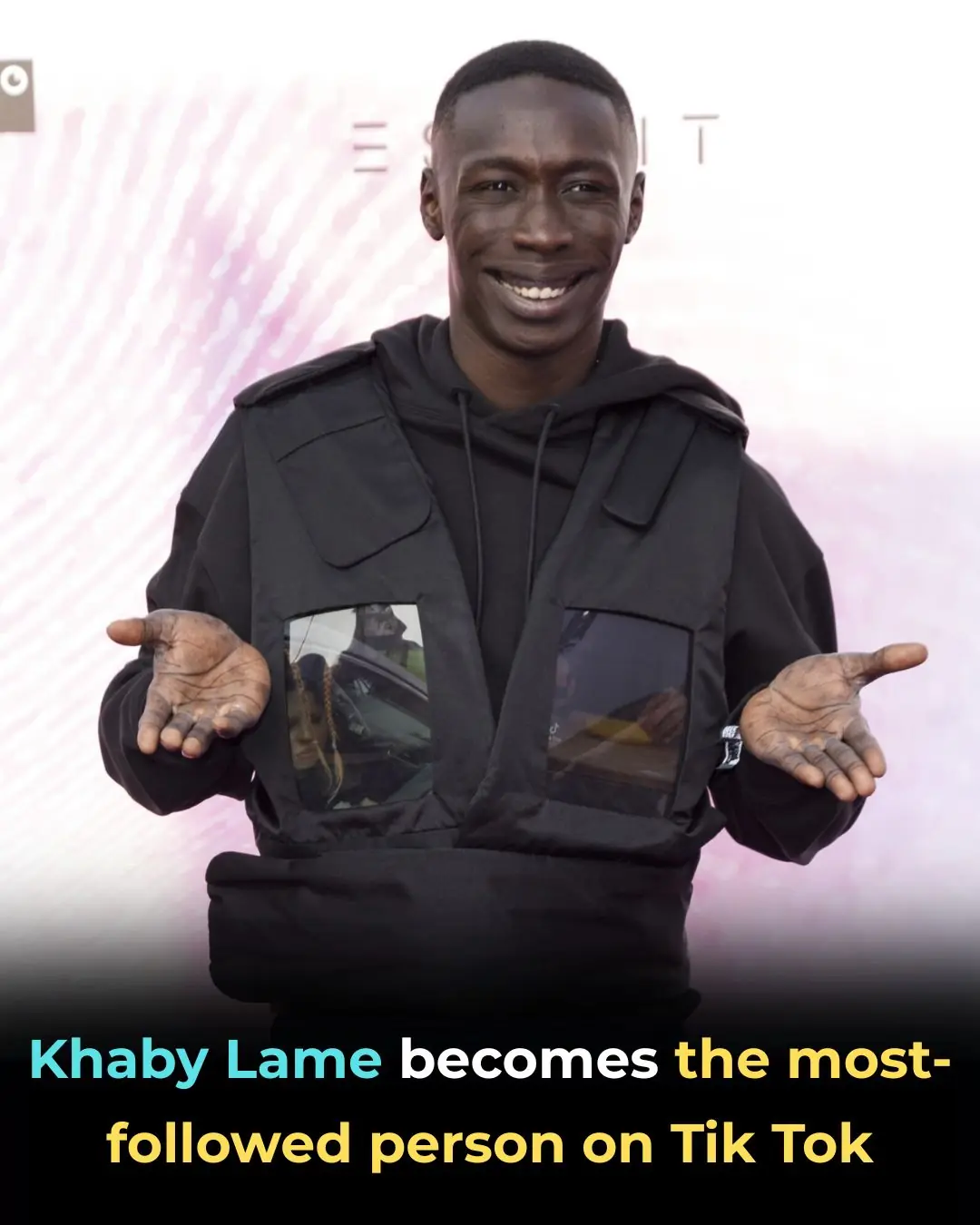
Khaby Lame Becomes The Most-Followed Person On TikTok
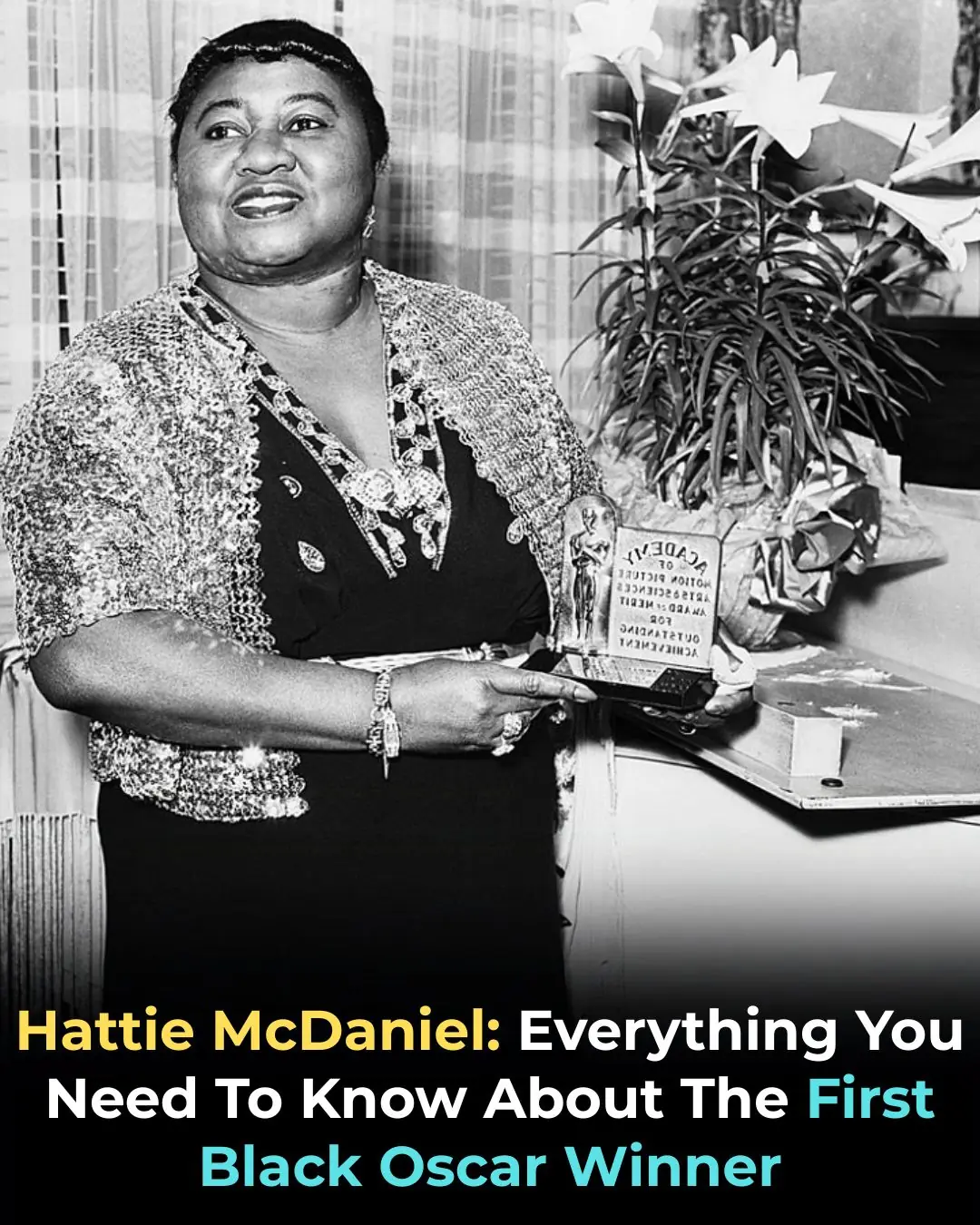
Hattie McDaniel: Everything You Need To Know About The First Black Oscar Winner

40 Years Ago, Michael Jackson’s ‘Thriller’ Album Made History at the Grammys

Raspberry Leaf Power: 30 Benefits and How to Use It

7 Powerful Bay Leaf Benefits for Heart Health and Smoother Blood Flow

Stop Counting Calories — The “100g Protein Rule” That Boosts Energy and Crushes Cravings

How Cats Use Smell and Earth’s Magnetic Field to Navigate Home Over Long Distances

10 Supplement Combinations You Should Never Take Together
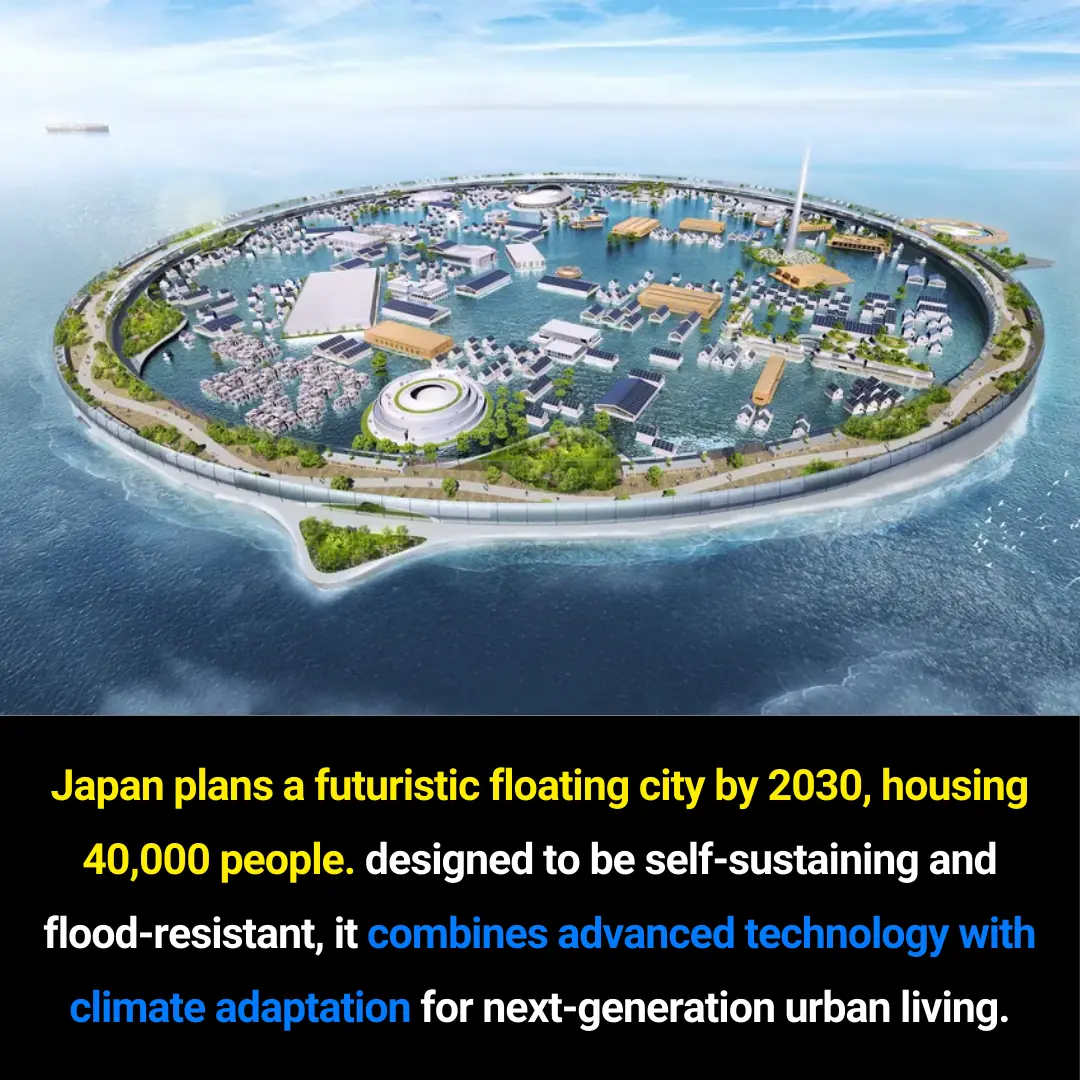
Japan’s Visionary Floating City: A Sustainable Urban Model for 2030 and Beyond
🦴 This Could Be the Vitamin Your Body Is Missing When Your Legs and Bones Hurt