The Link Between Gout and Kidney Disease: What You Need to Know
Gout and kidney disease are far more connected than most people realize. Each condition can aggravate the other, forming a harmful cycle that can be difficult to break without timely care and lifestyle changes. Understanding how they interact is the first step toward protecting both your joints and your kidneys — two vital systems that depend on one another for balance.
1. Understanding Gout and the Role of Uric Acid
Gout is a form of inflammatory arthritis triggered by elevated uric acid levels in the blood, a condition known as hyperuricemia. Normally, the kidneys filter out uric acid — a natural byproduct of breaking down purines, which are found in certain foods and in your body’s own cells.
However, when your body produces too much uric acid or your kidneys can’t excrete it efficiently, uric acid accumulates and crystallizes. These sharp, needle-like crystals lodge in the joints, causing sudden and intense flare-ups characterized by:
-
Severe pain and swelling
-
Redness and warmth around the affected area
-
Most often, inflammation in the big toe joint, but other joints like the ankles, knees, wrists, or fingers can also be affected.
Repeated attacks can lead to chronic joint damage if the underlying uric acid imbalance isn’t corrected.
2. How Gout Can Damage the Kidneys

Gout doesn’t just affect the joints — over time, high uric acid levels can harm the kidneys in several ways:
-
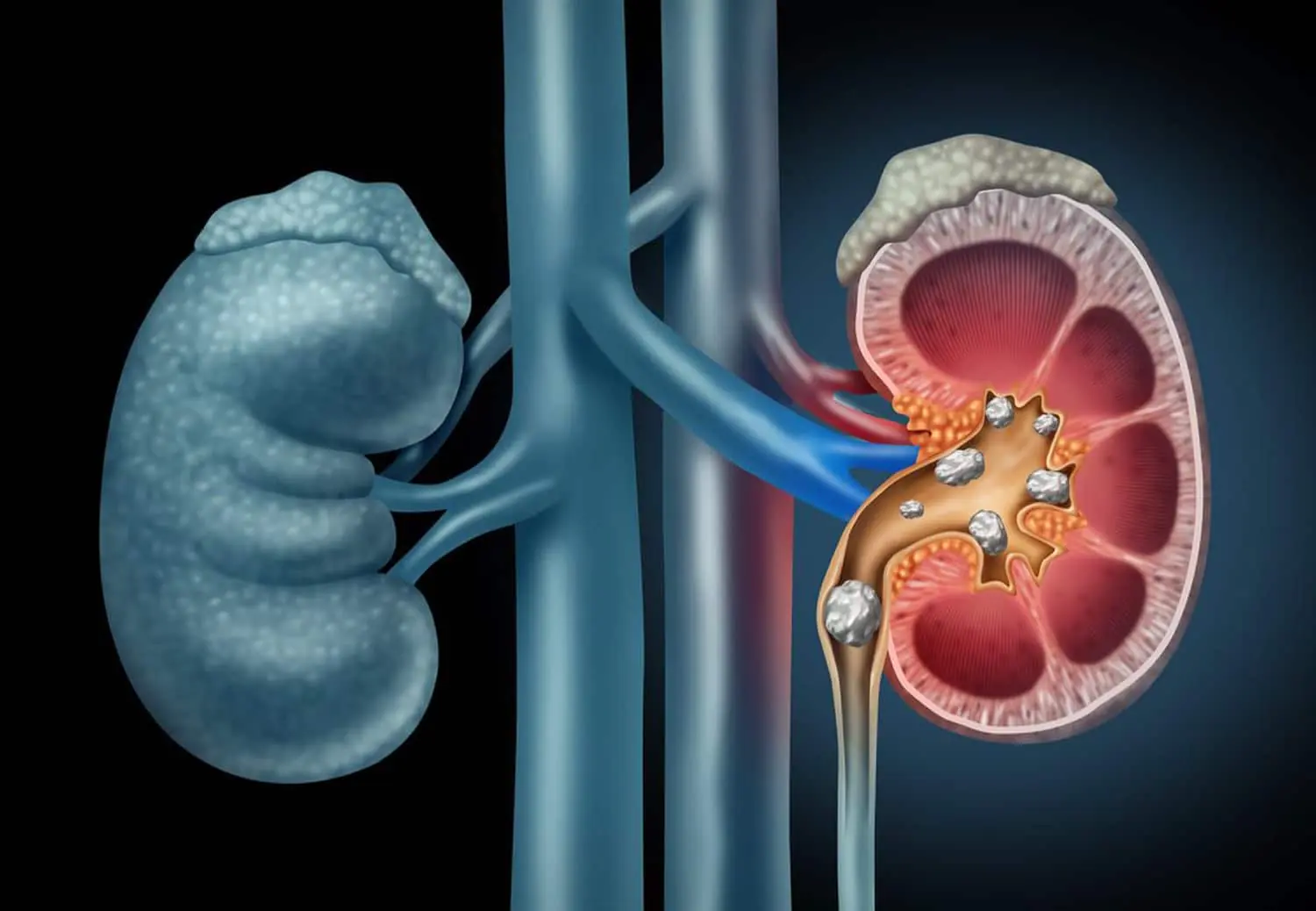
Uric acid kidney stones: Crystals can accumulate in the urinary tract, blocking urine flow and causing severe flank pain. These stones can also increase the risk of urinary infections.
-
Chronic urate nephropathy: Persistent uric acid deposits can scar delicate kidney tissues, gradually reducing their ability to filter waste from the blood.
-
Ongoing inflammation: Frequent gout flares trigger systemic inflammation that can place extra stress on the kidneys and nearby blood vessels.
Even if you don’t experience visible gout symptoms, elevated uric acid levels can quietly cause kidney damage over time.
3. How Kidney Disease Can Trigger Gout
The connection works both ways. When the kidneys are weakened or damaged — as in chronic kidney disease (CKD) — they lose their efficiency in filtering waste, including uric acid. This leads to:
-
Reduced uric acid clearance: Impaired kidney function allows uric acid to build up in the bloodstream.
-
Increased risk of gout flares: Persistent hyperuricemia makes gout attacks more frequent, painful, and difficult to control.
-
Silent uric acid buildup: Even without joint pain, high uric acid can continue to damage kidney tissue, worsening CKD progression.
In fact, studies show that people with kidney disease are several times more likely to develop gout compared to those with healthy kidney function.
4. The Vicious Cycle
When both gout and kidney disease coexist, they create a self-perpetuating loop that accelerates health decline:
Gout increases uric acid → Uric acid harms the kidneys → Damaged kidneys can’t clear uric acid → Uric acid levels rise → More gout attacks and further kidney strain
Breaking this cycle early is essential. Left unchecked, it can lead to advanced CKD, frequent gout flares, and a reduced quality of life.
5. Shared Risk Factors
Several lifestyle and metabolic factors raise the risk of both gout and kidney disease. Addressing them can help manage — and even prevent — both conditions.
Common shared risk factors include:
-
High blood pressure (hypertension)
-
Type 2 diabetes
-
Obesity or being overweight
-
Metabolic syndrome
-
High-purine diets (red meat, organ meats, shellfish, certain fish)
-
Sugary beverages (especially those with high-fructose corn syrup)
-
Excessive alcohol consumption, particularly beer and spirits
Other contributors include dehydration, certain medications (like diuretics), and family history of gout or kidney problems.
6. Managing and Preventing the Connection
If you have gout, kidney disease, or both, you can take proactive steps to manage uric acid levels and protect kidney function:
Medical Management
-
Lower uric acid levels: Medications such as allopurinol or febuxostat can reduce uric acid, but dosages must be carefully adjusted for kidney function.
-
Treat gout flares promptly: Anti-inflammatory medications (like colchicine or corticosteroids) can help control pain and prevent lasting joint damage.
-
Monitor kidney function regularly: Routine blood and urine tests help detect changes early.
Lifestyle Strategies
-
Stay well-hydrated: Adequate water intake helps flush uric acid through urine and prevents crystal formation.
-
Control blood pressure and blood sugar: These are key drivers of both kidney and vascular damage.
-
Maintain a balanced diet: Emphasize fruits, vegetables, whole grains, and low-fat dairy while limiting red meats, processed foods, and sugary drinks.
-
Limit alcohol consumption: Alcohol increases uric acid production and impairs its excretion.
-
Achieve and maintain a healthy weight: Weight loss can lower uric acid and improve kidney health.
Consistency is crucial — small, sustainable changes can make a major difference over time.
7. When to See a Doctor
You should talk to your healthcare provider if you experience:
-
Recurrent gout attacks or new joint pain
-
Swelling in your feet, ankles, or hands
-
Persistent fatigue, changes in urination, or foamy urine (possible kidney issues)
-
High blood pressure that’s difficult to control
Early medical intervention can prevent irreversible kidney damage and reduce the severity of gout.
Bottom Line
Gout and kidney disease are two sides of the same coin, linked through the way the body manages uric acid. If ignored, each condition can worsen the other, leading to chronic pain, kidney failure, or cardiovascular complications.
The good news: with proper management — including lifestyle adjustments, medication when needed, and regular monitoring — you can break the cycle and protect both your joints and kidneys.
Disclaimer: This content is for informational purposes only and should not replace professional medical advice. Always consult your doctor for diagnosis, treatment, or any questions about your health conditions.
News in the same category

The Best Foods to Cleanse and Prevent Clogged Arteries

Capsaicin Stops Heart Attacks And Destroys Cancer Cells
17 Signs Your Body Is Too Acidic And 9 Ways To Quickly Alkalize It
Adrenal fatigue: what it is and 17 all-natural ways to fix it fast

Colon Cleansing With Kefir and Flaxseed Meal
Apple extract kills colon cancer cells better than chemotherapy drug
12 surprising foods that help dissolve blood clots naturally

5 Best Water Benefits You Should Know

The Rise of Kissing Bugs
5 Common Drinks That Can Damage Your Liver Just Like Alcohol

Listen to Your Tongue: 11 Subtle Health Messages It Sends Health June 11, 2025 Updated: June 11, 2025

If your mouth feels dry at night, here are 8 reasons why
Two itchy areas on the body could be a sign of liver cancer — but many people mistake it for an allergy
GOOD NEWS: The U.S. Has Successfully Tested a 'Miracle Drug' That Destroys 70 Types of Cancer

Say Goodbye to Dead Skin on Your Feet with These Simple Natural Remedies

Sleeping Trick? Why Sticking One Foot Out Actually Works

12 Urgent Warning Signs That You’re Not Getting Enough Vitamin D
Top 10 Signs of Kidney Problems You Absolutely Must Be Aware Of
News Post

Lori Loughlin Could Get Nothing From 1997 Prenup That Shields Designer Husband’s $100M Fortune

Willie Flanigan and the Gift of a Simple, Perfect Day.

A Cart Full of Kindness: When a Stranger Paid It Forward.
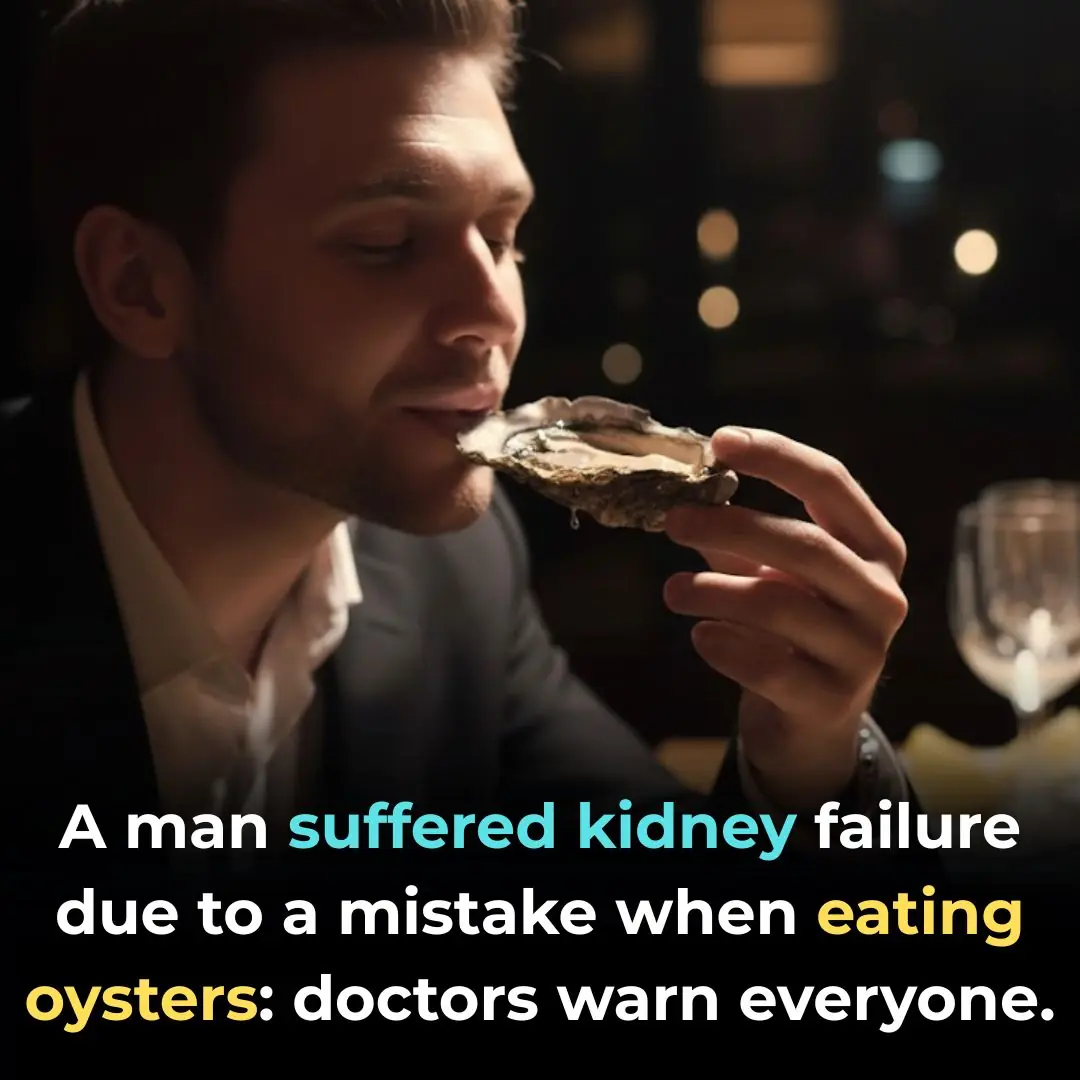
20-Year-Old Man Suffers Acute Kidney Failure After Eating 30 Grilled Oysters — Doctors Reveal the Shocking Cause

Fig Leaves: Surprising Benefits and Uses
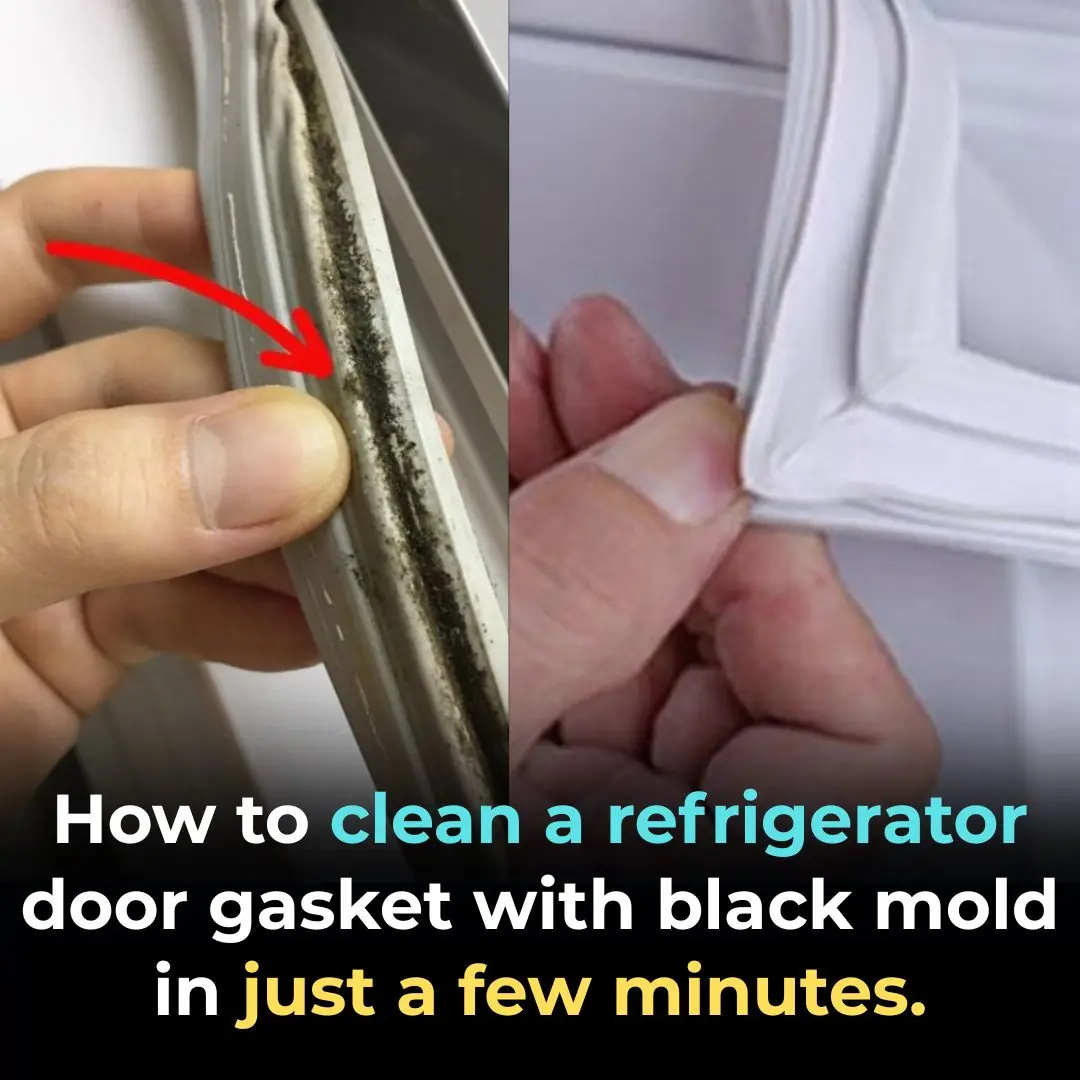
How to Clean Moldy Refrigerator Gaskets — Sparkling Clean in Just 5 Minutes

The Whale That Carried History In Its Neck For Over 100 Years

Denver Bans the Sale of Dogs, Cats, and Rabbits, Paving the Way for More Shelter Adoptions
Medicinal Health Benefits of Turmeric, Curcumin and Turmeric Tea Based on Science

The Best Foods to Cleanse and Prevent Clogged Arteries

Capsaicin Stops Heart Attacks And Destroys Cancer Cells
17 Signs Your Body Is Too Acidic And 9 Ways To Quickly Alkalize It
Adrenal fatigue: what it is and 17 all-natural ways to fix it fast

Colon Cleansing With Kefir and Flaxseed Meal
If you rub these 2 points behind your knees, this is the effect on your body
Apple extract kills colon cancer cells better than chemotherapy drug
12 surprising foods that help dissolve blood clots naturally

Elon Musk's ex Grimes reveals controversial face tattoo she spent 10 years 'emotionally' working up to

Justin Bieber announces 'wild' tech career move that could earn him millions
