
This New Million-Person Study Just Changed What We Know About Cholesterol and Dementia
This New Million-Person Study Just Changed What We Know About Cholesterol and Dementia
Many people worry that lowering their cholesterol—especially with medications like statins—might protect their heart but harm their brain. After all, the brain contains nearly 20% of the body’s cholesterol, a crucial ingredient for neuron structure, synaptic activity, and nerve insulation. With so many mixed messages online, the fear is understandable: Could lowering cholesterol starve the brain of what it needs to function?
A massive new study analyzing over one million people has brought clarity to this debate. Using state-of-the-art genetic methods, researchers have provided the strongest evidence yet that long-term LDL reduction—naturally or through medication—substantially lowers dementia risk. Even better, the study helps explain why short-term clinical trials haven’t always reflected this benefit.
This article breaks down the science behind cholesterol and brain health, what the new research means for you, and practical steps anyone can take to protect cognitive function for life.

Key Takeaways
1. Your Brain Makes Its Own Cholesterol
Reducing blood cholesterol doesn’t reduce brain cholesterol—because the brain synthesizes its own supply behind the blood–brain barrier.
2. Statins Appear Protective Long-Term
Short trials show mixed results, but long-term genetic and observational analyses indicate significantly reduced dementia risk among long-term users.
3. Midlife Is the Critical Window
Cholesterol levels in your 40s and 50s are far more strongly linked to dementia risk than cholesterol levels in older age.
4. Dementia Prevention Requires a Holistic Approach
Key modifiable factors include blood pressure, diabetes, exercise, hearing, vision, cognitive activity, and mental health.
1. The Cholesterol Conundrum: Friend or Foe to Your Brain?
A central misconception is that reducing dietary or blood cholesterol lowers cholesterol inside the brain. In reality, the two systems are isolated. Cholesterol does not cross the blood–brain barrier, and almost all brain cholesterol is manufactured locally by astrocytes and oligodendrocytes.
Why this matters
-
Diet-induced or medication-induced low blood cholesterol cannot starve the brain.
-
Brain cholesterol turnover is extremely slow—lasting up to 5 years—because it is tightly regulated for stability.
Reference: Björkhem et al., Nat Rev Neurol, 2013.
Thus, lifestyle changes that lower LDL are brain-safe. Concerns arise only when medications might cross the blood–brain barrier—leading to…
2. Statins and Your Brain: Clearing Up the Confusion
Some statins are fat-soluble (lipophilic), meaning they can cross the blood–brain barrier more easily. Early anecdotal reports described reversible memory problems in some users, creating public anxiety.
But what does high-quality evidence show?
Randomized Controlled Trials (RCTs):
-
PROSPER Trial (2002, 5,804 participants)
Found no significant difference in cognitive decline between pravastatin and placebo.
Reference: Shepherd et al., Lancet. -
Evolocumab + Statins (FOURIER Cognitive Substudy, 2017)
Achieving extremely low LDL (<30 mg/dL) did not impair cognition.
Reference: Giugliano et al., NEJM. -
Alirocumab + Statins (ODYSSEY trials, 2020)
Same conclusion: no cognitive harm.
Reference: Robinson et al., Am J Cardiol.
Across RCTs, statins do not harm memory or cognition.
3. Can Lowering Cholesterol Actually Prevent Dementia?
Here the data get compelling.
Observational Evidence
A sweeping meta-analysis of 55 studies (7+ million people) found:
-
14% lower dementia risk among statin users overall
-
63% lower risk among those taking statins longer than 3 years
(Poly et al., Prev Chronic Dis, 2020)
These numbers are far too large to ignore.
Why might LDL reduction protect the brain?
-
Vascular dementia prevention
LDL drives arterial plaque formation, including in brain-supplying arteries.
Reference: Arvanitakis et al., Lancet Neurology, 2016. -
Alzheimer’s risk reduction
LDL-related vascular damage accelerates amyloid deposition.
Reference: Iturria-Medina et al., Nat Commun, 2016. -
Anti-inflammatory effects
Statins reduce neuroinflammation—a major contributor to dementia progression. -
Antioxidant and endothelial benefits
Improved blood flow means better oxygen delivery to the brain.
These effects take years or decades to build—which explains the mismatch with short-term trials.
4. So Why Don’t Randomized Trials Show Reduced Dementia?
A major 2023 meta-analysis of 20 RCTs (100,000+ participants) found no short-term dementia reduction.
But there’s a simple reason:
Clinical trials follow patients for too short a period.
Most RCTs:
-
last 2 to 5 years
-
study older adults
-
begin treatment long after vascular damage has accumulated
Yet we know from brain pathology research that dementia is a 20–40 year process.
Evidence:
-
High LDL at age 40–55 strongly predicts dementia after age 70.
Reference: Solomon et al., JAMA Neurology, 2017. -
Lowering LDL late in life may be too late to meaningfully alter long-term trajectory.
5. The Breakthrough: What a Million-Person Mendelian Randomization Study Revealed
Mendelian randomization (MR) uses natural genetic differences to mimic the effect of lifelong LDL reduction. It’s like running a lifetime clinical trial without giving anyone drugs.
This massive 2024–2025 MR study found:
-
Genes mimicking the lifelong effect of statins → 76% lower dementia risk
-
Genes mimicking ezetimibe → 82% lower dementia risk
These results are remarkably strong and minimize lifestyle confounders.
Key implication:
Long-term LDL lowering—whether by genes or medication—appears highly protective.
Referenced in: Ference et al., JAMA, 2017; updated MR analyses through 2024.
6. Beyond Cholesterol: 4 Hidden Dementia Risk Factors You Can Control
The Lancet Commission (2020, 2023 updates) identified modifiable risk factors that could prevent up to 40% of dementia cases.
1. Cognitive Stimulation
-
Mentally stimulating work lowers dementia risk.
Wu et al., BMJ, 2021.
2. Hearing Loss (One of the strongest modifiable risks)
-
Untreated hearing loss → 2.4× higher dementia risk
Lin et al., Lancet Neurology, 2020. -
Using hearing aids reduces risk significantly
Livingston et al., Lancet, 2020.
3. Poor Vision
-
Visual impairment → 47% higher dementia risk
Zhang et al., Acta Ophthalmologica, 2021.
4. Depression & Social Isolation
-
Midlife depression doubles dementia risk
Kuring et al., Psychological Medicine, 2020. -
Treating depression reduces risk by ~30%
Gimson et al., Transl Psychiatry, 2018.
7. Promising Supplements for Brain Health (Evidence-Backed)
1. Multivitamins
Large RCTs (COSMOS-Mind, 2022 & 2023):
-
Daily multivitamin improved global cognition
-
Equivalent to 2 years younger brain age
2. Creatine
Meta-analysis (Avgerinos et al., Psychopharmacology, 2022):
-
Improved memory and cognitive processing, especially in older adults.
3. TMG (Trimethylglycine)
-
Lowers homocysteine, a known dementia risk factor
-
Supports methylation and neuronal health
Ref: Schwab et al., Am J Clin Nutr, 2002.
Always consult a clinician before starting supplements.
Conclusion
The cholesterol–dementia debate is shifting decisively. The largest genetic study to date shows that lifelong LDL reduction is strongly protective, aligning with decades of vascular and Alzheimer’s research.
But protecting your brain isn’t about cholesterol alone. The most powerful strategy is a multi-factor approach:
-
Manage LDL cholesterol (especially in midlife)
-
Control blood pressure
-
Treat hearing and vision problems
-
Challenge your mind
-
Stay physically active
-
Maintain social connections
-
Address depression early
-
Support brain health with evidence-based nutrition and supplements
By taking these steps—starting as early as possible—you’re investing in a stronger, more resilient brain for decades to come.
News in the same category

How to Survive a Heart Attack When You’re Alone: Immediate Steps You Must Take

This 30-Second Chair Test Reveals if Your Legs Are Aging Faster Than You Think
The #1 plant to eliminate mucus and phlegm instantly (how to use it!)
12 warning signs of heart failure you should never ignore
7 Nighttime Signs of Diabetes + 8 Tips to Avoid Blood Sugar Spikes Without Cutting Carbs!

All lupus cases may be linked to a common virus, study finds

Take this one shot and watch what happens to your blood pressure
Take just 1 a day for strong bones, pain-free joints & osteoporosis protection!
Can a Common Kitchen Spice Help Prevent Type 2 Diabetes? New Research Raises Big Questions

Garlic Clove Oil: The Homemade Remedy That Transformed My Mother’s Chronic Leg Pain
Doctors prescribe LEVOTHYROXINE—but here’s what they don’t tell you

The #1 vitamin that can eliminate varicose veins—see how it fixes venous insufficiency!

7 nutrients that actually repair nerves

The Forbidden 6-Ingredient Nightcap That Melts Belly Fat While You Sleep and Rewires Immunity Before Breakfast
Super good vegetable for the liver, the elderly and middle-aged people must eat

Don’t ignore this heart test—it might save your life!
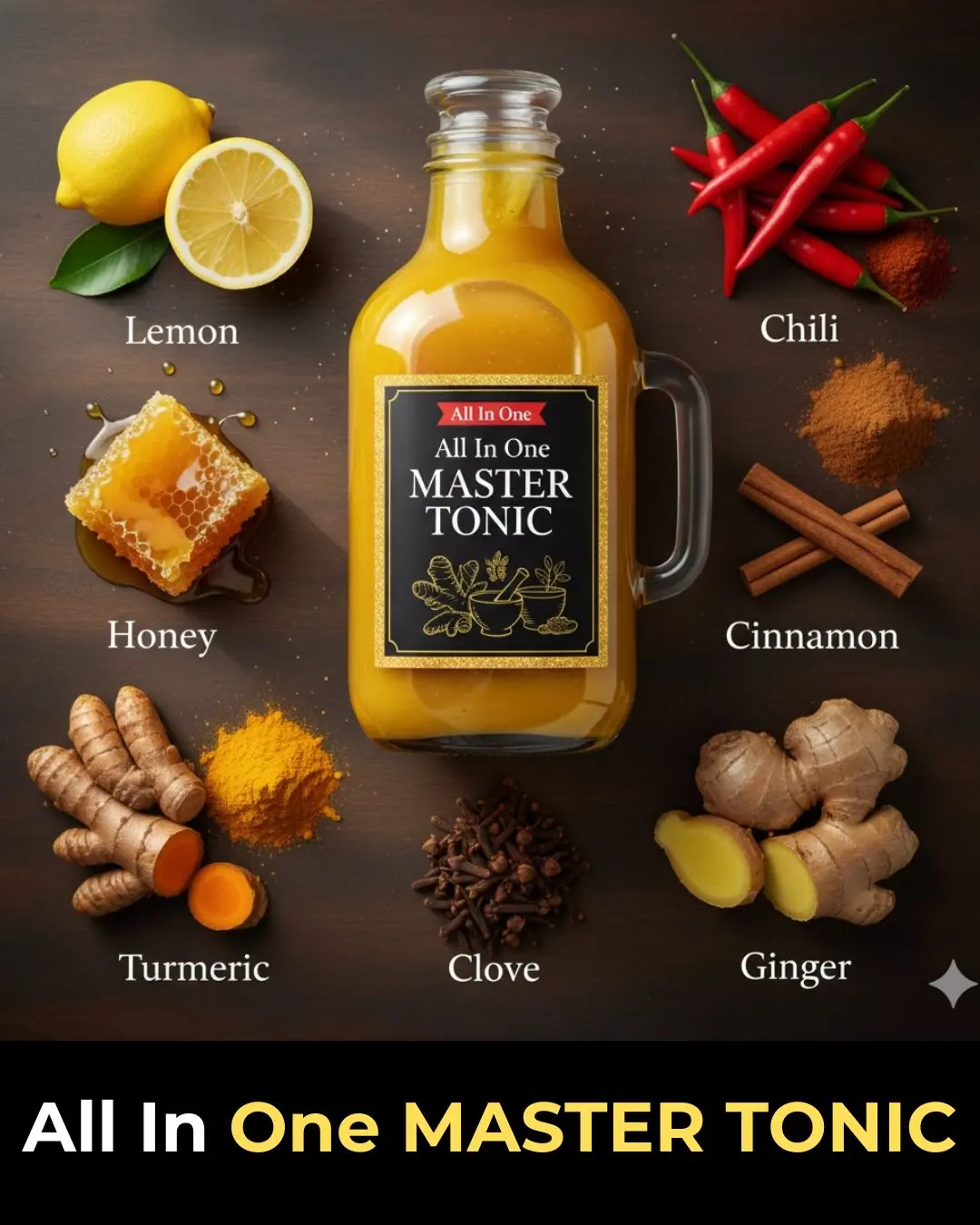
The Forbidden Elixir Big Pharma Hopes You Never Discover: Master Tonic – One Daily Shot to Bulletproof Your Immunity and Ignite Lifelong Vitality!
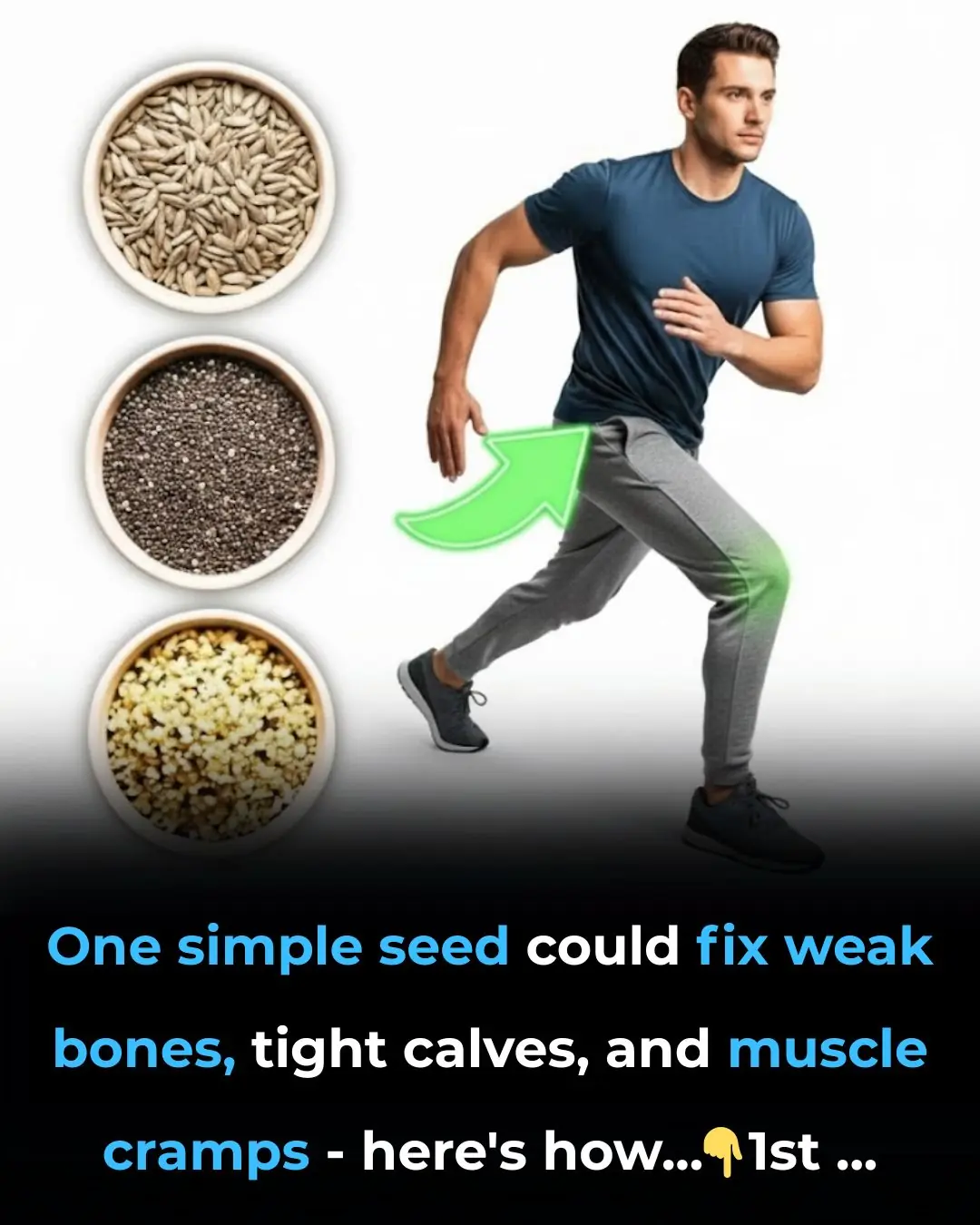
The #1 seed that makes bones & muscles strong—how to use it!
News Post
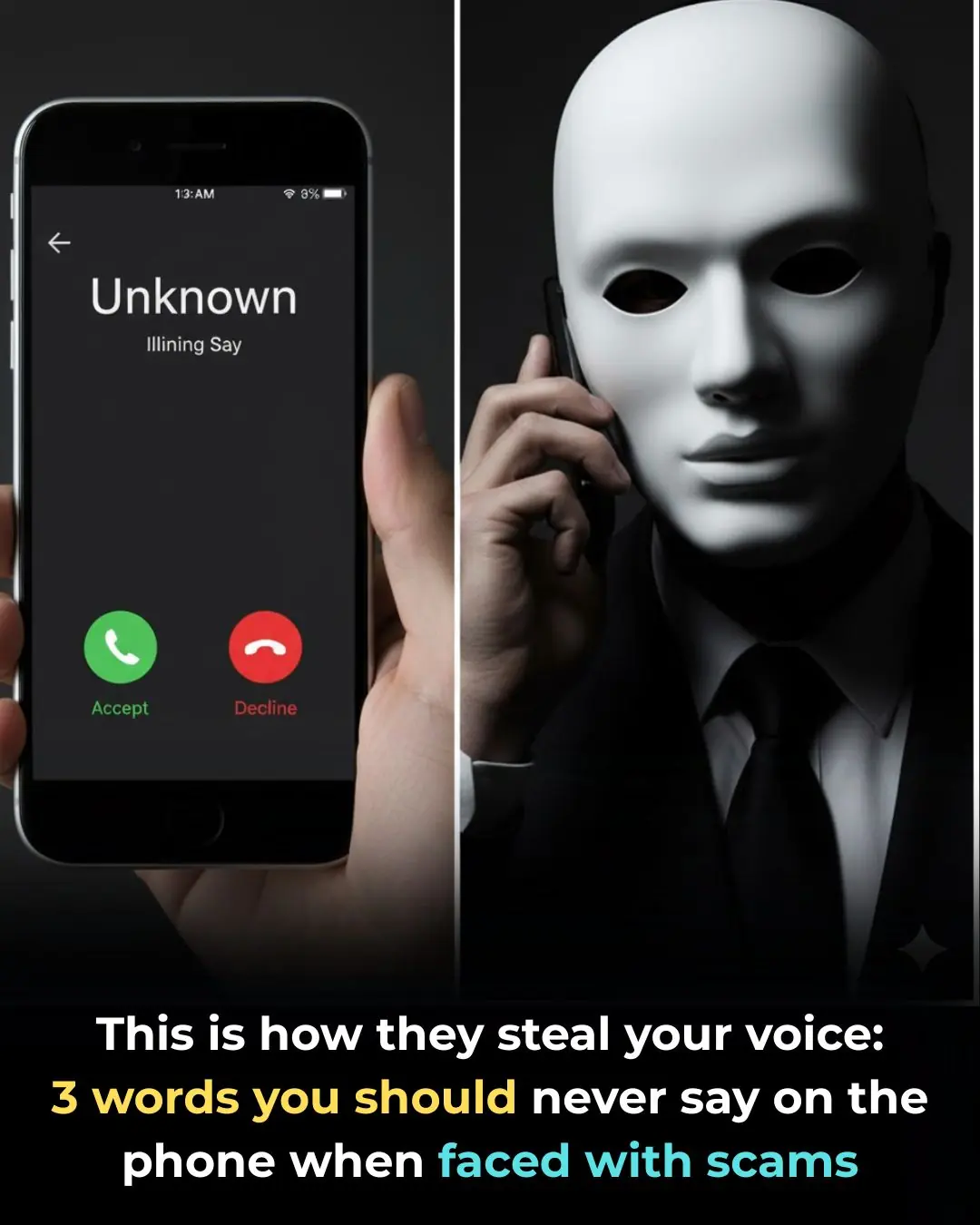
This Simple Word Could Let Scammers Clone Your Voice with AI

Here's why you have cramps at night and how to avoid them

11 Unusual Floor-Cleaning Hacks You’ve Probably Never Heard Of

I Had No Idea About This

12 Strange but Surprisingly Smart Ways to Use Aluminum Foil at Home
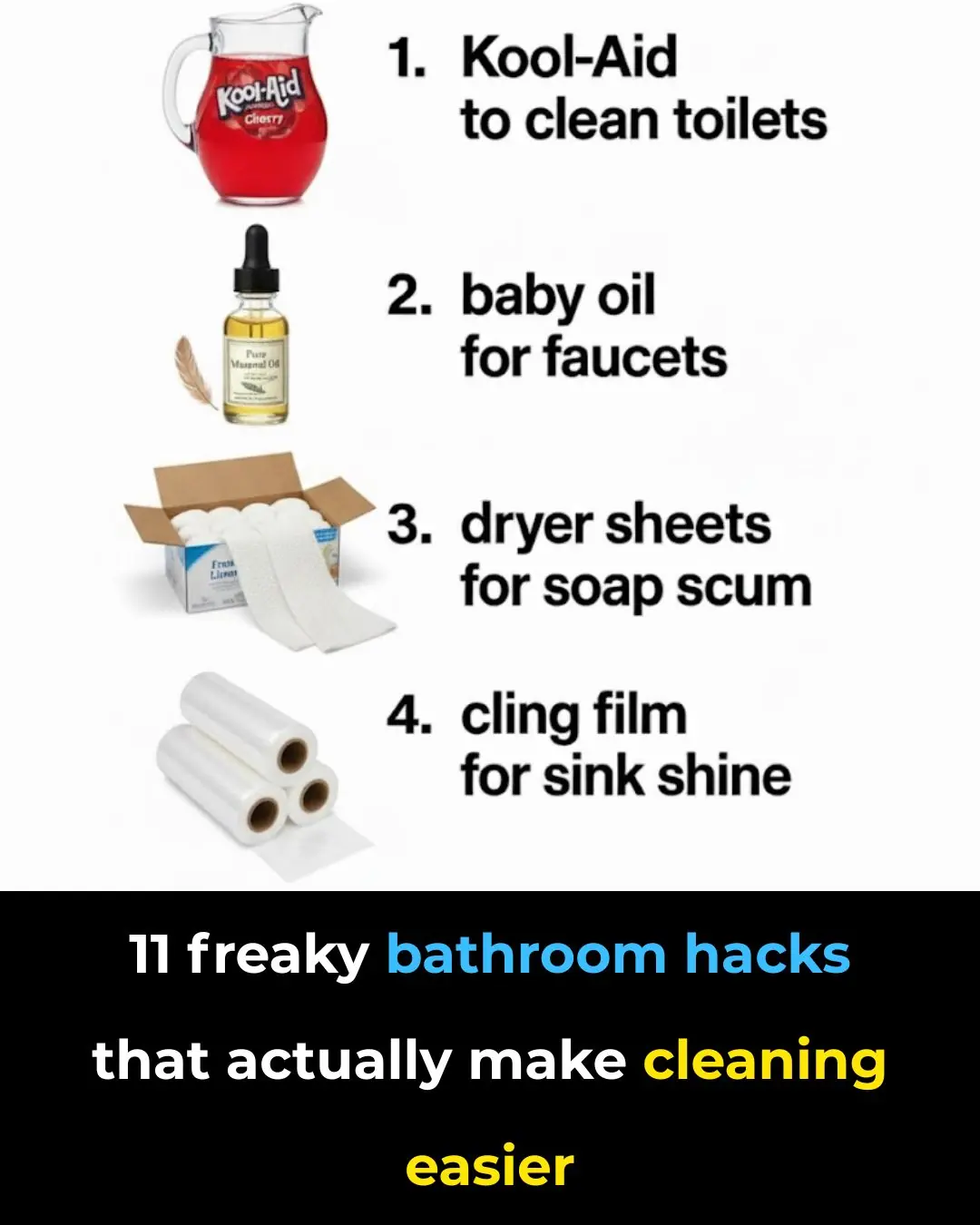
11 Weird Bathroom Hacks That Actually Make Cleaning Easier
10 Weird Microwave Tricks That Make Cleaning Shockingly Easy

NYC Meltdown: Top Restaurateurs Flee City After Mayor-Elect’s ‘Radical’ Policies

Lady Puts a Cup of Vinegar in the Microwave — and the Reason Is Brilliant
10 Unusual Dishwasher Hacks That Have Nothing to Do With Dishes

I Had No Idea This Was a Thing

Deleted Photos, Secret Requests: Inside Meghan & Harry’s Blow-Up With the Kardashians

Wendy Williams’ New Brain Test Results CHANGE EVERYTHING — Guardianship Could Collapse

3 Natural Ways to Relieve Acid Reflux Fast

Heartbreaking: Kirsty Gallacher Confirms Her Brain Tumour Has Rapidly Grown Amid Court Battle

Millie Gibson Drops Bombshell About The Forsytes Season 2 — Fans Didn’t See This Coming
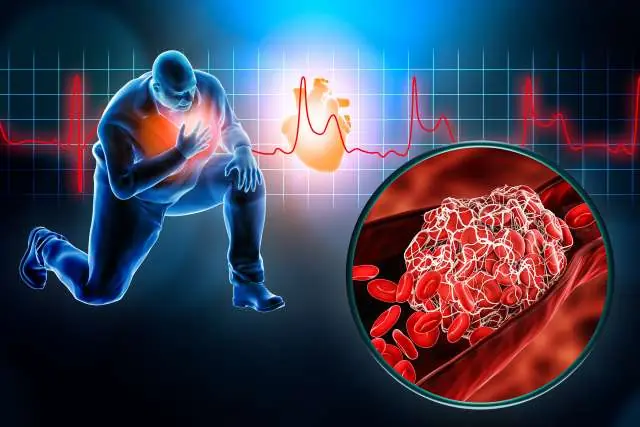
How to Survive a Heart Attack When You’re Alone: Immediate Steps You Must Take

Deal or No Deal Chaos: Sonya’s Game Collapses — Then She Drops a Heart-Stopping Family Reveal
