13 Early Warning Signs of Lupus You Need to Know (And What To Do The Moment You See Them)

Lupus: A Silent Battle Affecting Millions
For many people, lupus may sound like a distant medical term, almost like a condition they will never have to face. But for the 1.5 million Americans currently living with it, lupus is a harsh reality that shapes their daily lives. This chronic autoimmune disease has no known cure, making it both physically and emotionally challenging. Yet, thanks to modern medicine, there are various treatments available to help manage the symptoms, reduce flare-ups, and improve quality of life.
Statistics show that lupus disproportionately affects women—nine out of ten diagnosed cases are female, with the majority of symptoms appearing between the ages of 15 and 45. This highlights not only the gendered impact of the disease but also the fact that it often strikes during the most active years of a person’s life, affecting career, family, and social responsibilities.
What Exactly Is Lupus?
Lupus is classified as an autoimmune disease, meaning the body’s own immune system, which is supposed to defend against viruses and harmful bacteria, mistakenly turns against itself. Instead of protecting, it begins to attack healthy tissues and organs, causing widespread inflammation and damage.
The onset of lupus is usually a combination of factors—genetic predisposition, hormonal imbalance, environmental triggers, and immune system dysfunction. Certain medications, infections, or even long-term hormonal changes can also contribute to the development of the disease.
The Main Types of Lupus
There are several forms of lupus, but the two most common are:
-
Discoid Lupus Erythematosus (DLE): This primarily affects the skin, particularly areas exposed to sunlight, and can cause rashes, lesions, and scarring.
-
Systemic Lupus Erythematosus (SLE): The most serious and widespread form, affecting not only the skin but also vital internal organs and connective tissues.
Systemic lupus can damage joints, muscles, lungs, heart, kidneys, and even the brain, making it a potentially life-threatening condition if not properly managed. In severe cases, it has been linked to kidney disease, cardiovascular complications, and neurological issues such as seizures or cognitive decline.
Living With Lupus: Triggers and Management
Since lupus cannot yet be cured, the primary focus of treatment is on symptom management and avoiding triggers. Flare-ups—sudden episodes when symptoms worsen—can be set off by sunlight, certain medications, and infections. Other contributing factors include stress, rapid changes in temperature, and inflammatory foods, all of which can make the disease more difficult to control.
To manage these risks, doctors often prescribe medications such as:
-
Anti-inflammatory drugs to reduce pain and swelling.
-
Immunosuppressants to calm the overactive immune response.
-
Chemotherapy agents (in lower doses) to control severe cases.
Beyond these, patients may also receive diuretics, antihypertensive drugs, antibiotics, anticonvulsants, or bone-strengthening medications to manage complications linked to organ damage or long-term side effects.
A Team-Based Approach
Because lupus can affect so many different parts of the body, patients are often cared for by a team of specialists, including rheumatologists, cardiologists, nephrologists, neurologists, and gastroenterologists. This collaborative care helps reduce the risk of long-term damage and ensures that the disease’s multiple complications are monitored closely.
Final Thoughts
Lupus is far more than a skin rash or occasional joint pain—it is a complex, lifelong battle that affects the body on multiple levels. While a cure has yet to be discovered, advances in treatment options have given patients the ability to live longer, healthier lives with proper care. By recognizing triggers, following medical advice, and working closely with specialists, those living with lupus can take proactive steps to control flare-ups and protect their long-term health.
News in the same category
The #1 habit that’s destroying muscle in older a:dults—are you doing this?

Vaping vs. Smoking: New Study Says Vapes May Be More Harmful
Waking Up to Pee? Here’s What You Should Know—and When It Might Be a Problem

Girl, 5, died days after being misdiagnosed with a cold
Heart surgeon shares four daily habits to avoid for better health
Top 10 foods that unclog arteries naturally and prevent heart attack

10 Warning Signs You’re Eating Too Much Sugar – Many People Ignore #5
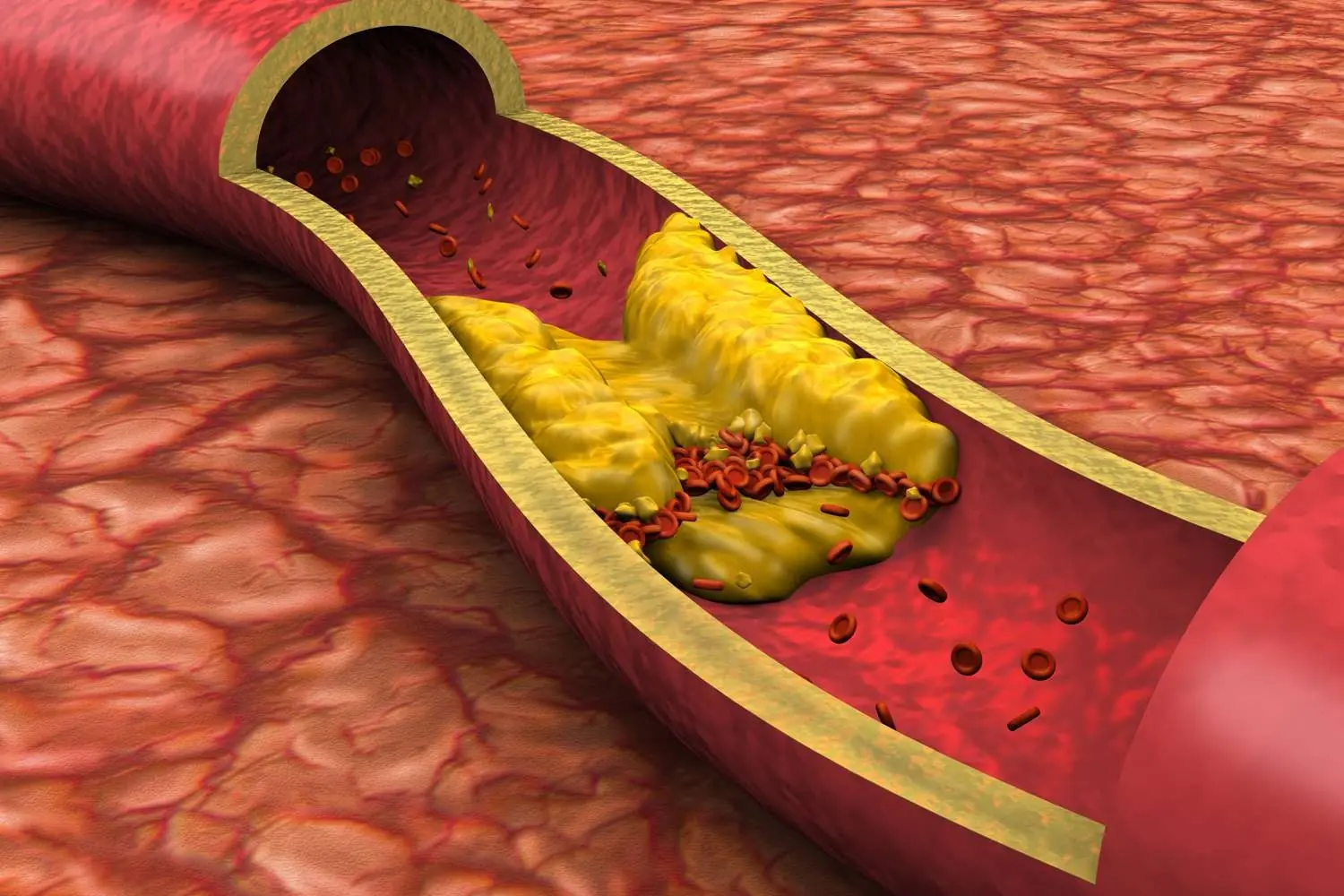
Clogged Arteries Mean Poor Blood Circulation and Risks of Heart Attacks. Here is How You Can Clean Your Arteries from Plaque

Get Rid of Throat Mucus Faster With These Simple Natural Treatments That Work
Scientists Have Discovered Hidden Brain Patterns That May Predict Your Intelligence
One Vitamin That Could Transform Your Circulation

Why Cold Showers on Hot Summer Nights May Keep You Awake

Lesser-Known Menopause Symptoms

Signs Your Cortisol Is Dangerously High

He Never Drank Alcohol but Died of Liver Failure: Doctors Reveal 4 Common Foods That Quietly Destroy the Liver
A man who stayed away from alcohol his entire life shocked his family when he was diagnosed with liver failure and passed away at just 55 years old. Doctors warn that alcohol is not the only enemy of the liver—certain everyday foods can be just as destr
Vitamin D Overdose: When Good Intentions Turn Toxic
Vitamin D is often celebrated as the “sunshine vitamin,” vital for bone strength, immune health, and even protection against certain chronic diseases. But while moderate amounts are essential, excessive or unsupervised intake can be toxic—and in som

6 Types of Pain You Shouldn’t Ignore
Occasional mild discomfort may not require urgent care, but sudden, unexplained, or severe pain always deserves medical attention.

Scrolling on the Toilet? Experts Warn It Could Trigger Painful Hemorrhoids
For many, the bathroom has become more than a necessity—it’s a private escape, a brief pause in the day, and for some, even a mini reading lounge. But researchers warn that lingering too long with your smartphone on the toilet may quietly be raising y
News Post
7 Surprising Benefits of Euphorbia Hirta
Purslane: The Superfood That Tastes Better Than Meat – 7 Reasons to Grow It in Your Garden
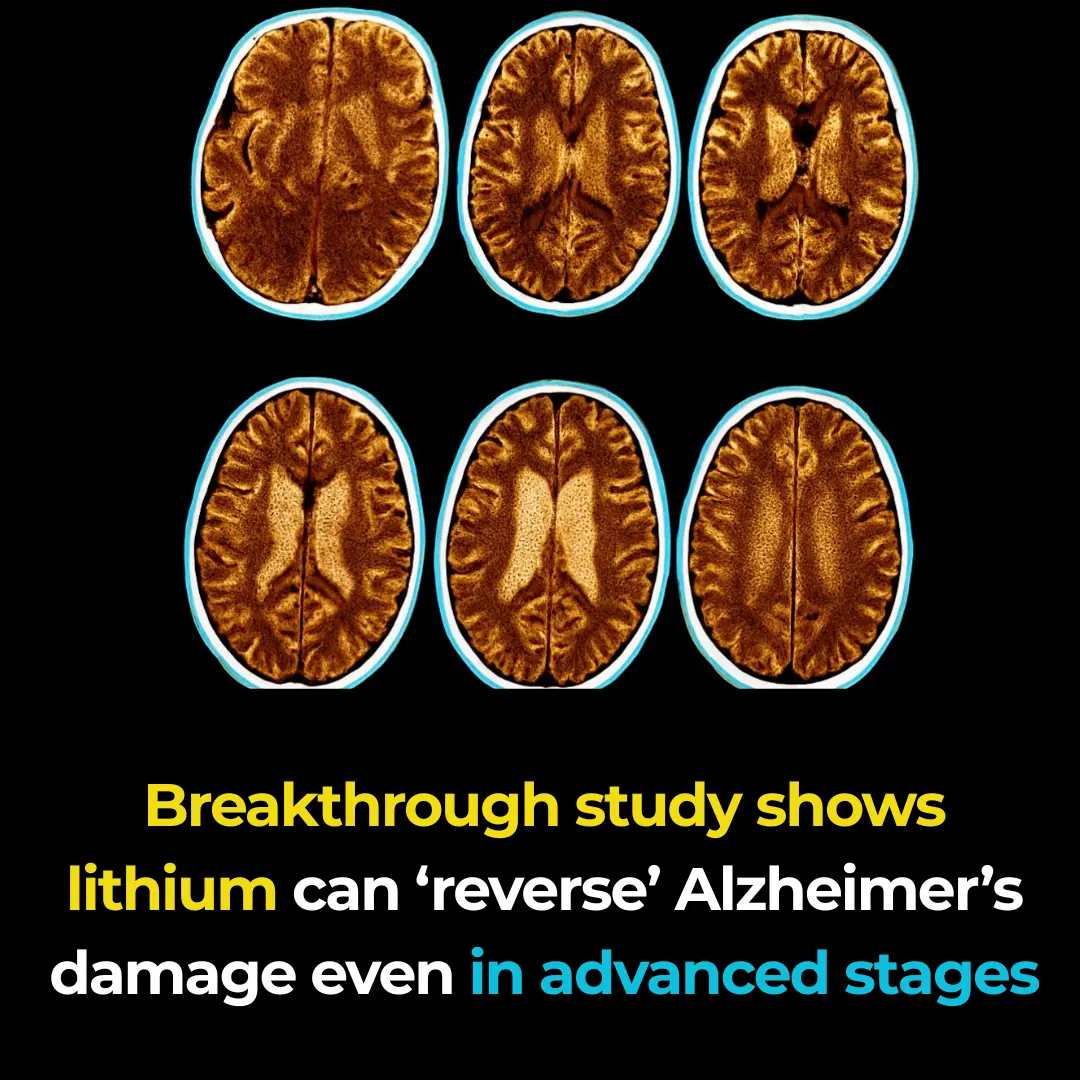
Breakthrough study shows lithium can ‘reverse’ Alzheimer’s damage even in advanced stages
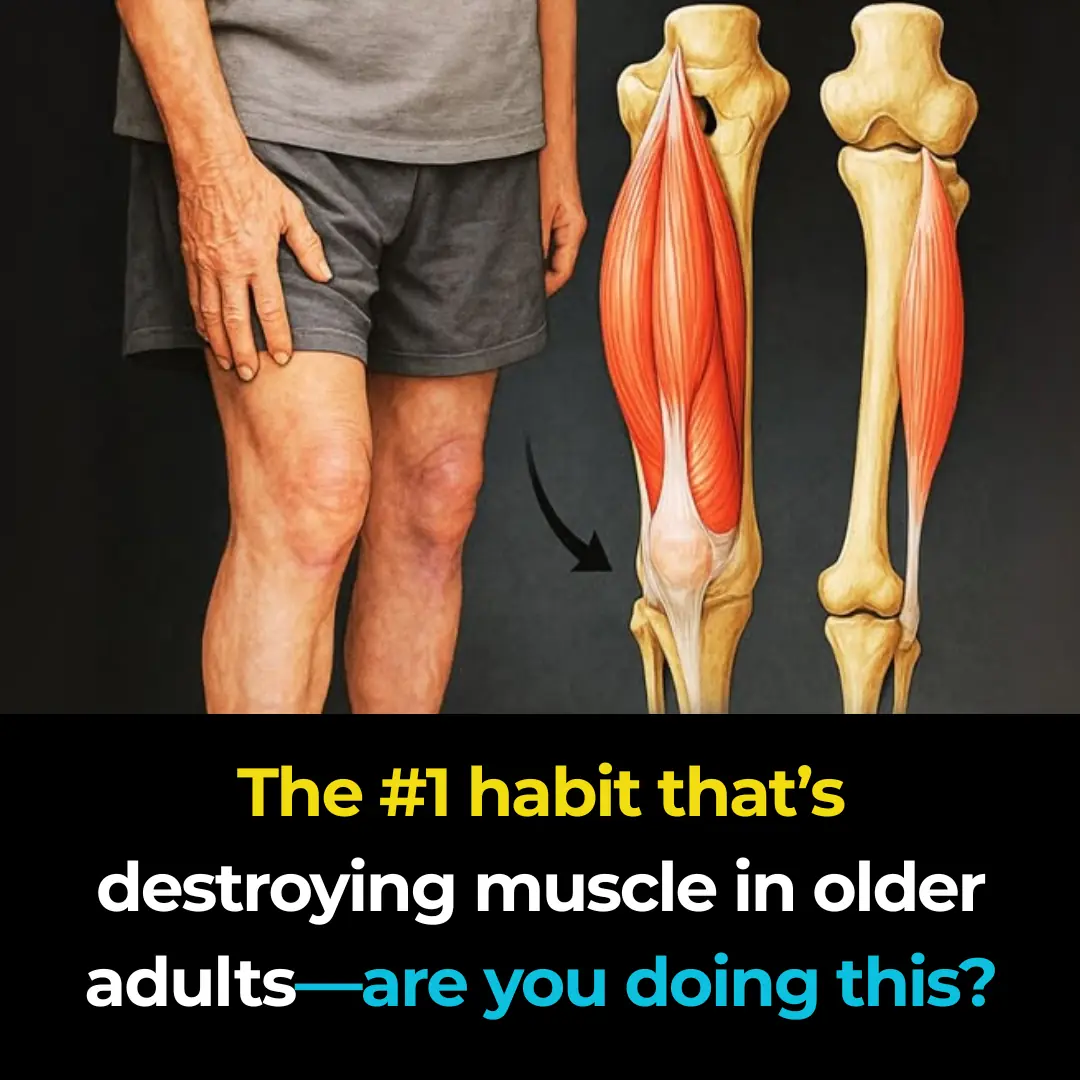
The #1 habit that’s destroying muscle in older a:dults—are you doing this?

2 quick and easy ways to wash yellowed pillow inserts, making them instantly white and fresh like new

When buying luffa, should you choose dark green or light green ones? Even after years of going to the market, many people still don’t know this

Insert this into a lemon and place it in the corner of your house — mosquitoes will be gone for good
Jar of sour star fruit soaked in rock sugar
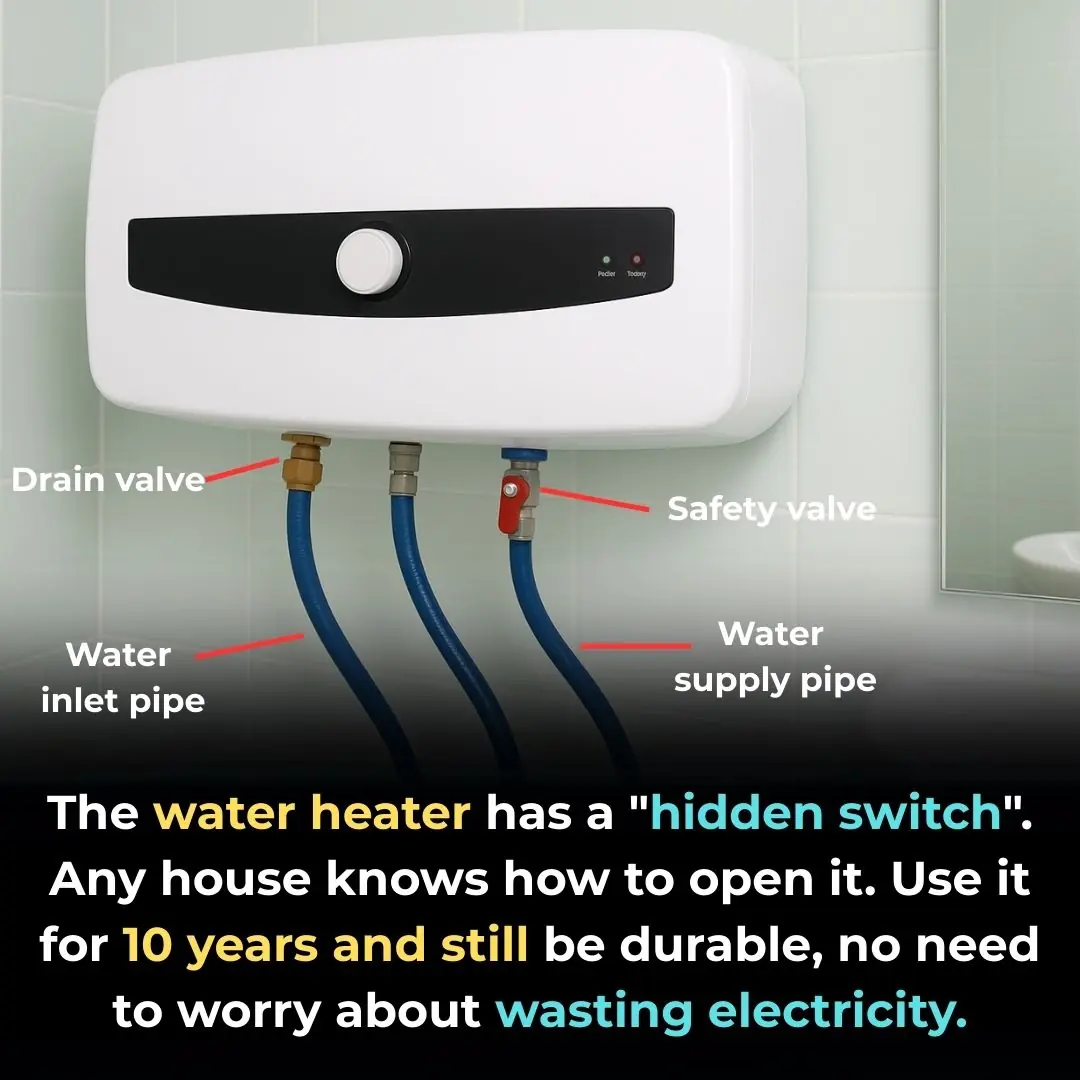
There is a "hidden switch" on the water heater that you can turn on and use for more than 10 years and it will still be durable.

Soak fish in this water, the fish meat will be firm, sweet, well-rounded, and will no longer have a fishy smell
Misunderstandings turn water purifiers into disease hotbeds, get rid of them immediately or your whole family will be harmed

10 foods to help fight fatty liver: Nutritionists recommend eating them every day!
Mix banana peels with this and leave it in the corner of the house. After just 1 night, all the cockroaches will run away

12 Moringa Seed Benefits You’ll Never Hear from Your Doctor (But You Should Know)

This is why you should never leave a water bottle in your car.

Supermarket staff reveal: 6 things never buy in supermarkets even on big sale

Ditch the Pills: Unlock Chayote’s Secret to Pain-Free, Vibrant Health! 🥗

7 types of food that won't spoil for a long time: It's still safe to eat after the expiration date, don't waste it
