
7 Warning Signs of Diverticulitis Most Doctors Miss
7 Warning Signs of Diverticulitis Most Doctors Miss
Did you know that diverticulitis sends more than 300,000 Americans to the hospital each year — and that number is steadily climbing? Even more troubling is that for many people, their first encounter with the term diverticulitis happens only after they’re doubled over in pain and sitting in an emergency room.
But it doesn’t have to reach that point. Your body often sends early warning signs long before a full-blown infection sets in. The challenge is that these signs can be subtle, inconsistent, or appear in unexpected ways — which is why even seasoned clinicians sometimes overlook them.
In this article, we’ll explore seven early warning signs of diverticulitis that can help you catch the condition early — possibly before it escalates into a medical emergency. Some of these are easy to miss or misinterpret, while others mimic completely unrelated issues. Understanding them can help you recognize red flags, ask better questions, and advocate for the right tests before things get serious.
(Based on insights from nutrition scientist Joe Leech, MSc)

Key Takeaways
-
Pain in a Specific Spot: Persistent, sharp discomfort in the lower-left abdomen is the number-one sign of diverticulitis.
-
Fever & Night Sweats: Infection-driven inflammation can raise your temperature and cause heat or sweating around the affected area.
-
Unpredictable Bowel Habits: Alternating between constipation and diarrhea is a strong clue that something is off in your colon.
-
Bladder-Like Symptoms: Painful urination or urinary frequency may actually stem from colon inflammation pressing on your bladder.
-
Pain in Unusual Areas: Nerve irritation can cause referred pain in the hip, groin, thigh, or even chest.
-
Age-Dependent Patterns: Younger people tend to have more aggressive cases; older adults may show vague or systemic symptoms instead of abdominal pain.
-
Severe, Localized Bloating: Trapped gas and bloating that won’t resolve — especially on the left side — can signal a developing flare.
1. Pain in the Lower-Left Abdomen: The Classic Clue
The hallmark symptom of diverticulitis is pain that’s steady, sharp, and anchored in the lower-left quadrant of your abdomen. To understand why, a quick anatomy refresher helps: diverticulitis develops when small pouches, called diverticula, form in weak spots of the colon wall and then become inflamed or infected. These pouches most commonly form in the sigmoid colon — the final, S-shaped section of your large intestine.
If you imagine your navel as the center of a cross, this pain typically sits in the lower-left box. It’s not the kind of stomach ache that moves around or comes and goes; it’s usually stubborn, worsening over time.
Other abdominal pain locations often point elsewhere:
-
Upper right: liver or gallbladder issues
-
Upper left: stomach or spleen concerns
-
Lower right: possible appendicitis
Interestingly, in people of Asian descent, diverticulitis often develops on the right side, where it can easily be mistaken for appendicitis. So even the location of pain can vary depending on genetics and diet patterns.
2. Fever and Night Sweats: The Infection You Don’t Notice
At its core, diverticulitis is an infection — and the body’s natural reaction is to raise its temperature. But the fever pattern can vary widely. Some people report low-grade fevers and drenching night sweats, while others experience a sense of heat specifically concentrated in the lower-left abdomen.
One patient described it perfectly:
“I’d wake up drenched, my sheets soaked, and my lower belly actually felt hot to the touch.”
These symptoms signal your immune system fighting inflammation in overdrive. But here’s the catch: up to 15% of patients never develop a fever at all. This can cause both patients and doctors to overlook the infection in its early stages.
If you experience any combination of fever, chills, or night sweats with localized abdominal pain — even mild — take it seriously. This isn’t the kind of “just wait it out” fever. It’s your body telling you something deeper is wrong.
3. Mixed and Confusing Bowel Changes
Your bowel habits are one of the best indicators of your gut’s health. When diverticulitis flares, the colon becomes inflamed, irritated, and sometimes partially blocked — causing a strange mix of diarrhea and constipation that can be baffling.
Some patients describe their stools as small, hard pellets (“like rabbit droppings”), while others swing to the opposite extreme with bouts of diarrhea. You might find yourself running to the bathroom multiple times but only passing tiny amounts.
This inconsistency is key. It’s not about whether you have diarrhea or constipation — it’s about sudden, unpredictable change from your usual rhythm. If your gut feels out of sync for more than a few days, and especially if it’s paired with pain or fever, it’s worth a medical evaluation.
4. Urinary Symptoms That Mimic a UTI
Here’s one most people — and many doctors — don’t realize: diverticulitis can cause urinary tract–like symptoms. Because the colon and bladder sit side by side in the lower pelvis, inflammation in one can irritate the other.
Common signs include:
-
Painful urination
-
Frequent urges to pee
-
A sensation of bladder fullness or pressure
In rare, more serious cases, diverticulitis can create an abnormal tunnel between the colon and bladder called a fistula. This allows gas or stool to leak into the urinary tract. Warning signs of a fistula include:
-
Air bubbles in urine (pneumaturia)
-
Stool particles in urine (fecaluria)
-
Recurrent UTIs that antibiotics don’t fix
If you notice these signs alongside digestive discomfort, don’t brush them off. This isn’t just a bladder issue — it’s a colon problem that’s crossed the line.
5. Pain in Unexpected Places: When the Body Sends Mixed Signals
Diverticulitis pain doesn’t always stay confined to the abdomen. Because nerves in the pelvic and lower abdominal regions overlap, inflammation can cause “referred pain” that radiates to the groin, hip, thigh, or even down one leg.
One patient put it this way:
“It feels like menstrual cramps gone wrong — pain that starts in my belly but spreads to my hip and thigh.”
Others experience a tight chest, cold hands, or even numbness in the leg on the affected side. These aren’t random sensations — they’re your body’s nervous system reacting to systemic inflammation.
Referred pain is also why diverticulitis can be misdiagnosed as kidney stones, ovarian cysts, endometriosis, or nerve compression. The rule of thumb: if multiple strange symptoms appear together — gut pain, urinary issues, tingling limbs — consider a digestive root cause.
6. How Age Changes Everything
Diverticulitis looks very different depending on your age.
-
In older adults, symptoms are often vague: fatigue, confusion, fainting spells, or kidney issues, with little to no abdominal pain. Because these symptoms mimic other conditions, diagnosis is frequently delayed. Recent studies suggest that anyone over 65 with unexplained infection or weakness should have a CT scan to rule out diverticulitis.
-
In younger adults (under 50), the opposite problem occurs — doctors may dismiss their symptoms because the disease was once considered an “old person’s issue.” Yet younger patients often develop more aggressive inflammation, and their cases are twice as likely to require surgical intervention.
Sometimes, the illness hides in plain sight. As one patient said,
“I never had sharp pain — just this dull, annoying pressure that wouldn’t go away. Turns out, I had diverticulitis the whole time.”
Pain isn’t the only indicator. Fatigue, bloating, and subtle digestive shifts are enough reason to pay attention — especially if they persist.
7. Persistent Bloating and Trapped Gas
Bloating happens to everyone, but in diverticulitis, it feels different. It’s localized, intense, and doesn’t improve with typical remedies like walking or taking gas-relief tablets.
During a flare-up, swelling and inflammation in the colon can create a partial blockage, preventing gas from moving through. This results in painful distention and a sensation of tightness in the lower abdomen — often on the same side as the infection.
Patients often describe the feeling as:
“My stomach feels hard as a rock. I can’t even pass gas.”
When bloating combines with fever, pain, or bowel changes, it’s time to take it seriously. Chronic or one-sided bloating is a red flag that deserves more than a casual “it’s probably just IBS” response.
Conclusion: Listen to What Your Body Is Whispering
Your body rarely goes silent — it’s constantly sending messages about what’s happening inside. Diverticulitis is one of those conditions that starts as a whisper and ends in a roar if ignored.
By learning to recognize these early warning signs — especially the combination of left-sided pain, bowel changes, bloating, and urinary issues — you can act sooner and potentially prevent hospitalization.
If your symptoms don’t add up, or if your gut tells you something’s off, trust that instinct. Request imaging, ask questions, and seek a second opinion if necessary.
The bottom line? Don’t settle for vague reassurances when your body is asking for attention. Understanding these subtle clues could save you from a painful — and entirely preventable — medical crisis.
News in the same category


The Best Natural Gout Treatments: Remove Uric Acid Crystallization To Prevent Gout And Joint Pain

4 things your hands could be telling you about the health of your kidneys

The Secret to Caring for Your Aging Skin – Gentle, Effective & Realistic

12 Amazing Benefits of Drinking Baking Soda Water Daily

5 Deficiencies Almost Everyone Has (And Doesn’t Know About)
Osteoporosis Is Scurvy of the Bone, Not Calcium Deficiency

This olive oil fasting trick resets insulin resistance — and triggers deep cellular cleanup

Forget Calcium — Doctors Say This Is the #1 Exercise for the Strongest Bones

This Ends Insulin Resistance (in Days, Not Years)
![Are You Being Misled About What Your Blood Pressure Should Be? [READ THIS CAREFULLY]](https://onplusnewscom.8cache.com/onplusnewscom/images/2025/10/25/1761400387Ii4TCVIhQj.webp)
Are You Being Misled About What Your Blood Pressure Should Be? [READ THIS CAREFULLY]
Medicinal Health Benefits of Turmeric, Curcumin and Turmeric Tea Based on Science

The Best Foods to Cleanse and Prevent Clogged Arteries

Capsaicin Stops Heart Attacks And Destroys Cancer Cells
17 Signs Your Body Is Too Acidic And 9 Ways To Quickly Alkalize It
Adrenal fatigue: what it is and 17 all-natural ways to fix it fast

Colon Cleansing With Kefir and Flaxseed Meal
Apple extract kills colon cancer cells better than chemotherapy drug
12 surprising foods that help dissolve blood clots naturally
News Post

7 Common Health Issues That Keep Appearing Could Be Early Warning Signs of Cancer

Small Life Hacks That Can Be Life-Saving
How to Sharpen Dull Scissors Without a Sharpening Stone: Simple and Effective Method

The Best Scientifically Proven Foods to Cleanse Your Liver
Flush the toxins silently damaging your kidneys — with these 13 powerful cleansing foods

The Best Natural Gout Treatments: Remove Uric Acid Crystallization To Prevent Gout And Joint Pain

4 things your hands could be telling you about the health of your kidneys

The Secret to Caring for Your Aging Skin – Gentle, Effective & Realistic

When Staying Alone in a Hotel: Place Two Cups on the Door Handle – A Small Action with Big Benefits

15 Things You Should Never Do to Protect Yourself from Lightning During Thunderstorms

12 Amazing Benefits of Drinking Baking Soda Water Daily

5 Deficiencies Almost Everyone Has (And Doesn’t Know About)
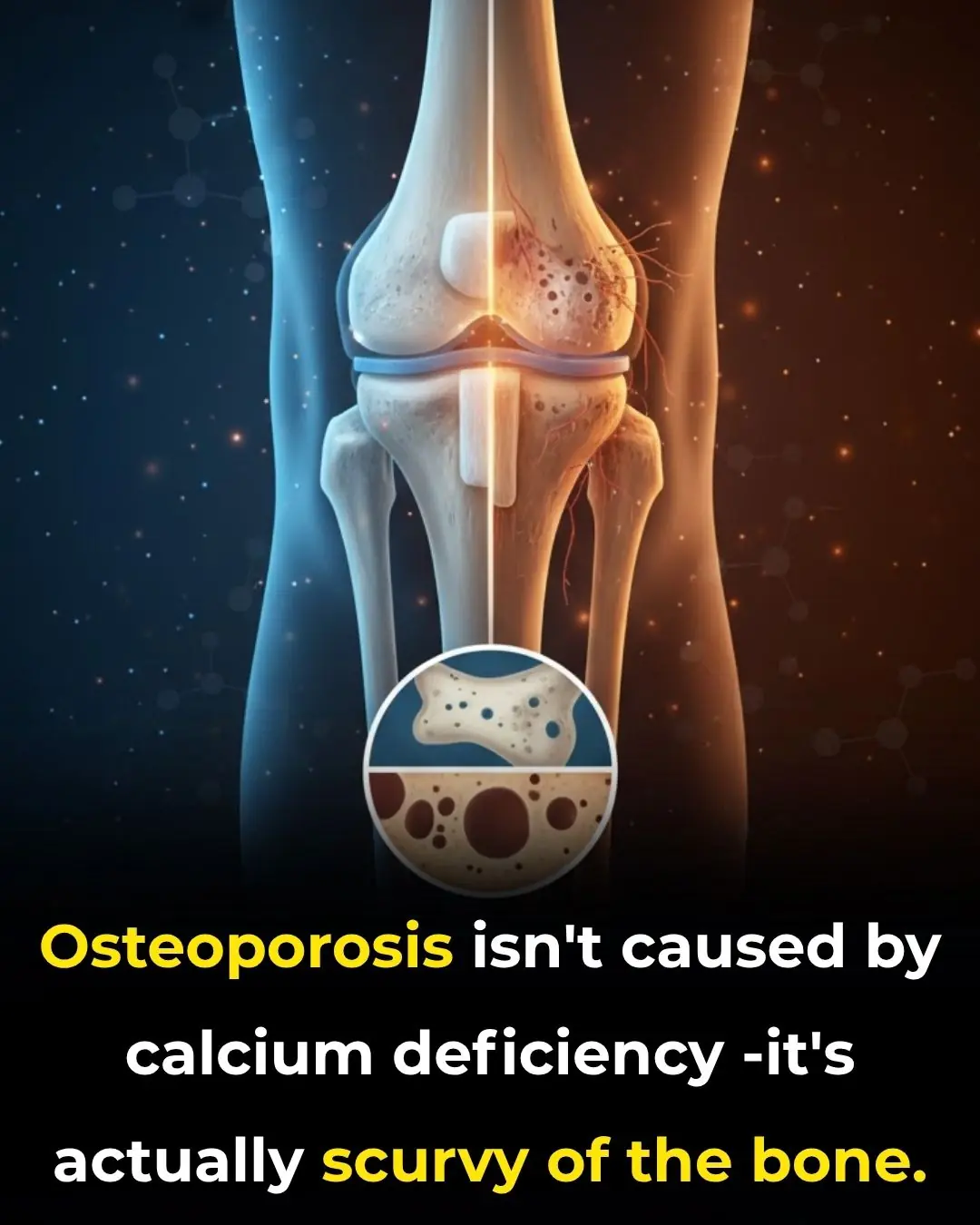
Osteoporosis Is Scurvy of the Bone, Not Calcium Deficiency

This olive oil fasting trick resets insulin resistance — and triggers deep cellular cleanup
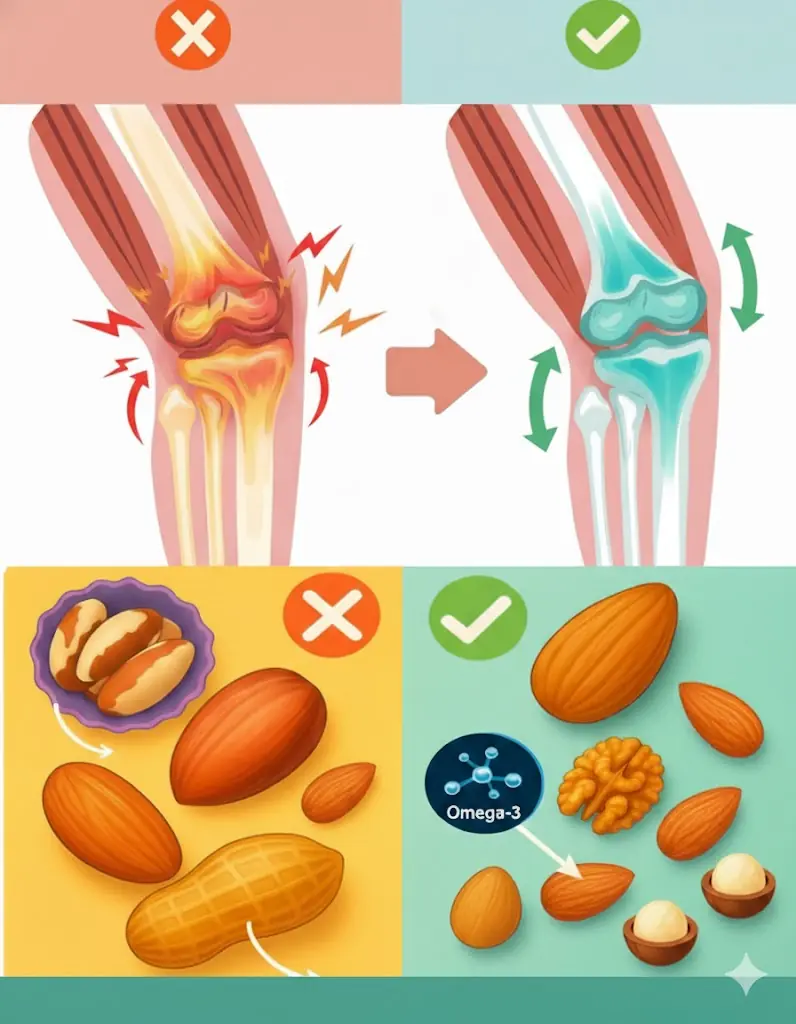
The Ultimate Nut Guide for Seniors: 4 Healthy Choices and 4 to Skip

The Man Who Walks for Dogs: Edgardo Perros’ 8,500-Mile Mission of Compassion

The Dog Who Went Out and Never Came Back the Same
To cook any kind of fish, just add a handful of these leaves: the fish will lose all its fishy smell and the meat will be rich and firm.

Great tips when growing pothos, in just 3 months the plant will form a beautiful green carpet
