A Fluorescent Breakthrough: New Dye Helps Surgeons Precisely Target Prostate Cancer
A breakthrough in cancer surgery may soon make tumour removal far safer and more precise. Researchers at the University of Oxford together with biotech firm ImaginAb Inc. have developed a fluorescent dye-based tracer called IR800-IAB2M that binds specifically to prostate cancer cells. When injected before surgery, this tracer adheres to a protein marker called Prostate-Specific Membrane Antigen (PSMA), which is commonly overexpressed on prostate cancer cells. Under a special imaging system, the dye makes cancerous tissue glow — giving surgeons a “second pair of eyes” to precisely see where tumours and potentially spread cancer cells are located. Đại học Oxford+2Genetic Engineering & Biotechnology News+2
In a small clinical trial involving 23 men with prostate cancer, all scheduled for robot-assisted radical prostatectomy, patients were injected with IR800-IAB2M before their operations. During surgery, surgeons used a dual-mode imaging platform (white light + near-infrared fluorescence) to visualise the prostate, pelvic lymph nodes, and surrounding tissues in real time. In many cases, the glowing dye revealed cancerous lesions that were invisible under normal surgical lighting — including small clusters of tumour cells that had spread beyond the prostate capsule and into lymph nodes or neighbouring tissues. Oxford Users+2NDS Oxford+2
Thanks to this enhanced visibility, surgeons were able to remove diseased tissue more completely while sparing healthy tissue — especially crucial structures involved in bladder control, sexual function, and other quality-of-life factors. This precision could significantly reduce the risk of recurrence and the need for repeat operations, as well as minimise the debilitating side effects that often follow prostate cancer surgery. Technology Networks+2Inside Precision Medicine+2
Crucially, the study reported no adverse side effects from administration of the dye-tracer, underscoring its safety for clinical use. Oxford Users+1 The fluorescent minibody-based tracer relies on a humanised PSMA-targeting antibody fragment (the “minibody” IAB2M), conjugated to a near-infrared dye (IRDye 800CW), making IR800-IAB2M highly specific — it binds to PSMA and not to other molecules. Genetic Engineering & Biotechnology News+1
While this technique does not cure cancer by itself, it represents a major leap forward in how tumours are visualised and removed surgically. By improving the detection of cancerous tissue — including microscopic spread — it could drastically lower rates of incomplete tumour removal, recurrence, and the physical harms associated with over-extensive tissue excision. Đại học Oxford+2ORA+2
What’s more, experts believe this approach could be adapted to other types of cancer. By changing the targeting molecule to bind proteins unique to different cancer cells, similar fluorescent tracers may one day assist surgeons worldwide in removing tumours safely and precisely — potentially reshaping cancer surgery across disciplines. The Independent+2ImaginAB+2
The first-in-human study of IR800-IAB2M — part of the clinical trial dubbed ProMOTE trial — was published in the peer-reviewed journal European Journal of Nuclear Medicine and Molecular Imaging. Oxford Users+1 The trial showed that intraoperative fluorescence imaging of prostate cancer tissue is feasible and safe, and that IR800-IAB2M can meaningfully improve a surgeon’s ability to distinguish between healthy and cancerous tissue during real-time surgery. Đại học Oxford+2ORA+2
Although further trials — including larger, randomized studies — are underway (for example with higher-risk patients) to validate whether this technique consistently leads to better long-term outcomes, the early results are promising. Many in the medical community regard this as a potentially transformative step in the evolution of “precision surgery.” Ndorms+1
In short: while not a magic bullet, IR800-IAB2M and its associated imaging technique offer a powerful new tool — giving surgeons the clarity they need to remove cancer completely while preserving the patient’s quality of life. It could herald a new era where tumours are not only removed — they are illuminated, scrutinised, and surgically excised with near-microscopic precision.
News in the same category
Fingerprint Individuality: A Story Written by Biology, Environment, and Chance

Northwestern Study Reveals Hidden Dangers in Youth Skincare Influencer Culture
Scientists Discover a Brain Receptor That Acts as a Natural Shield Against Alzheimer’s
The Shocking Secret of Spider Flight: How Electric Forces Lift Them Into the Sky

When a Humpback Whale Became a Hero: The Extraordinary Rescue of Marine Biologist Nan Hauser

🤯 Beyond the Void: How Quantum Physics Suggests the End of Life Is an Illusion

🧠 Medical Marvel: The Bullet That Accidentally Cured Severe OCD
If you kiss a deceased loved one, you should know that it causes ...
When a Woman Bites Her Lip While Staring at You, It Means She Is ...

3 flowers that make snakes tremble with fear — beautiful and safe to plant around your home

Meet Jonathan: The 192-Year-Old Tortoise Who Has Witnessed History and Continues to Inspire

Retired Couple in UK Successfully Nurtures 90-Million-Year-Old Wollemi Pine, Leading to Its First Reproduction Outside Australia
Stem Cell Therapy for Type 1 Diabetes Shows Promise in Human Clinical Trials

Have you noticed small white spots on your arms or legs… and you don't know what they are?
How Guyana Became the Only Nation Fully Self-Sufficient in All Seven Major Food Groups
Donald Trump's new scarf leaves everyone saying the same thing

Scientists May Have Just Found a Breakthrough Hair-Loss Treatment

Panama's Marine Collapse: The End of a Key Ocean Upwelling System and What It Means for the Future
News Post

Study Finds Parents Show More Affection to Daughters Than Sons Worldwide
US Researchers Develop Ultra-Light Metal Foam That Stops Armor-Piercing Bullets
🛁 Say Goodbye to the Shower: Japan Unveils the 15-Minute "Human Washing Machine"
Fingerprint Individuality: A Story Written by Biology, Environment, and Chance

Northwestern Study Reveals Hidden Dangers in Youth Skincare Influencer Culture

Japanese Scientists Launch Human Trials for TRG-035, a Drug That Could Regrow Lost Teeth Naturally
Scientists Discover a Brain Receptor That Acts as a Natural Shield Against Alzheimer’s
The Shocking Secret of Spider Flight: How Electric Forces Lift Them Into the Sky

When a Humpback Whale Became a Hero: The Extraordinary Rescue of Marine Biologist Nan Hauser

🤯 Beyond the Void: How Quantum Physics Suggests the End of Life Is an Illusion

Mauro Morandi: Living 33 Years in Complete Solitude on a Remote Italian Island

🧠 Medical Marvel: The Bullet That Accidentally Cured Severe OCD

One simple scoop a day can spark full-body healing — here’s what happens next

Twenty-Year-Old Nokia 3310 Still Holds 70% Battery, Highlighting the Longevity of Early Mobile Phones

Magnetic Rice-Sized Robot Could Revolutionize Non-Invasive Kidney Stone Treatment

4 Unusual Morning Pains You Should Never Ignore — They May Signal a Hidden Tumor
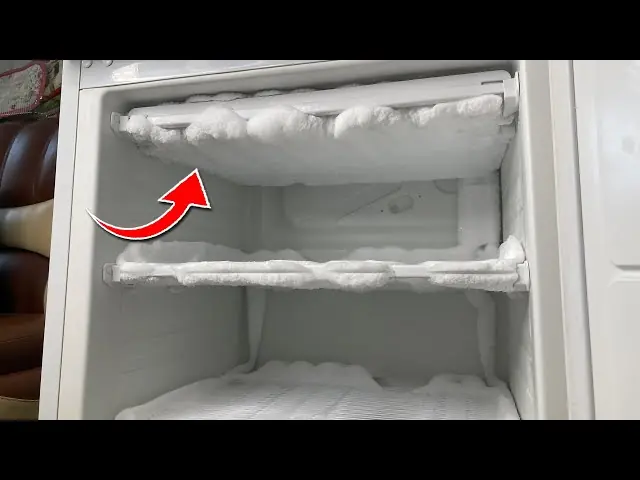
Quick & Easy Freezer Defrost Hack: Melt Ice in Just 5 Minutes with Zero Effort

A Love That Never Looked Away — The Story of Ron and Cheryl.
