
Never Mix Medications in One Box: 10 Serious Risks Most People Don’t Know
In our fast-paced world, it’s easy to look for shortcuts—especially when managing multiple prescriptions. Many people, hoping to simplify their daily medication routines, mix all their pills in a single box or container. While this might seem harmless and convenient, health experts warn that it can be a dangerous mistake with serious consequences.
According to pharmacists at the Mayo Clinic, even minor errors in medication storage can lead to reduced effectiveness, harmful chemical reactions, or dangerous overdoses (Mayo Clinic, 2023). Understanding the hidden risks of mixing medications is crucial for anyone taking more than one prescription. Below are 10 serious dangers most people don’t realize when storing different drugs together.
1. Risk of Chemical Reactions
Every medication is formulated to remain stable under specific conditions—temperature, light, and humidity. When several drugs are mixed in one container, their chemical compounds may interact, causing instability or even forming toxic byproducts.
For example, certain antibiotics and vitamins can react with each other, reducing potency or creating unwanted chemical residues (Healthline, 2024). Even minor chemical changes can alter a drug’s absorption or effectiveness, particularly in medicines with a narrow therapeutic index, where even a small dosage change can be dangerous. Storing each medication separately is the only reliable way to prevent unintended chemical interactions.
2. High Risk of Accidental Overdose
When pills of different colors and sizes are mixed together, keeping track of doses becomes confusing—especially for older adults or those managing multiple prescriptions. A simple mix-up can result in taking an extra pill or the wrong one altogether.
The Centers for Disease Control and Prevention (CDC) reports that medication errors cause more than one million emergency room visits each year in the U.S. (CDC, 2023). Accidental overdoses can damage the liver, kidneys, or heart and, in severe cases, can be fatal. Keeping medications in labeled compartments or their original packaging is a simple but life-saving habit.
3. Increased Side Effects and Drug Interactions
Mixing medications can unintentionally amplify side effects. For instance, combining two drugs that cause drowsiness—such as antihistamines and certain painkillers—can lead to extreme sedation or dizziness, impairing driving or coordination.
Harvard Health notes that some medications compete for the same liver enzymes that metabolize drugs, leading to dangerously high levels in the bloodstream (Harvard Health, 2022). The outcome? Greater fatigue, nausea, or even life-threatening reactions like respiratory depression. Always consult a pharmacist before storing or taking medications together.
4. Reduced Effectiveness Over Time
Medications exposed to light, moisture, or heat can lose potency faster. Mixing pills in one box makes it nearly impossible to protect each one according to its storage requirements.
For instance, antibiotics like amoxicillin can degrade in humid conditions, while nitroglycerin tablets lose potency when exposed to air (WebMD, 2024). Once potency decreases, the medication may no longer effectively treat the condition it was prescribed for. Keeping each drug in its original airtight container ensures its stability and shelf life.
5. Confusion and Misidentification
When pills look similar, even experienced patients can confuse them—especially in low light or during busy mornings. For someone with visual impairments or memory challenges, the risk of error increases dramatically.
GoodRx pharmacists emphasize that even a single mix-up between medications like metformin (for diabetes) and atenolol (for blood pressure) can trigger dangerous complications (GoodRx, 2023). Keeping medications labeled and organized eliminates this unnecessary risk.
6. Cross-Contamination Risks
Tiny particles from one medication can transfer to another, a process known as cross-contamination. This can alter dosage accuracy or trigger unexpected allergic reactions.
This issue is particularly concerning for sensitive drugs like thyroid medication, insulin, or chemotherapy pills, which require precise dosing (Cleveland Clinic, 2023). Even residue dust from one pill can compromise another’s safety. Separate storage with tight-sealed containers prevents contamination.
7. Losing Track of Expiration Dates
Mixing pills makes it impossible to monitor which medications are expired. Over time, expired drugs may lose potency—or worse, break down into toxic substances.
For example, tetracycline antibiotics can degrade into compounds that harm the kidneys (U.S. FDA, 2023). By keeping medications in their original packaging, you can easily check expiration dates and safely discard old ones.
8. Complications During Emergencies
In emergencies, clear identification of your medications can help medical staff save your life. If all your pills are mixed in one box, healthcare providers may have no idea what you’re taking, how much, or why.
A report by the American Pharmacists Association shows that incomplete medication information delays treatment and increases medical errors in emergency settings (APhA, 2022). Keeping prescriptions in labeled bottles or maintaining a written list of medications ensures faster, safer care.
9. Legal and Safety Liabilities
In some countries, tampering with or relabeling prescription drugs violates pharmaceutical regulations. If mixed medication storage leads to harm—especially in caregiving settings—it may even result in legal liability.
Following the original labeling and packaging guidelines is not only safer but also ensures compliance with drug safety laws. This is especially crucial in households caring for children or elderly family members.
10. Misleading “Viral Hacks” and Myths
Social media is full of so-called “organizing hacks” that encourage people to simplify pill storage. However, many of these viral tips ignore basic pharmaceutical science. Mixing medications for convenience can lead to all the risks mentioned above—and none of the promised benefits.
Medical professionals at Johns Hopkins Medicine caution that online health trends should never replace advice from a licensed pharmacist or physician (Johns Hopkins, 2024). Always verify such claims with trusted healthcare sources.
11. Safe Storage Best Practices
To protect your health, store medications in their original packaging or use a labeled pill organizer with separate compartments for each day and time. Keep them in a cool, dry place, away from direct sunlight and moisture.
For added safety:
-
Review your medication list regularly with your doctor or pharmacist.
-
Keep emergency contact and medication information in your wallet or phone.
-
Dispose of expired drugs at authorized collection points rather than throwing them in the trash.
By following these best practices, you can maintain medication effectiveness and greatly reduce the risk of harmful mistakes.
Bottom Line
Mixing medications in one container may seem efficient, but it’s a shortcut that risks your safety. As the World Health Organization (WHO) emphasizes, “Medication safety begins with proper handling and awareness” (WHO, 2023). By storing medicines correctly and consulting trusted medical professionals, you protect not only your health but potentially your life.
Sources:
-
Mayo Clinic (2023) – Safe Medication Storage and Handling
-
Healthline (2024) – How to Store Medications Properly
-
CDC (2023) – Medication Safety and Poisoning Prevention
-
Harvard Health Publishing (2022) – Drug Interactions and Safety
-
WebMD (2024) – Stability and Potency of Prescription Drugs
-
Cleveland Clinic (2023) – Cross-Contamination Risks in Medication Use
-
FDA (2023) – Expired Drugs and Potential Hazards
-
APhA (2022) – Medication Management in Emergencies
-
Johns Hopkins Medicine (2024) – The Dangers of Viral Health Hacks
-
WHO (2023) – Global Patient Safety Alert
News in the same category


Drop a Silver Foil Ball Into Your Toilet — The Results Are Surprisingly Brilliant

5 Amazing Health Benefits of Drinking Fresh Turmeric Water

Why You Should Sprinkle Salt on Your Gas Stove
3 Flowers That Make Snakes Tremble — Natural Repellents You Can Grow at Home

You’re Taking Iron Supplements Wrong — Here’s the Science-Backed Way to Do It Right

Nana’s Baking Soda Hack: The Surprisingly Effective Trick to Soften and Thin Thick Toenails

The Right Way to Take Ashwagandha: A Science-Backed Guide to Unlock Its Full Potential

‘One Less Thing That I Have to Think About’: Michelle Obama Dishes on Life After the White House and the Freedom That Came With It

78-Year-Old Grandmother Is Inspiring Others To Stay Active Through Powerlifting

Coco Gauff Donates $100K to UNCF to Fund Scholarships for HBCU Tennis Players

Honoring Revolutionary Audre Lorde: The Poet Who Dared Us All To Be Powerful

5 Black YouTube Channels That Make Exercising Fun For Beginners

Grant Hill and Chris Webber Join Ownership Group to Bring WNBA Team Back to Detroit
Remembering Civil Rights Titan and Congressman John Lewis

Boiling Sweet Potatoes: Don’t Just Add Plain Water—Add This Spoonful for Perfectly Fluffy, Sweet Results

The Science Behind Putting a Cotton Swab in a Menthol Oil Bottle

More People Are Struggling with Visceral Fat — Doctors Reveal 9 Foods That Help Burn It Naturally
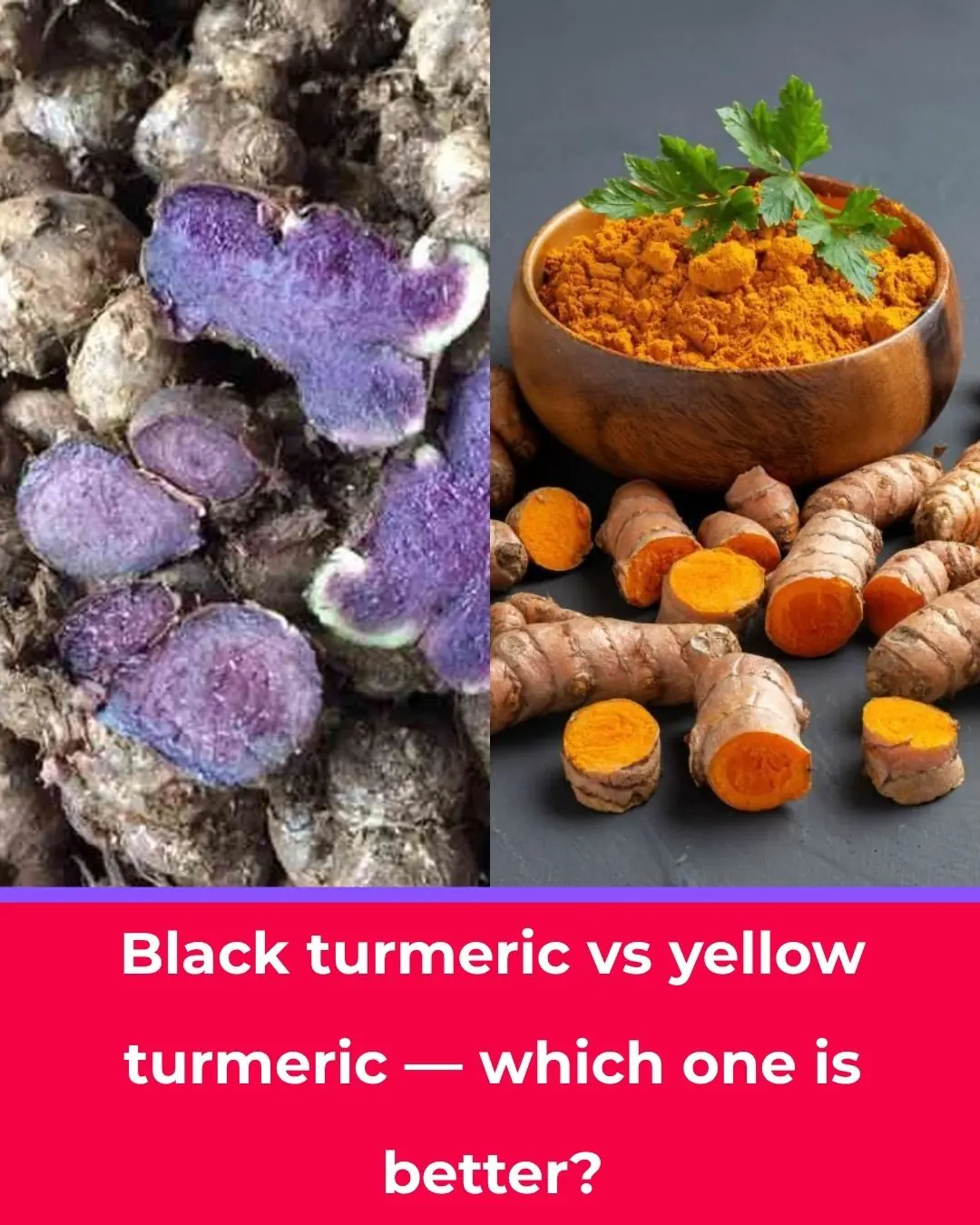
Black Turmeric vs. Yellow Turmeric: Which One Is Better?
News Post

The Best Tea for Mornings and After Dinner: A Powerful Blend for Health

Homemade Vitamin E Cream for Face – Vitamin E Oil benefits for Skin

DIY Rice Cream for Glowing Skin - The Ultimate Anti-Aging Moisturizer

This DIY curry leaves and lemon oil can give your hair healthy growth

Grow Date Trees From Seed (Start in a Pot → Plant Outdoors): The Complete, No-Stress Guide
Should You Place a Fan Close to or Far from the Bed While Sleeping? Many Homes Are Doing It Wrong

Simple, Cost-Free Ways to Fix Moldy or Peeling Walls — Easy Solutions for Every Home

The Incredible Benefits of Common Comfrey: Uses, Remedies, and Precautions

Why Do Fish Sellers Often Use Black Plastic Bags? A Simple Trick Few People Notice
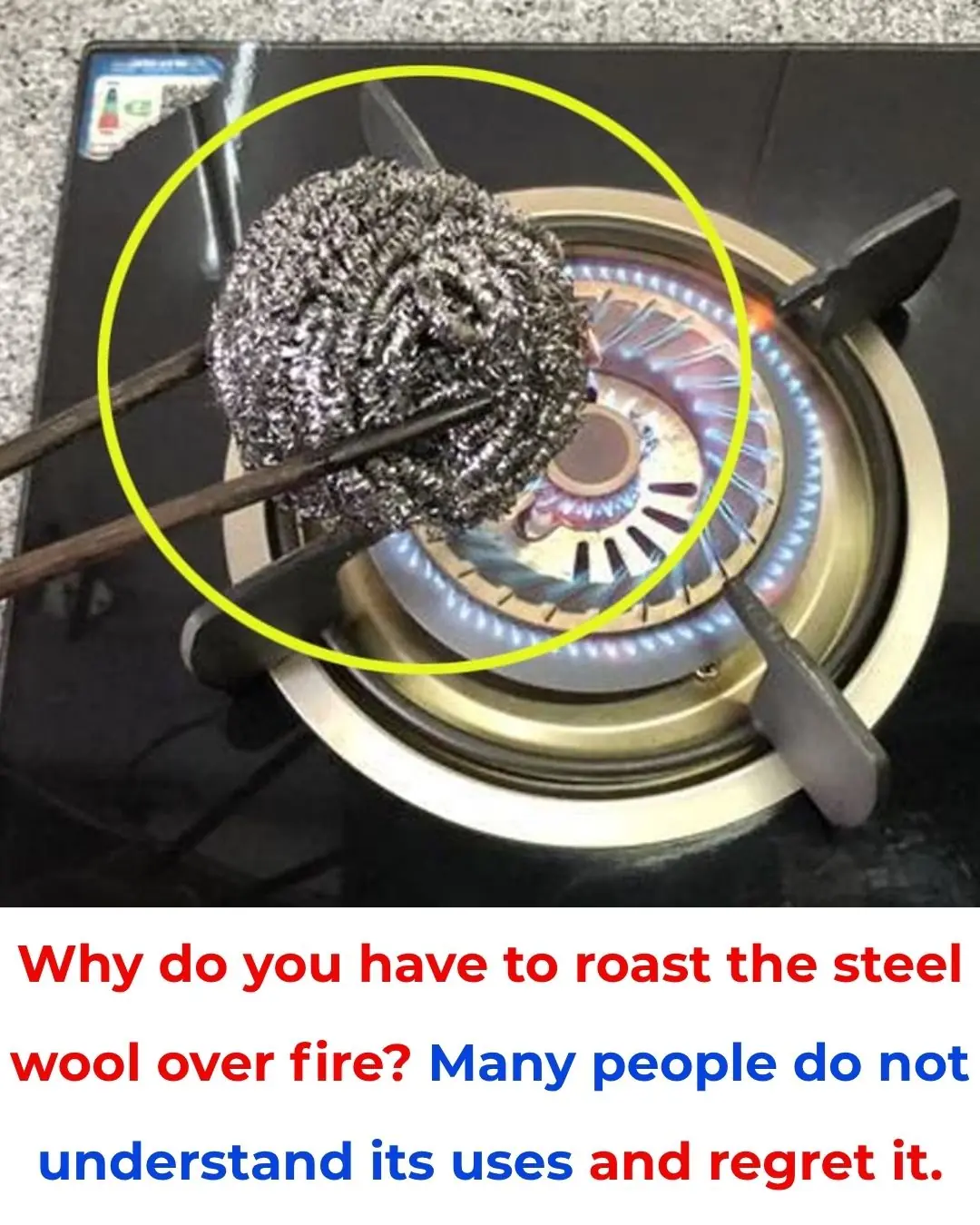
Why Do We Burn Steel Scrub Pads Over Fire? Many People Don’t Know This Useful Trick
Scientists discover evidence of 'Adam and Eve' living 200,000 years ago

14 Reasons to Drink Lemon Water First Thing in the Morning

You're doing it all wrong. Here’s the right way to store potatoes
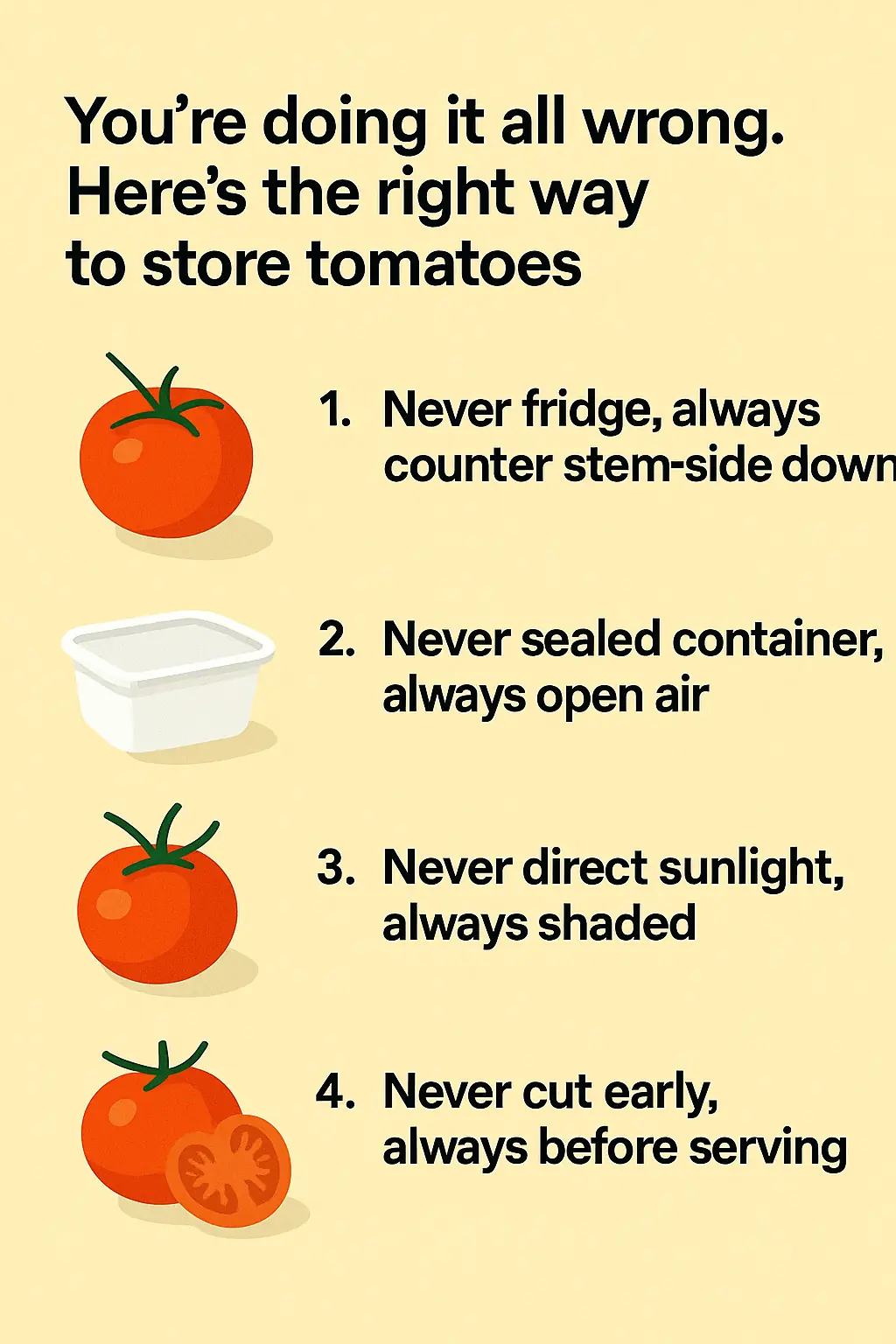
You're doing it all wrong. Here’s the right way to store tomatoes

Drink THIS every morning to BOOST leg circulation!

Preserving eggs without a refrigerator, using this method, the eggs will stay fresh for a whole month

Drop a Silver Foil Ball Into Your Toilet — The Results Are Surprisingly Brilliant

5 Amazing Health Benefits of Drinking Fresh Turmeric Water

Rice Water for Skin | DIY Toner Benefits to Remove Dark Spots & Shrink Large Pores
