New Evidence Links Hepatitis C to Brain Pathways in Mental Illness
A surprising scientific breakthrough is reshaping the way researchers think about mental illness. Recent investigations have revealed traces of the Hepatitis C virus (HCV) within brain-related tissues of individuals diagnosed with bipolar disorder and schizophrenia. Although the finding does not prove that the virus directly causes these psychiatric conditions, it raises provocative questions about the role of infections, immune responses, and neurological vulnerability in mental health. This unexpected result opens new possibilities for understanding how viral activity might interact with the brain in ways previously overlooked.
For decades, mental illnesses such as bipolar disorder and schizophrenia have been approached primarily through the lenses of genetics, neurotransmitter imbalance, and structural changes in the brain. While these factors remain essential, the emerging evidence suggests that they may not tell the whole story. Researchers from several respected institutions, including Johns Hopkins University, have identified viral RNA associated with Hepatitis C in the choroid plexus, a membrane responsible for producing cerebrospinal fluid and maintaining the brain’s protective barrier. Although this tissue is not part of the neuronal cortex, its interaction with the brain makes the discovery scientifically meaningful. According to a 2025 study in Translational Psychiatry, viral presence in this region may influence neuroinflammatory pathways, which are increasingly recognized as potential contributors to psychiatric symptoms.
The idea that infections could shape mental health is not entirely new but has gained strong momentum in recent years. Prior research, including publications from the National Institutes of Health (NIH) and the Journal of Clinical Investigation, has highlighted how chronic viral infections can alter immune responses, disrupt neurological signaling, and trigger long-term inflammation. In the case of Hepatitis C, earlier studies have already shown that the virus can affect cognitive function, mood regulation, and fatigue—even in individuals without diagnosed psychiatric disorders. The new findings add another layer of complexity, suggesting that the immune system’s interaction with the virus might heighten susceptibility to certain mental illnesses or influence how they progress.
These insights could have significant implications for clinical practice. If viral activity or immune dysregulation contributes to psychiatric symptoms, treatments that target inflammation, antiviral mechanisms, or disruptions in the blood–brain barrier might become viable additions to existing therapies. This could help explain why some patients show limited response to conventional psychiatric medications and why more personalized, biology-based approaches are urgently needed. Future interventions may include combining psychiatric care with antiviral therapy, immune-modulating treatments, or diagnostic screening that identifies infection-related risk factors.
However, scientists caution that much more research is required before drawing definitive conclusions. The presence of viral RNA does not mean that Hepatitis C directly causes bipolar disorder or schizophrenia, nor does it imply that all patients with these conditions harbor the virus. Large-scale studies and advanced neuroimaging will be necessary to clarify the mechanisms at play, determine the prevalence of viral involvement, and assess whether these findings can be replicated in broader populations. Researchers also emphasize the importance of distinguishing correlation from causation—a critical step in preventing misinterpretation of early data.
Even with these uncertainties, the discovery marks an important turning point in the study of mental health. It underscores the intricate relationship between the brain, the immune system, and external biological agents such as viruses. By expanding the scope of psychiatric research beyond traditional frameworks, scientists hope to unlock new strategies for prevention, diagnosis, and treatment. Ultimately, this line of investigation may pave the way for a more comprehensive and personalized understanding of mental illness—one that accounts not only for genetics and neurochemistry but also for the subtle, long-term impact of infections on the human brain.
Sources:
-
Johns Hopkins University, Translational Psychiatry (2025)
-
National Institutes of Health (NIH) – Mental Health and Immunology Research
-
Journal of Clinical Investigation: Viral infections and neuroinflammation
-
Centers for Disease Control and Prevention (CDC): Hepatitis C neurological effects
News in the same category

Goodbye Synthetic Dyes: Doritos Join the Push for Cleaner, Transparent Ingredients
Breakthrough Research Suggests Kidney Damage May Be Reversible After All

How Intermittent Fasting Protects the Heart: New Evidence on Blood Clots and Cardiovascular Health

If You See a Woman Wearing a Wedding Ring On Her Pinky, Here's What It Means

Reinventing Renewable Energy: Germany Launches Compact Turbine for Off-Grid Power

Rethinking Depression: New Brain-Imaging Research Reveals It’s More Than a Chemical Imbalance

Seventeen Years Lost: How a Look-Alike Helped Free an Innocent Man
You Must Live Without One Modern Comfort — Your Choice Reveals Who You Really Are

Why do foreigners use electric kettles so little even though they are very convenient?

How Poor Sitting Posture Impacts Your Spine, Muscles, and Overall Health
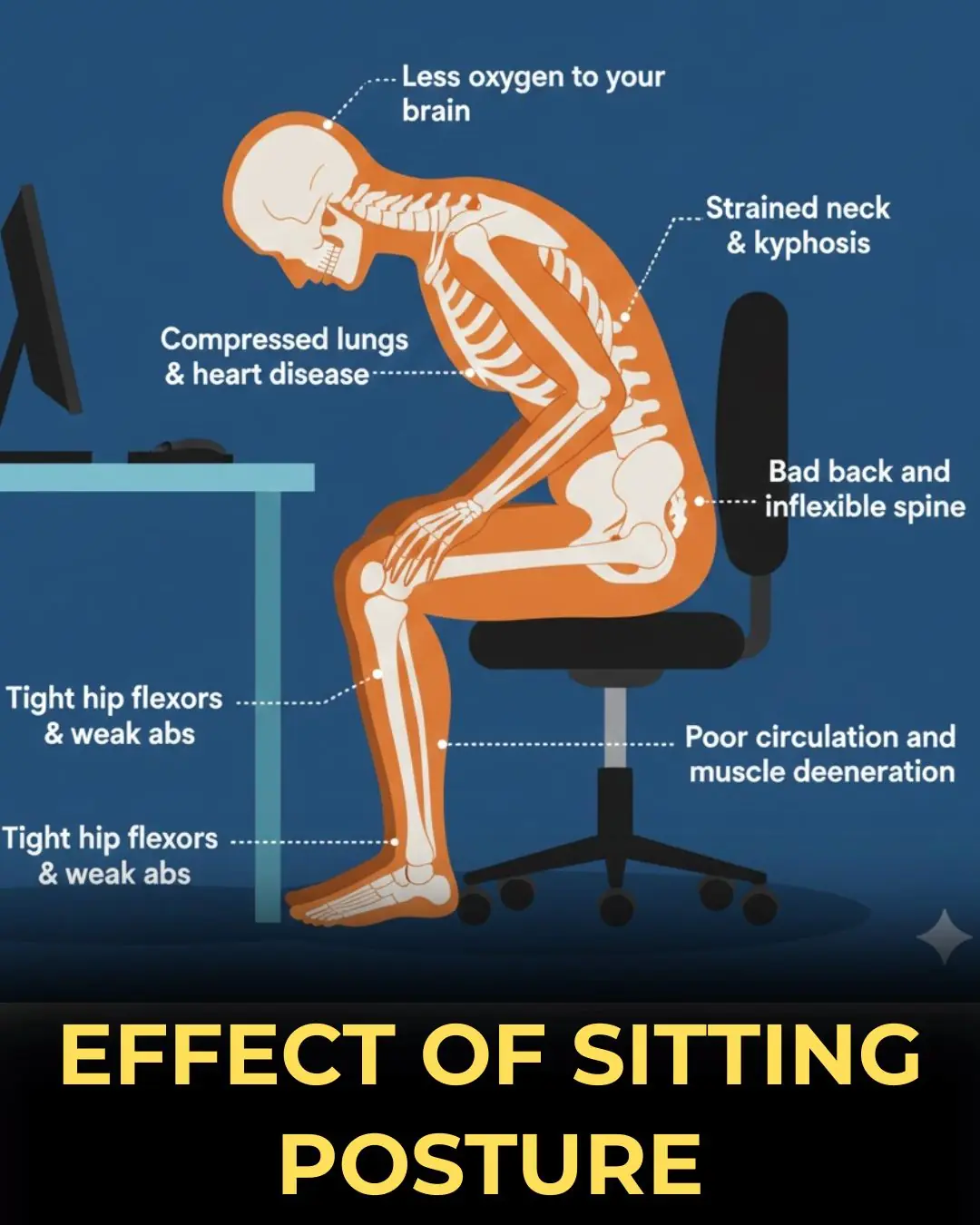
Understanding the Long-Term Consequences of Poor Sitting Posture
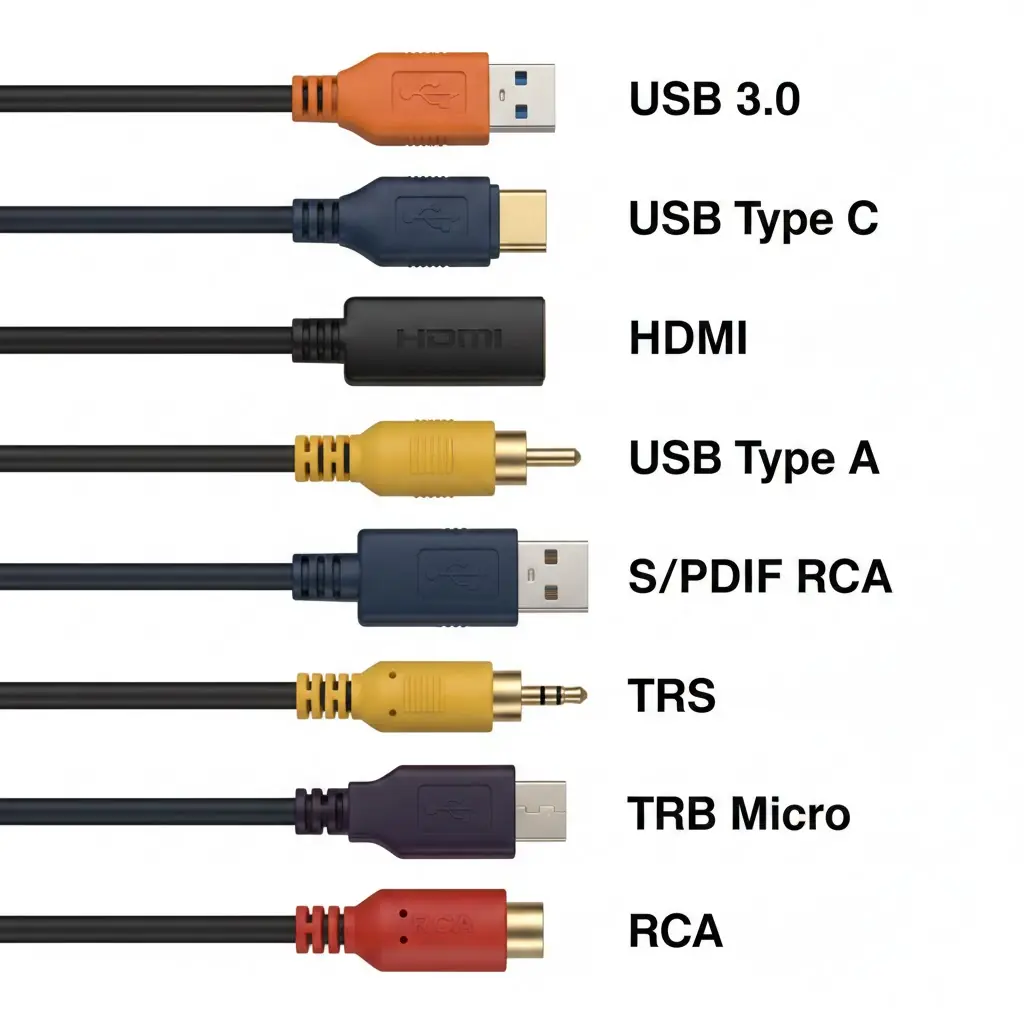
A Complete Guide to Common Cable Types and How They Keep Devices Connected
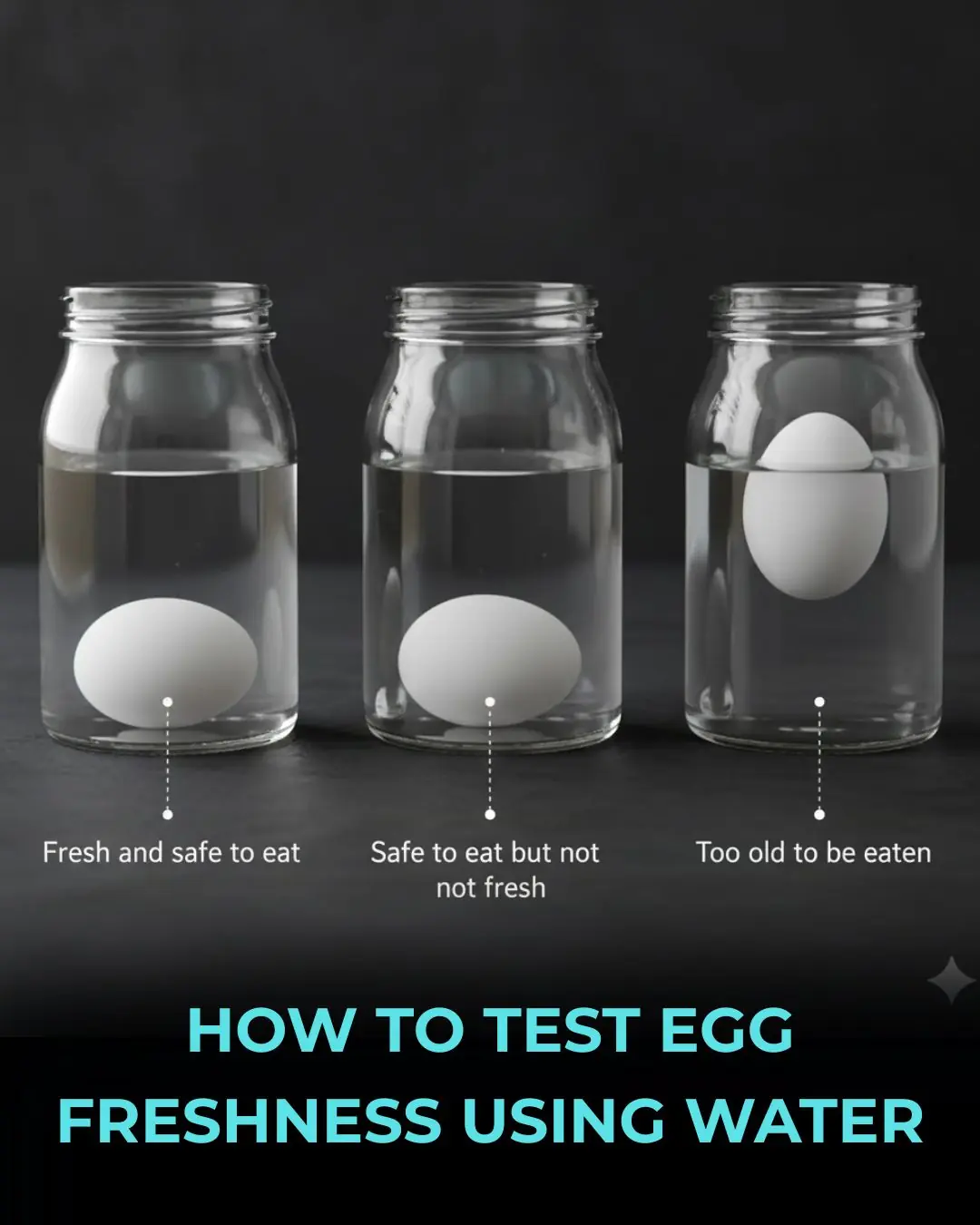
Egg Freshness Explained: What Sinking, Tilting, and Floating Really Mean

A Sleeping Giant Stirs: Taftan Volcano Experiences Uplift Driven by Shallow Gas Pressure
The Healing Power of Touch: How Hugs Support Emotional Balance and Immune Health

Why Sleeping in Socks Might Be the Secret to Better Sleep
Think Bottled Water Is Safer Think Again

Can Eggs Protect Your Mind? Emerging Evidence Suggests a Cognitive Benefit
News Post
Injectable Gel Breakthrough Brings New Hope for Nerve Regeneration

Why Boiled Eggs Deserve a Spot on Your Breakfast Table

Goodbye Synthetic Dyes: Doritos Join the Push for Cleaner, Transparent Ingredients
Breakthrough Research Suggests Kidney Damage May Be Reversible After All

How Intermittent Fasting Protects the Heart: New Evidence on Blood Clots and Cardiovascular Health

ITV breaks silence as Celebrity Big Brother is ‘axed from ITV schedule’

Peter Andre teases ‘special’ project with wife Emily: ‘We are having exciting meetings’

🚫 When to Avoid Ginger — 6 Medical Conditions That May Be Affected

What Happens to Your Body When You Eat Canned Tuna Every Day

I’m A Celebrity star Kelly Brook’s husband reveals when he’s flying out to Australia

Kris Jenner shows support for Meghan Markle weeks after Kardashians photo scandal

Inside Angry Ginge’s ‘bromance’ with Angry Ginge – how they met; ‘going to war’ over diss track; huge ‘risk’ that ‘paid off’

Ant McPartlin’s tattoos explained – tribute to wife Anne-Marie; uproar over ‘missing’ family member; nod to his recovery

Emmerdale disaster incoming: Bear’s fate ‘sealed’ as Joshua Richards makes devastating admission

How Do Farmers Grow Avocado Trees
Robron plot Kev’s downfall – but Emmerdale fans declare they ‘love him’

If You See a Woman Wearing a Wedding Ring On Her Pinky, Here's What It Means

2-Minute Painless Hair Removal: Natural At-Home Solution