
Not All JAK Inhibitors Are the Same: Applying Evidence-Based Differences in Atopic Dermatitis Treatment

Atopic dermatitis (AD) is a chronic, inflammatory skin disease characterized by intense pruritus, recurrent eczematous lesions, and a significant impact on quality of life. In recent years, Janus kinase (JAK) inhibitors have emerged as an important systemic treatment option for patients with moderate-to-severe atopic dermatitis. However, not all JAK inhibitors are the same. Differences in selectivity, efficacy, safety profiles, and real-world applicability make it essential for clinicians to understand how these agents compare and how to choose the most appropriate therapy for individual patients.
This CME activity explores the key distinctions among systemic JAK inhibitors used in atopic dermatitis and provides guidance on translating the latest clinical evidence into real-world treatment decisions.
Understanding the JAK-STAT Pathway in Atopic Dermatitis
The JAK-STAT signaling pathway plays a central role in immune regulation and inflammatory responses. In atopic dermatitis, cytokines such as interleukin (IL)-4, IL-13, IL-31, and interferon-γ drive inflammation, skin barrier dysfunction, and pruritus. These cytokines signal through different JAK enzymes—primarily JAK1, JAK2, JAK3, and TYK2.
Systemic JAK inhibitors work by blocking one or more of these enzymes, thereby reducing downstream inflammatory signaling. However, the degree of selectivity for specific JAK enzymes varies among agents, which directly influences both therapeutic benefits and safety risks.
Key Differences in Efficacy Among Systemic JAK Inhibitors
Clinical trials have demonstrated that systemic JAK inhibitors can provide rapid and meaningful improvements in atopic dermatitis, often with faster itch relief compared to some biologic therapies. However, efficacy is not uniform across agents.
-
JAK1-selective inhibitors tend to show strong efficacy in reducing pruritus and skin inflammation, reflecting the central role of JAK1-mediated cytokines in AD pathophysiology.
-
Less selective JAK inhibitors may offer broad immunomodulation but do not necessarily translate to superior clinical outcomes in atopic dermatitis.
Differences in trial endpoints—such as EASI-75, EASI-90, Investigator’s Global Assessment (IGA) response, and time to itch relief—highlight that some agents achieve higher response rates or faster symptom control. Understanding these nuances helps clinicians align treatment choice with patient priorities, such as rapid itch reduction or long-term disease control.
Safety Profiles: Why Selectivity Matters
Safety considerations are critical when prescribing systemic JAK inhibitors. While all agents in this class share certain warnings, the risk profile can differ based on JAK selectivity, dosage, and patient characteristics.
Key safety considerations include:
-
Infections: Herpes zoster and other opportunistic infections have been reported, with risk varying by agent and patient age.
-
Laboratory abnormalities: Changes in lipid levels, liver enzymes, and blood counts may occur and require monitoring.
-
Cardiovascular and thromboembolic risk: These risks appear to be influenced by patient-specific factors such as age, smoking status, and comorbidities, as well as by the degree of JAK inhibition beyond JAK1.
-
Long-term safety: Ongoing real-world data and post-marketing surveillance continue to refine our understanding of long-term risk.
A more selective JAK1 inhibitor may reduce off-target effects associated with JAK2 or JAK3 inhibition, potentially improving the benefit–risk balance for certain patients.
Applying Evidence to Real-World Treatment Decisions
Choosing the right systemic JAK inhibitor for atopic dermatitis requires an individualized approach. Clinicians should consider:
-
Disease severity and symptom burden, particularly the impact of itch on sleep and daily functioning
-
Patient age and comorbidities, including cardiovascular risk factors and history of infections
-
Previous treatment response, including biologics and conventional systemic therapies
-
Need for rapid symptom control versus long-term maintenance therapy
-
Patient preferences, such as oral versus injectable treatments and monitoring requirements
Shared decision-making is essential. Discussing both the potential benefits and risks allows patients to make informed choices aligned with their treatment goals.
Conclusion
Systemic JAK inhibitors have transformed the treatment landscape for moderate-to-severe atopic dermatitis, but they are not interchangeable. Differences in JAK selectivity lead to meaningful variations in efficacy, speed of response, and safety profiles. By understanding these distinctions and applying the latest clinical evidence, clinicians can make more precise, patient-centered treatment decisions.
As real-world data continue to emerge, ongoing education remains essential to optimize outcomes and ensure the safe, effective use of JAK inhibitors in atopic dermatitis.
News in the same category


6 Powerful Seeds That May Help Reduce Cancer Risk in Seniors – Eat Them Daily for Natural Support
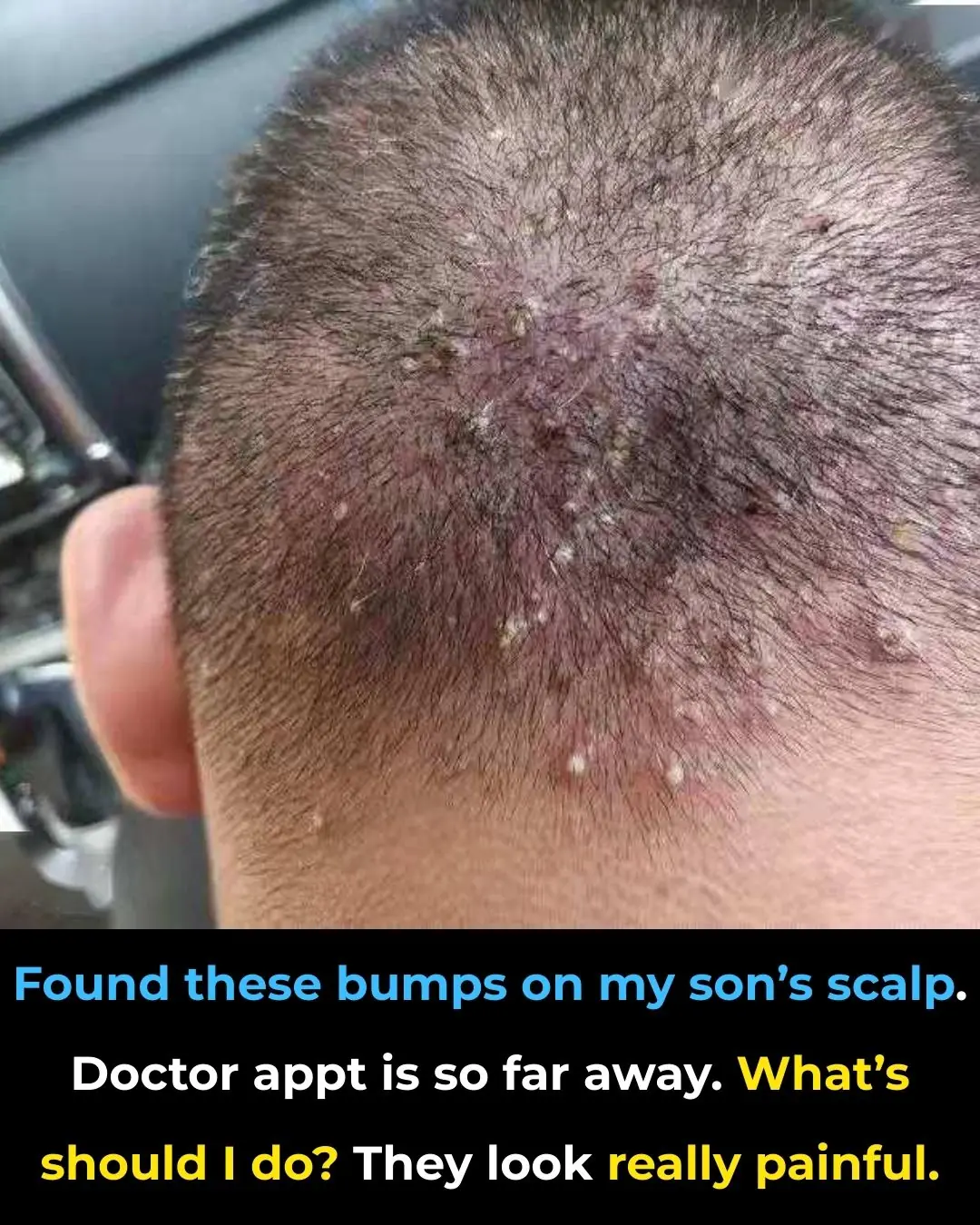
Found these bumps on my son’s scalp. Doctor appt is so far away. What’s should I do? They look really painful

Can Wearable Devices Help Prevent Heart Disease?

A man with kidney failure collapsed in front of the toilet, his wife sobbing: "I advised him many times, but he wouldn't listen."
First Human Trial of Robotic-Assisted Cataract Surgery Reports No Treatment-Related Complications
How daily showers after 65 can do more harm than good

A Common Refrigerator Mistake That Can Spread Bacteria and Make Your Whole Family Sick

Shoulder Pain from Sleeping: Causes, Solutions and More

Top Signs Your Body is Toxic and What to Do About It

How Water Fasting Can Regenerate the Immune System, Slow Aging, Reduce Heart Attack Risk and More
Colon Cleansing With Kefir and Flaxseed Meal
CRISPR-Edited Islet Cell Transplantation: A New Therapeutic Horizon for Type 1 Diabetes

Reversing Alzheimer’s Disease by Restoring Brain Energy Metabolism: Implications of a 2025 Breakthrough Study

Fermented Royal Jelly and Enhancement of Human Mucosal Immunity
Coenzyme Q10 Supplementation and Survival in Chronic Heart Failure: Evidence from the Q-SYMBIO Trial

Vitamin C Status, Fat Oxidation, and Fatigue: Evidence from a Human Metabolic Study

Household Clutter as a Chronic Stressor for Women: Psychological and Physiological Evidence

Why Your Cough Gets Worse at Night — and What to Do About It
News Post

What Happens When You Try Incorporating Papaya Seeds into Your Diet?

6 Powerful Seeds That May Help Reduce Cancer Risk in Seniors – Eat Them Daily for Natural Support
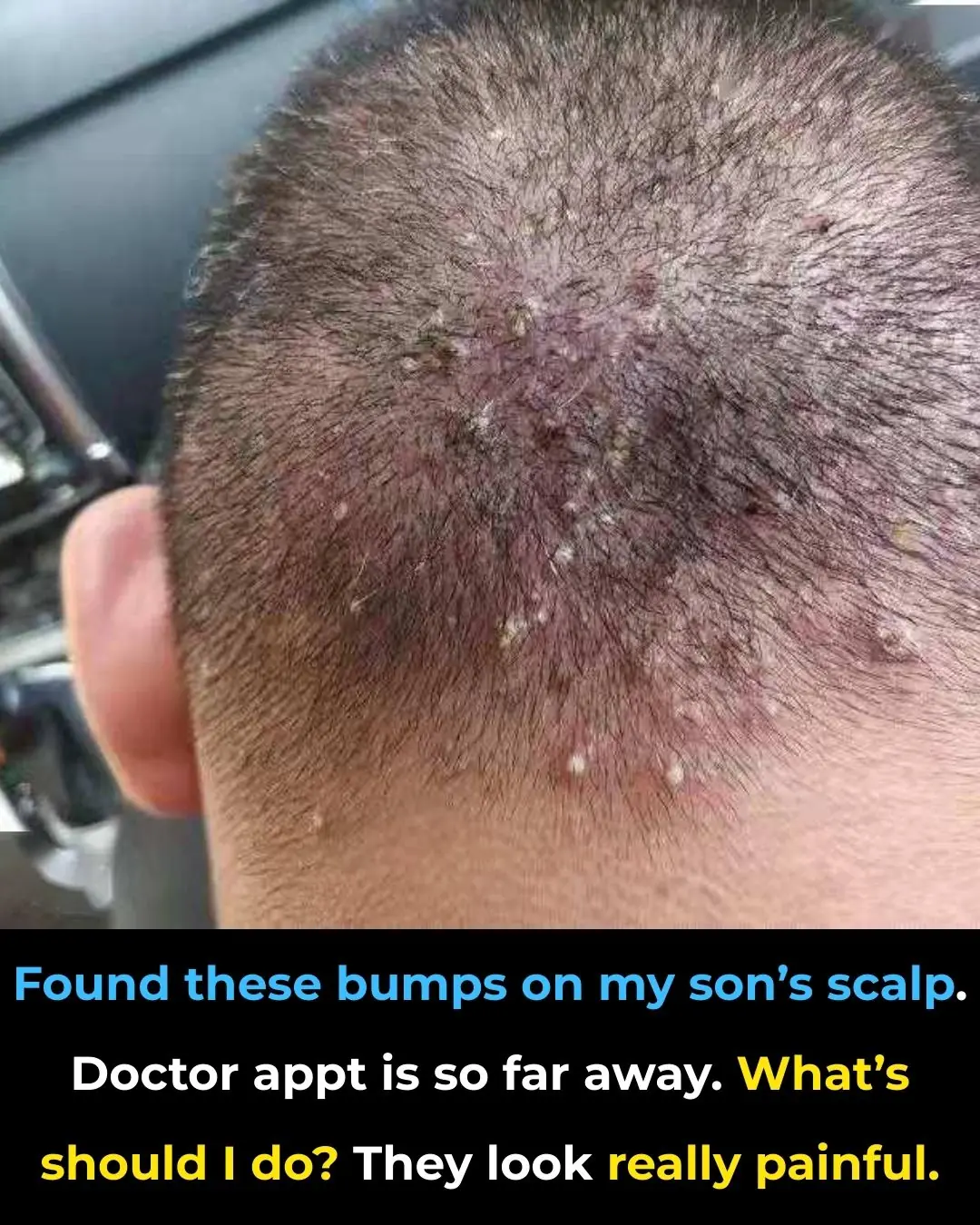
Found these bumps on my son’s scalp. Doctor appt is so far away. What’s should I do? They look really painful

Can Wearable Devices Help Prevent Heart Disease?
Japan’s 108-Year-Old Doctor Swears by This 1-Glass Morning Drink to Empty Your Colon Fast

Discover the Surprising Nutritional Powerhouse: 10 Benefits and Everyday Uses of Purslane

9 Hidden Garlic & Honey Benefits at Night (99% Don’t Know)

A man with kidney failure collapsed in front of the toilet, his wife sobbing: "I advised him many times, but he wouldn't listen."
The Viral T-Shirt That Perfectly Sums Up Married Life

Only People With “Sniper Vision” Can Spot the Squirrel Hidden in This Tree

Only Those with “Sniper Vision” Can Spot the Hidden Squirrel in This Tree

From Mockery to Merit: How a Child’s Creativity Opened the Door to a Full University Scholarship

Deforestation and the Cost of Human Progress: A Wake-Up Call for Environmental Responsibility
7 ways to preserve onions and garlic so they don't mold, rot, or sprout all year round

The UK Launches a Landmark Trial of a Personalized mRNA Lung Cancer Vaccine
UK Plans to Ban Boiling Lobsters and Crabs Alive in Major Animal Welfare Shift

Swallowed While Sleeping: How an AirPod Survived Inside the Human Body
Dark Oxygen in the Deep Sea: How Ocean Floor Rocks Are Redefining the Origins of Life
Too Dangerous for the App Store: The Phone-Throwing Game That Went Viral
