Scientists Regenerate Eyes With Stem Cells Restoring Corneas And Full Vision In Patients

A New Era in Treating Corneal Blindness
For generations, corneal blindness has stood among medicine’s most unyielding challenges. Patients often faced permanent vision loss, limited treatment options, and the emotional toll of losing independence. Traditional corneal transplants could sometimes restore sight, but when the eye’s own stem cells were destroyed, even the most skillful surgeries often ended in disappointment. Worldwide, millions live with this condition, burdened not only by impaired vision but also by chronic pain, scarring, and the daily obstacles that come with visual disability.
That reality, however, is beginning to shift. In Boston, scientists and clinicians have pioneered two groundbreaking approaches that are reshaping what many thought was impossible in eye care. One breakthrough centers on isolating a rare protein marker, ABCB5, which makes it possible to purify the exact stem cells needed to regenerate the cornea. Another approach, called cultivated autologous limbal epithelial cell therapy (CALEC), involves growing new corneal tissue from a patient’s own cells and transplanting it back into the damaged eye. Early results from both strategies suggest that medicine may soon restore the natural healing power of the eye, allowing damaged corneas to repair themselves rather than relying solely on donor tissue.
The Challenge of Corneal Blindness
Corneal blindness affects millions of people globally, often leaving patients with irreversible visual impairment and significant loss of quality of life. The cornea—the clear, dome-shaped surface at the front of the eye—plays a crucial role in focusing light and protecting inner eye structures. When it is damaged by burns, infections, trauma, or autoimmune disease, it can lose transparency, scar over, and cause severe pain.
At the heart of many cases is limbal stem cell deficiency (LSCD). The limbus, a narrow rim encircling the cornea, houses the stem cells responsible for regenerating its surface. If those cells are destroyed, the cornea can no longer heal properly. Standard corneal transplants replace tissue but not the missing regenerative machinery, which is why they frequently fail in patients with LSCD.
Traditional treatments, such as transplanting limbal cells from a patient’s healthy eye or using tissue from deceased donors, have produced mixed results. Success depends heavily on the proportion of true stem cells present in the graft—a factor that, until recently, doctors could not reliably measure. As Harvard researcher Dr. Natasha Frank discovered, transplants worked consistently only when at least 3% of the graft contained actual stem cells. Anything less, and the cornea could not regenerate.
Breakthrough: Identifying the Right Cells
The turning point came when scientists at the Harvard Stem Cell Institute and Massachusetts Eye and Ear identified ABCB5, a protein marker that reliably tags the rare limbal stem cells most capable of regenerating the cornea. This discovery removed the guesswork that had plagued earlier therapies.
In preclinical studies, researchers transplanted purified ABCB5-positive cells into mice with corneal blindness. The results were striking: the corneas regenerated to normal thickness and clarity, and the improvements lasted for more than a year. For the first time, scientists had clear evidence that human adult stem cells could be isolated, expanded, and directed to regenerate an entire tissue.
The implications are vast. A single donor’s stem cells could potentially help restore sight in multiple patients. Biotech companies are now working to scale up production of clinical-grade ABCB5 antibodies, a necessary step before FDA-regulated trials can begin. Though still early, this discovery provides a precise scientific foundation for a therapy that could reach patients in the foreseeable future.
From Bench to Bedside: The CALEC Clinical Trial
While ABCB5 research is still moving toward human testing, another innovation—CALEC therapy—has already reached clinical trials with remarkable success. Developed at Mass Eye and Ear, CALEC involves harvesting a tiny biopsy from the patient’s healthy eye, expanding those cells in a controlled lab environment over several weeks, and transplanting the resulting graft onto the injured cornea. Because the tissue comes from the patient, the risk of rejection is minimal.
A Phase 1/2 clinical trial, published in Nature Communications in March 2025, tested CALEC in 14 patients with severe corneal injuries, including chemical burns. Results were encouraging:
-
79% of patients achieved complete restoration of the corneal surface within one year.
-
By 18 months, over 90% had partial or complete recovery.
-
Visual acuity improved in all participants, with some requiring a second graft for full success.
-
Safety outcomes were excellent, with only one unrelated infection reported.
For individuals who had been told their vision loss was permanent, the results were transformative. Lead investigator Dr. Ula Jurkunas emphasized that the trial demonstrated not just feasibility but consistent efficacy, positioning CALEC as a strong candidate for broader adoption once larger studies confirm the findings.
Why These Advances Matter
The cornea may seem like a simple transparent layer, but biologically, it is dynamic and constantly renewing. When limbal stem cells are destroyed, the surface becomes unstable, scarred, and painfully sensitive. This is why conventional corneal transplants often fail in LSCD patients: they address the damage but not the regenerative engine that maintains clarity.
Both ABCB5-guided transplants and CALEC grafts address the root cause by restoring the regenerative cells themselves. CALEC offers a personalized solution for patients with one healthy eye, while ABCB5-based therapies could eventually help those with bilateral damage by enabling scalable donor-derived treatments.
Remaining Challenges
Despite optimism, challenges remain. CALEC requires at least one healthy eye for biopsy, excluding patients with injuries to both eyes—the most severe cases. Scaling up lab-grown cell therapies to meet FDA standards is complex, costly, and time-intensive. Ensuring long-term stability, affordability, and accessibility will be key hurdles before these treatments can reach the global population in need.
Additionally, ethical and financial questions loom. With intellectual property tied to biotech firms such as OcuCell, Inc., balancing innovation with equitable access will be essential. Policymakers, clinicians, and patient advocates will play a critical role in ensuring that these breakthroughs benefit not only those in wealthy healthcare systems but also patients in lower-income regions where corneal blindness is most common.
Looking Ahead
The rapid progress from basic lab discovery to human trials illustrates the momentum of regenerative medicine. Patients once consigned to permanent blindness are now regaining sight—a change that carries profound emotional and symbolic weight. Restoring vision does not simply improve quality of life; it restores independence, confidence, and human connection.
These breakthroughs are also a testament to persistence in science. The CALEC trial was the culmination of nearly two decades of steady research, while the ABCB5 discovery followed years of painstaking stem cell biology. Together, they remind us that progress often feels slow but can transform lives once it arrives.
For now, patients must temper hope with patience: these therapies are not yet standard of care, and more research lies ahead. But for the millions living with corneal blindness, the message is clear—a future once thought unreachable is now within sight.
News in the same category


The hidden meaning of thumb rings: what they represent for women vs. men

The Small Hole on the Sink: A Feature You Never Knew You Needed
Concerned Woman: Beware of Abandoned Prams on Roadsides!
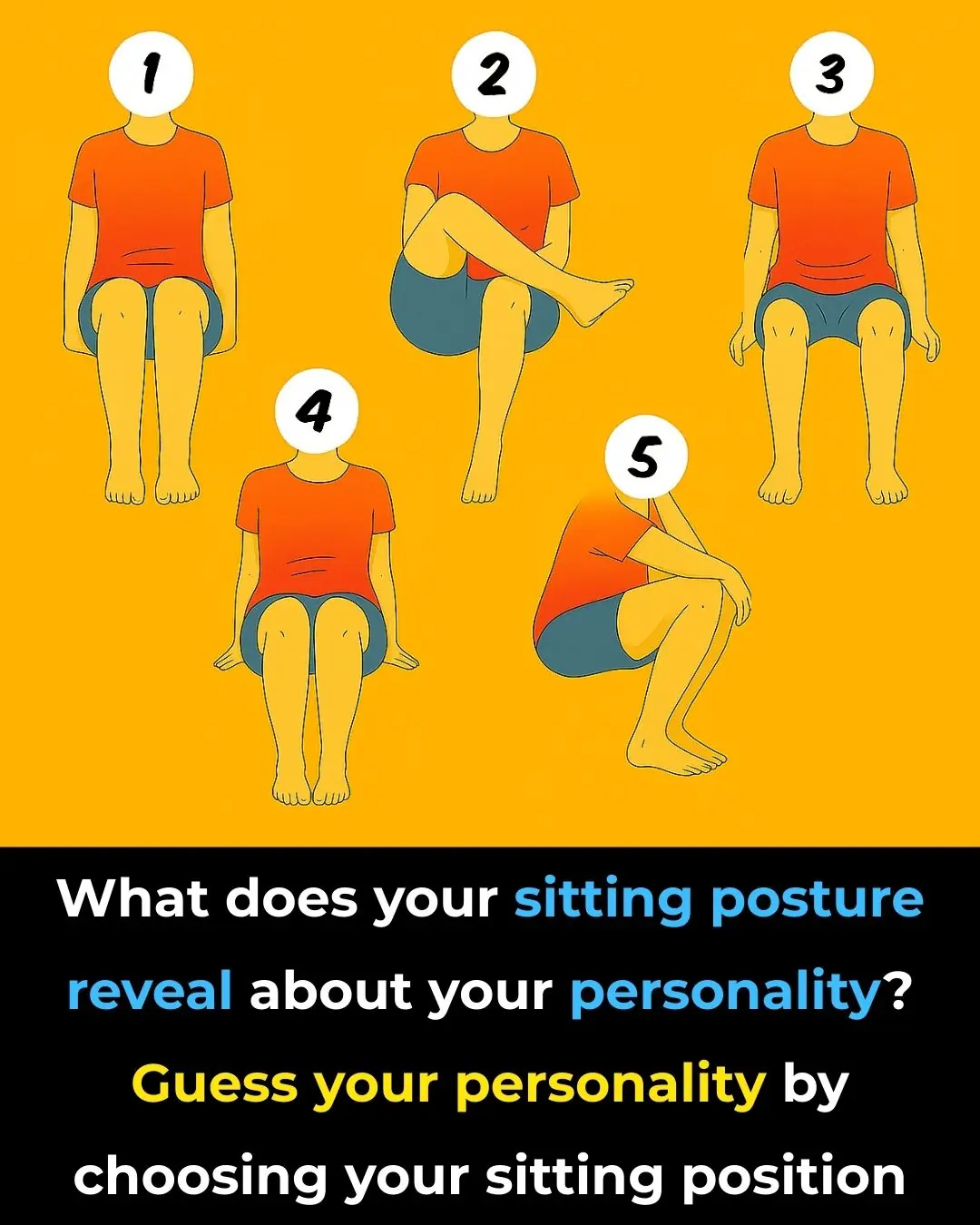
Your Character According to Your Sitting Style

California’s Canals Are Being Covered With Solar Panels To Save Water And Generate Power
Emma Stone explains why not believing in aliens is ‘narcissistic’ as she declares belief in extra terrestrial beings

Damaging effects of new ‘phubbing’ trend that could be ruining your relationship

Japanese airport has never lost luggage in over 30 years – This is why

A Company in Kenya Builds Houses From Recycled Shipping Containers – Solar-Powered and Ready in Days

What Terrible Things Happen When Women Lack Intimacy? A Painful Yet True Reality

Why You Should Never Place Your Bed Like This
Sink Trick You Should Always Do Before Vacation

Elon Musk Issues Serious Warning on Japan’s Population Decline
What it says about your relationship when your partner sleeps with their back to you

Orlando Bloom explains ‘horrible’ side effects his weight-loss transformation caused
A:dult star reveals the clause written into her contract that helps keep her safe

Bear Attack Survivor’s Haunting Farewell Note to Wife After Gathering Pieces of His Own Flesh
Ring Finger Longer Than An Index Finger
News Post
Seniors: Take This for 5 Nights and See What Comes Out in Your Stool!

Clove benefits for Skin – Clove Oil, Clove Gel & Clove ice cubes
The Surprising Benefits of Overnight Tea: A Wasteful Habit You Might Not Know About
How to Clean Limescale Off Your Faucet in Just 25 Seconds with a Simple Trick

How to Clean Your Air Conditioner Easily in Just 15 Minutes — No Technician Needed, Even Women Can Do It Effortlessly

How to Keep Your Non-Stick Pan as Good as New for 3 Years: Simple Tips and Tricks
Using Electric Kettles to Boil Water: 9 Out of 10 Households Make This Mistake — Remind Your Loved Ones to Fix It Early
These 3 types of “acne” on the body could be cancerous; whether male or female, no matter the age, don’t ignore them.

Why Some People Can’t Handle Spicy Food

The hidden meaning of thumb rings: what they represent for women vs. men

The Small Hole on the Sink: A Feature You Never Knew You Needed
🌅 Three Morning Symptoms That Could Be Early Warning Signs of Cancer

Woman shares ’embarrassing’ symptoms she regrets hiding from doctors as she’s diagnosed with incurable cancer
Concerned Woman: Beware of Abandoned Prams on Roadsides!
Your Character According to Your Sitting Style

They say the eyes are the windows to the soul — but what about the mind’s eye?

Should You Eat Rice for Breakfast
Japan has a Lower Rate of Breast Cancer than the U.S. – This Nutrient Makes the Difference
How To Do a 3-Day Sugar Detox to ACCELERATE Fat Loss And Improve Your Mood!