Scientists Say Cancer Can Now Be Detected Years in Advance with Simple Blood Test

Imagine this: You walk into a clinic for a routine blood test and walk out with crucial knowledge — that you might develop cancer years down the line, long before symptoms would ever show.
It might sound like science fiction, but thanks to revolutionary research from Johns Hopkins University, this future is quickly becoming a reality.
In a landmark study published in Cancer Discovery, scientists introduced a blood test that could detect cancer as much as three years earlier than today’s standard diagnostic methods. This represents a potential seismic shift in cancer care — moving the field from late-stage treatment to early-stage prevention.
The Science: How Cancer Leaves Clues in Your Blood
Every cell in the body — healthy or otherwise — sheds tiny fragments of DNA into the bloodstream. But cancer cells leave behind a unique genetic fingerprint in the form of circulating tumor DNA (ctDNA). This ctDNA carries mutations or epigenetic markers that can be distinguished from the DNA of normal, healthy cells.
Leveraging this concept, the team at Johns Hopkins utilized advanced genetic sequencing techniques to comb through these fragments. Their study analyzed 52 stored blood samples — originally collected for unrelated cardiovascular research — from two groups: 26 people who would later develop cancer, and 26 who remained cancer-free.
The tool used was a Multicancer Early Detection (MCED) test, designed to spot early molecular signs of cancer. Remarkably, the test flagged signs of cancer in 8 of the 26 individuals who later received a diagnosis — and in 4 of those cases, clear tumor-linked genetic mutations were already present.
This finding highlights the potential of detecting cancer silently brewing in the body, long before it becomes symptomatic or visible on imaging.
Why Early Detection is a Game-Changer
The earlier cancer is caught, the higher the odds of a full recovery. Localized tumors — which haven’t yet spread — respond far better to treatment and often require less invasive interventions.
For example, according to the American Cancer Society, the five-year survival rate for localized breast cancer is about 99%. That number drops significantly when cancer is diagnosed at a later stage.
As Dr. Yuxuan Wang, the lead researcher, put it:
“Three years earlier provides time for intervention. The tumors are likely to be much less advanced and more likely to be curable.”
Put simply: this test could act like a smoke detector for disease — catching a spark before it grows into a wildfire.
A Field in Motion: Liquid Biopsy and MCED Tests
The technology used in this study is part of a fast-evolving domain known as liquid biopsy — non-invasive tests that detect diseases by analyzing blood, saliva, or other bodily fluids instead of tissue samples.
The idea is simple but powerful: instead of separate screening tests for breast, colon, lung, or cervical cancers, imagine a single blood draw that checks for dozens of cancer types at once.
Commercial efforts are already underway. One of the most prominent is Grail’s Galleri test, backed by biotech giant Illumina. It claims to detect over 50 types of cancer using a single blood sample by identifying abnormal methylation patterns — chemical modifications on DNA that often indicate cancer.
While promising, current MCEDs still face challenges. Tests like Galleri often detect late-stage cancers more reliably than early-stage ones — the latter being the key to saving lives.
The Big Questions: What Happens After a Positive Test?
Despite the excitement, many experts stress caution. A test that says “something is wrong” without identifying what or where introduces a range of complex questions:
-
Should a person undergo biopsies or imaging when there are no visible symptoms?
-
What if the test is a false positive — leading to anxiety, unnecessary procedures, and costs?
-
Or worse, what if it misses a cancer entirely — a false negative?
Dr. Nickolas Papadopoulos, co-author of the study, acknowledges these hurdles:
“We still need to figure out what clinical steps to take once a test result is positive — especially in the absence of a visible tumor.”
Dr. Hilary Robbins, an epidemiologist with the World Health Organization, added:
“Population-wide screening programs must be backed by strong evidence. We need to make sure they do more good than harm.”
The Future: Could This Replace Traditional Cancer Screening?
We’re still far from replacing mammograms, colonoscopies, or Pap smears, but the appeal of a unified, non-invasive cancer test is undeniable.
Tests like MCED offer a potential future where annual blood work could screen for dozens of cancers — much like today’s cholesterol or glucose checks.
Imagine how that could transform access to preventive care, especially in areas where standard imaging equipment is scarce or unavailable. It could also mean fewer invasive biopsies and a reduced reliance on often uncomfortable traditional screening methods.
But for this future to materialize, key questions need answers:
-
How often should such a test be done — yearly, bi-annually?
-
Which cancers are more likely to be picked up early?
-
What are the risks of false positives, and how should they be managed?
-
Can this test adapt to diverse populations across age, race, and genetics?
Scaling the Science: What's Next?
Johns Hopkins researchers plan to expand their study with larger, more diverse participant pools. While the current sample size of 52 is encouraging, it’s not yet enough to change medical guidelines.
Next steps will involve:
-
Validating the findings with thousands of participants
-
Testing the effectiveness across multiple cancer types
-
Refining the sensitivity to catch even smaller tumors
-
Collaborating with regulatory bodies like the FDA to ensure safety and accuracy
If successful, this test could become part of routine annual physical exams, changing the way primary care physicians screen for and address cancer risk.
A Glimpse Ahead: Hope Meets Caution
We are on the brink of a major turning point in oncology. This isn’t just a new test — it’s a new philosophy of care: one rooted in prevention, personalization, and early action.
As Dr. Bert Vogelstein, a giant in cancer genomics and senior figure in the study, concluded:
“This study shows the promise of MCED tests in detecting cancers very early, and sets the benchmark sensitivities required for their success.”
Still, researchers, clinicians, and policymakers agree: more work remains before such tests can be trusted on a wide scale. But if done right, they could revolutionize how we live, how we’re monitored, and ultimately — how long we survive.
In Summary: The Promise of the Invisible Fight
With every drop of blood, our bodies tell a story. What researchers at Johns Hopkins have shown is that, sometimes, that story starts before the first symptom ever appears. The dream of catching cancer before it becomes cancer is inching closer to reality.
Soon, a routine visit to your doctor could silently screen for life-threatening diseases — giving you not just information, but time. And in the world of cancer, time is everything.
News in the same category

Dogs Able to Sniff Out Parkinson’s Before Symptoms Appear

14 hidden causes of tingling feet (and what to do)
At last — how to detox the brain naturally

5 Blood Clot Facts Doctors Want You to Know

8 Foods That Help Lower Your Cholesterol
6 Harmful Foods That Weaken Calcium Levels

How to Use Castor Oil to Regrow Eyelashes and Eyebrows

Scientifically Proven Health Benefits of Avocado and Avocado Seeds
Experts Say They’ve Pinpointed the Cause of Autism—And It Could Lead to New Treatments

Final straw that led to billionaire CEO's desperate escape from Japan inside 3ft box

10 Early Warning Signs Your Blood Sugar Is Way Too High

If Your Legs Cramp at Night You Need to Know This Immediately

Warning Signs Your Body Is Full of Parasites and How to Effectively Eliminate Them Naturally

Warning Signs of a Parasite Infection And How to Eliminate It for Good

What Raw Garlic Can Do for Your Health Is Truly Unbelievable
Diabetes Tied to Slower Brain Recovery After TBI
Neuropathic Pruritus Has High Comorbidity Burden, Varied Treatment Responses
News Post
Eating More Cruciferous Vegetables May Cut Colon Cancer Risk

Dogs Able to Sniff Out Parkinson’s Before Symptoms Appear

14 hidden causes of tingling feet (and what to do)
At last — how to detox the brain naturally

5 Blood Clot Facts Doctors Want You to Know

8 Foods That Help Lower Your Cholesterol
6 Harmful Foods That Weaken Calcium Levels

8 Common Reasons For Waking Up at Night

How to Use Castor Oil to Regrow Eyelashes and Eyebrows

Scientifically Proven Health Benefits of Avocado and Avocado Seeds
Experts Say They’ve Pinpointed the Cause of Autism—And It Could Lead to New Treatments

You Can Adopt Puppies That Were ‘Too Friendly’ to Become Police Dogs

A Nigerian Scientist Developed a High-Tech Cancer-Detecting Goggles That Help Surgeons Spot Cancer Cells More Accurately.

Final straw that led to billionaire CEO's desperate escape from Japan inside 3ft box
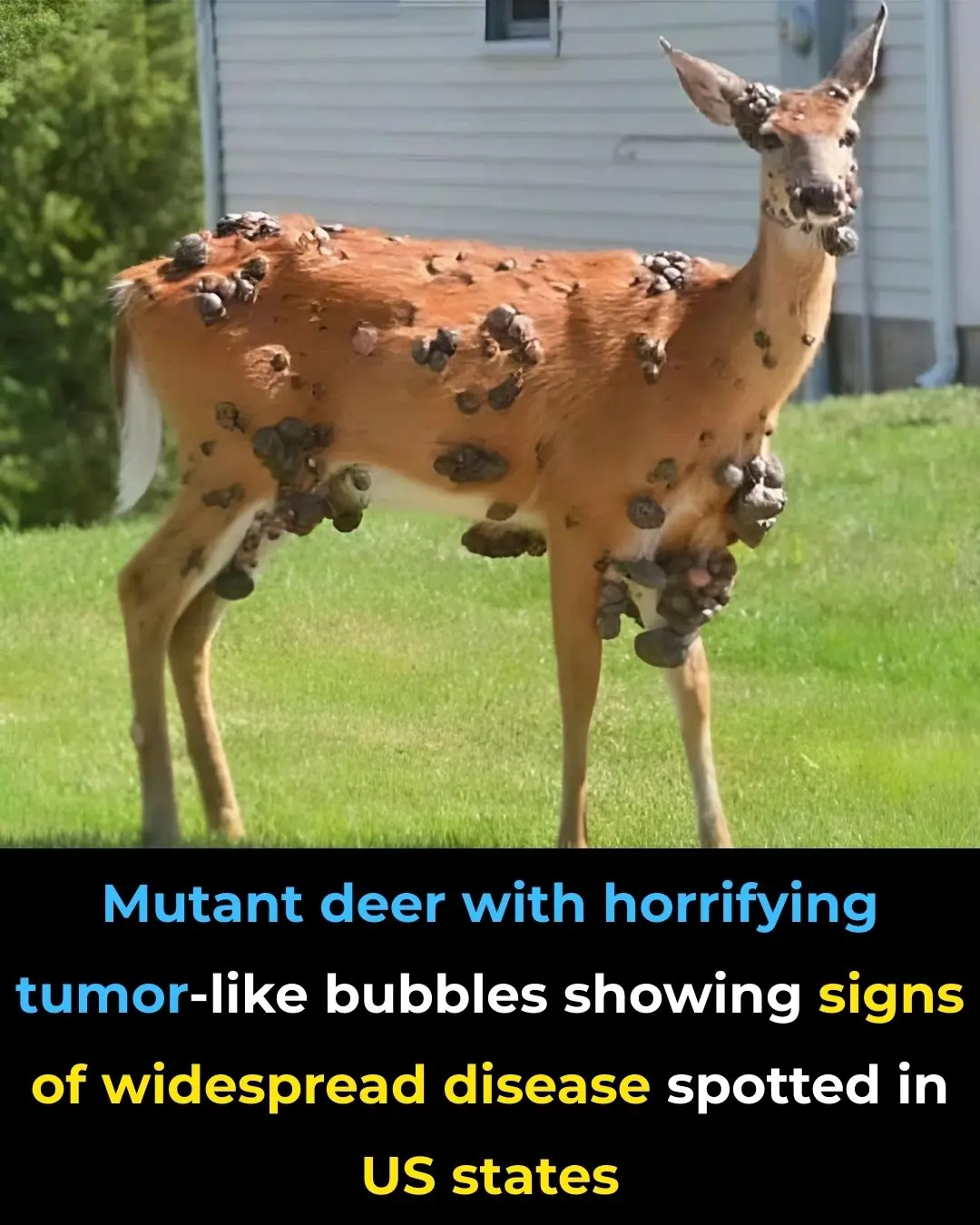
Mutant deer with horrifying tumor-like bubbles showing signs of widespread disease spotted in US states

'Frankenstein' creature that hasn't had s3x in 80,000,000 years in almost completely indestructible

Scientists discover ultra-massive 'blob' in space with a mass of 36,000,000,000 suns
When a Washing Machine Shows 7kg, 8kg, or 10kg, Is That the Weight of Dry or Wet Clothes? The Real Meaning Behind These Numbers Is Something That Few People Know
