Signs of Arthritis You Shouldn’t Ignore

Living with arthritis means learning to navigate daily discomfort and adapt to the changing needs of your body. Over time, you may have learned when to rest, when to keep moving, and when to reach out for support. But what happens when symptoms begin to change—when they go beyond the typical aches, stiffness, and fatigue?
Sometimes, what seems like a minor issue—such as unexplained exhaustion or gradual weight loss—can actually be a sign of something more serious happening inside your body. That’s why it’s important not to dismiss new or worsening symptoms as just "part of aging" or "a bad week."
Below are 7 key signs of arthritis that should never be ignored, and guidance on when to speak with a healthcare professional.
1. Persistent Joint Pain
Joint pain is one of the most recognizable and common symptoms of arthritis. It may start subtly—perhaps a dull ache after walking or climbing stairs—but can slowly worsen over time. You might notice that pain increases after physical activity or becomes more pronounced at night or upon waking.
In rheumatoid arthritis (RA), the pain can feel deep, intense, and at times unpredictable—like a broken bone or heavy bruising. This pain is often symmetrical, affecting both sides of the body equally, such as both knees or both wrists.
When to see a doctor: If joint pain persists for more than two to three weeks, or worsens without an identifiable cause (such as an injury), it’s time to seek medical evaluation. Early diagnosis can prevent long-term joint damage.
2. Joint Swelling and Tenderness
Swelling is a red flag, particularly if it's recurrent or persistent. You might observe:
-
Puffiness around joints
-
Warmth to the touch
-
Redness or discoloration
-
Sensitivity or tenderness when pressing on the joint
This often indicates inflammation, which, if untreated, can accelerate joint damage and deformity. Inflammatory arthritis, like RA or psoriatic arthritis, often causes swelling that comes and goes—or flares—without a clear trigger.
When to see a doctor: Don’t wait if swelling interferes with movement or daily tasks like walking, writing, or gripping objects. Prompt attention is key to reducing long-term complications.
3. Morning Stiffness Lasting More Than 30 Minutes
Most people experience some stiffness upon waking, but if it lasts longer than 30 minutes, it could indicate inflammatory arthritis.
-
Osteoarthritis usually causes stiffness that fades within 30 minutes as you start moving.
-
Rheumatoid arthritis, by contrast, may cause stiffness that lingers for an hour or more, sometimes into the afternoon.
This kind of stiffness typically improves with movement, which helps distinguish it from other causes like injury or inactivity.
Pro tip: Stiffness that improves throughout the day but returns in the evening—or after sitting for long periods—is another red flag worth discussing with your doctor.
4. Grinding, Cracking, or Popping Sounds (Crepitus)
Hearing or feeling a grinding, clicking, or popping sound when moving your joints can signal cartilage deterioration. As the protective cartilage wears away (as in osteoarthritis), bones begin to rub against each other, leading to crepitus.
While some joint noise is normal with aging or after exercise, persistent or painful crepitus—especially if paired with reduced mobility—is more concerning.
When to see a doctor: If joint sounds are accompanied by swelling, pain, or reduced function, a medical evaluation is recommended. Imaging such as X-rays or MRIs can help assess the extent of cartilage damage.
5. Reduced Range of Motion
Do you struggle to fully straighten your arm or bend your knee? Loss of joint mobility—whether from pain, swelling, or structural changes—is a classic sign of progressive arthritis.
Common causes include:
-
Inflammation tightening surrounding tissues
-
Cartilage loss limiting joint flexibility
-
Joint deformities or bone overgrowth (common in advanced osteoarthritis)
When to act: If your joint feels "stuck," you avoid certain movements due to pain, or your flexibility is noticeably declining, don’t delay. Early physical therapy or treatment may help restore function.
6. Referred or Deferred Pain
Arthritis pain doesn’t always show up where you’d expect. Pain in one area of the body may actually stem from joint inflammation elsewhere. This is known as referred pain.
Examples include:
-
Hip arthritis causing pain in the groin, thigh, or even knee
-
Foot arthritis radiating discomfort to the lower back or hips
-
Spinal arthritis causing pain that shoots down the legs or feels like sciatica
Why it matters: Misdiagnosed referred pain can lead to ineffective treatment or delayed care. If pain feels "weird," migrates, or doesn’t match your movement patterns, let your doctor know.
7. Unexplained Fatigue
Chronic fatigue is more than just being tired. It can feel like a complete energy drain—mentally, emotionally, and physically. Even after a full night’s sleep, you may wake up exhausted.
Fatigue can be caused by:
-
Chronic inflammation (which overworks the immune system)
-
Poor sleep quality due to joint pain
-
Depression or anxiety linked to chronic illness
-
Decreased activity, leading to muscle weakness and reduced stamina
Fatigue is especially common in autoimmune arthritis, such as RA, lupus, or ankylosing spondylitis.
What to monitor: If your energy levels are affecting your work, relationships, or basic tasks, it’s time to take this seriously and get support.
What to Do If You Suspect Arthritis
Early diagnosis is crucial. Arthritis is a progressive condition, meaning it tends to worsen over time. But catching it early allows for more effective management—and in some cases, even remission.
Common treatment options include:
-
Medications: Anti-inflammatories, DMARDs, corticosteroids, and biologics
-
Physical therapy and guided exercise
-
Topical treatments: Drug-free gels like FlexiSEQ that lubricate joints and reduce stiffness
-
Lifestyle changes: Anti-inflammatory diet, weight management, stress reduction
-
Alternative therapies: Acupuncture, massage, tai chi, and mindfulness
You don’t have to “just live with it.” There are many tools available to help you maintain your independence and reduce pain.
Final Thoughts
Arthritis is not a one-size-fits-all condition. It affects people differently and often progresses silently before making a significant impact. That’s why it’s important to listen to your body—and act when something doesn’t feel right.
Don’t ignore persistent joint symptoms, unusual pain, or ongoing fatigue. When in doubt, consult with your primary care doctor or a rheumatologist. The sooner you get answers, the better your chances of living well with arthritis.
News in the same category


Seniors: the 1 simple ingredient that quickly rebuilds muscle
Doctors warn: this 1 cancer sign may show up in your sheets
How Water Fasting Can Regenerate the Immune System, Slow Aging, Reduce Heart Attack Risk and More
4 Reasons Why Cardiac Arrests Happen in The Bathroom
Shoulder Pain from Sleeping: Causes, Solutions and More
Cancer hates these 6 fruits—eat them to fight back!

Canadian Researchers Discover New Evidence That Vitamin D Shuts Down Cancer Cells

Research Reveals Two Life Stages of Accelerated Aging

9 Convincing Reasons to Consume More Dates

Unlocking the Hidden Potential of Papaya Seeds: A Nutritional Treasure

Garlic & Black Pepper: The Kitchen Cure for Leg Pain and More

Castor oil for older adults: key benefits and safety tips you shouldn’t miss

Top 10 signs of a gallbladder attack

Which fruit prevents cancer cells from growing rapidly?
Does The Inside Of Your Ear Itch
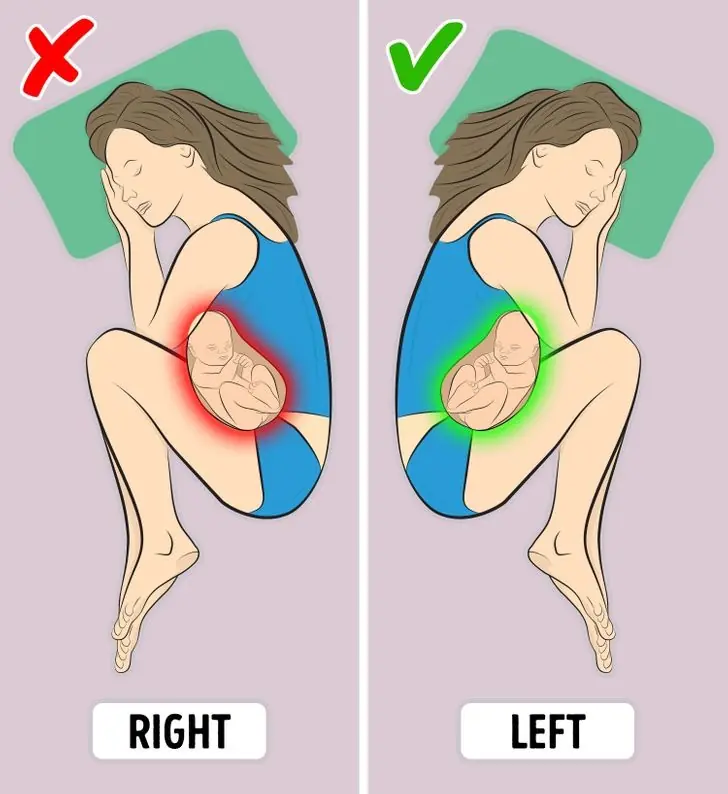
Disadvantages of Sleeping on Your Right Side: What Your Body Isn’t Telling You

A Natural Remedy for Thinning Hair

Simple Aloe Vera Trick Will Leave Your Skin Glowing
News Post

The fish that is the "king of omega-3," with salmon only ranking second: Sold everywhere in Vietnamese markets at incredibly low prices.

Tips for using rice water and ginger to nourish your hair, promoting faster growth and making it thicker, darker, and shinier.

Treat premature gray hair with a black dye formula made from sour starfruit and potatoes, as cheap as can be!
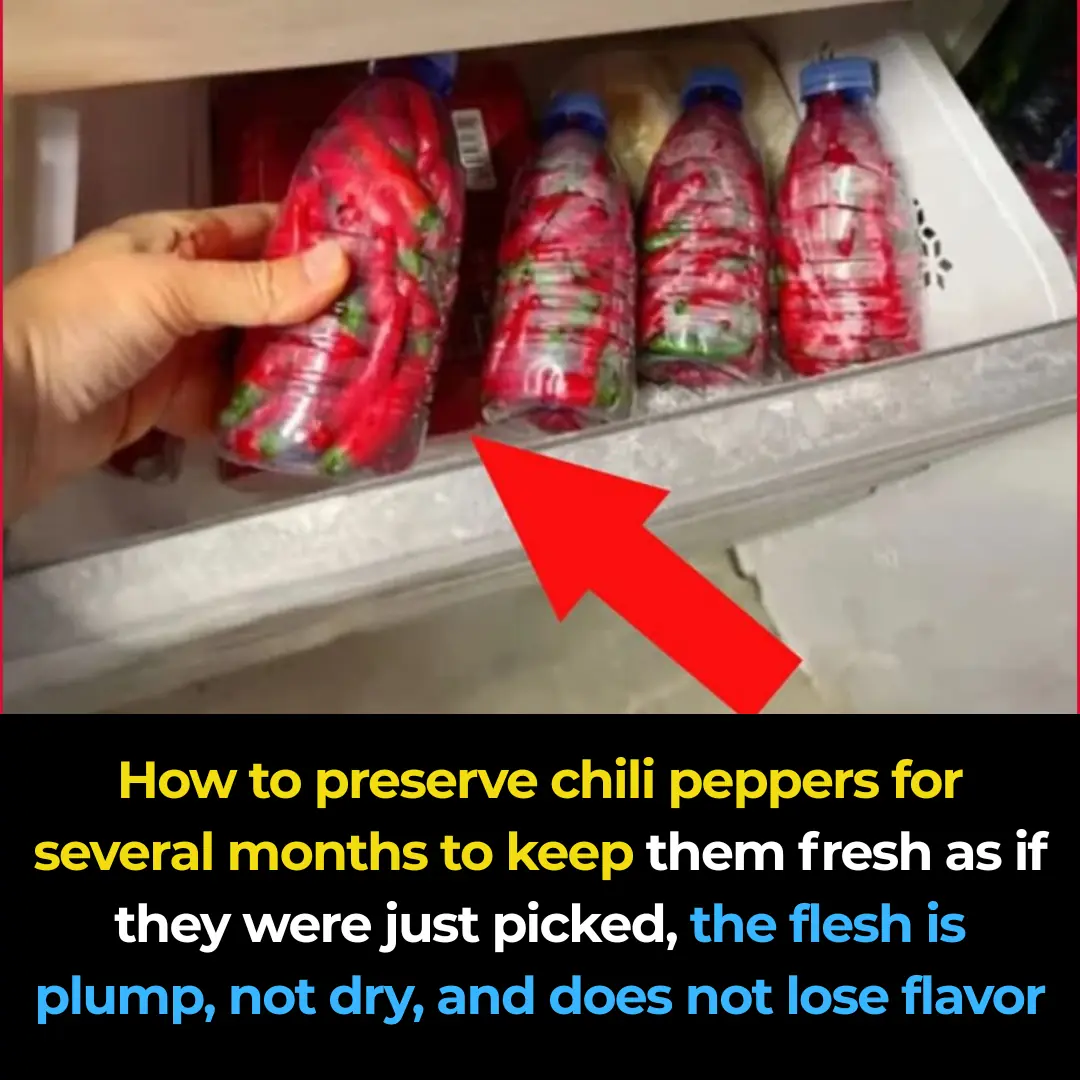
How to store chili peppers for months while keeping them as fresh as the day they were picked, with firm, plump flesh that doesn’t dry out or lose flavor.
10 people eat avocado, but 9 of them discard this part without realizing it's a "treasure."
How to help you travel thousands of miles without getting motion sickness.
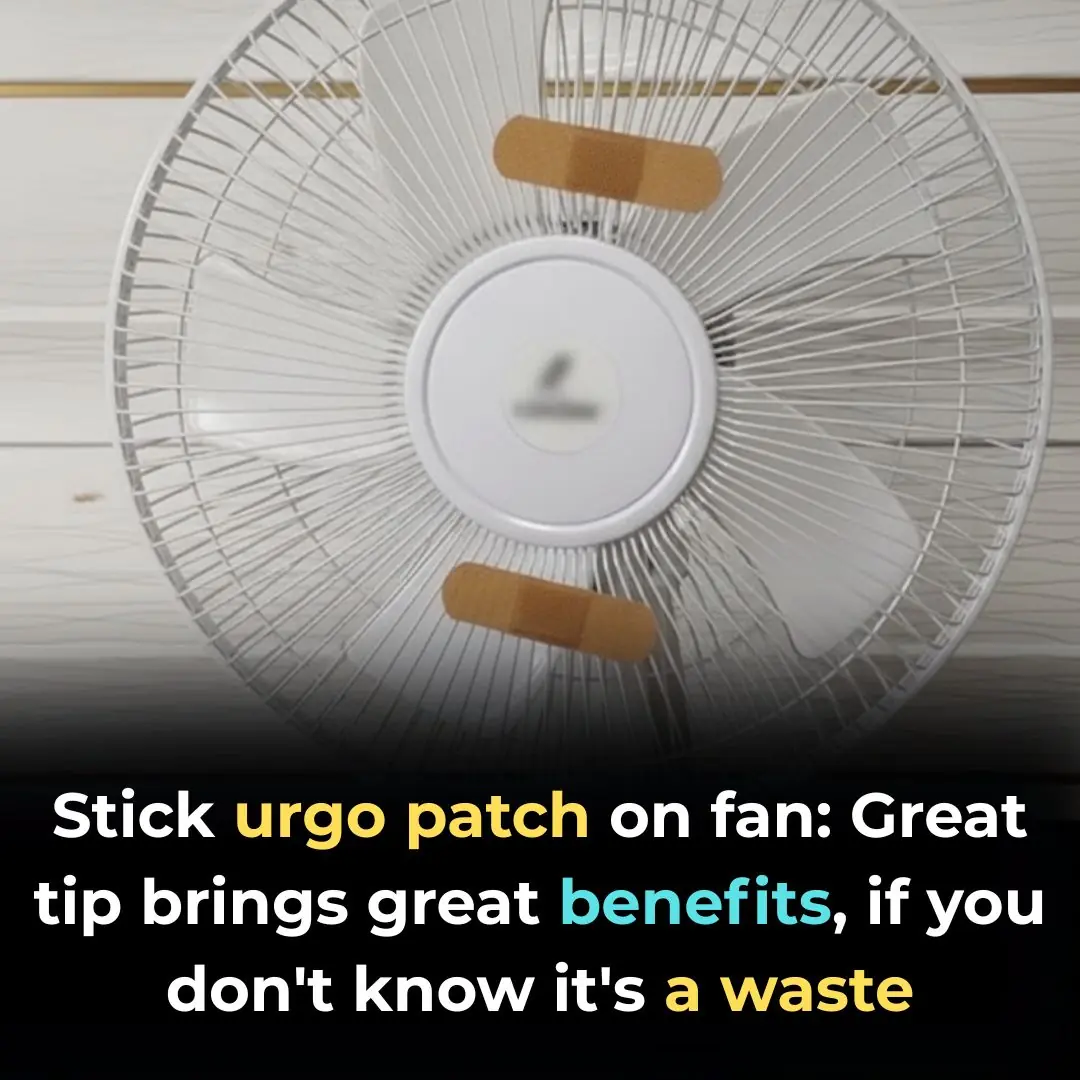
Stick an Urgo Patch on Your Fan: A Clever Trick That Brings Amazing Benefits—Don’t Miss Out if You Haven’t Tried It

Tips to Prevent Blackening of Pots When Using a Gas Stove: Very Simple, Everyone Should Know

Drink coffee THIS way to protect and reverse liver damage caused by alcohol

Seniors: the 1 simple ingredient that quickly rebuilds muscle
Doctors warn: this 1 cancer sign may show up in your sheets

Don’t Throw Away Bubble Wrap — Keep It in Your Kitchen to Discover These Amazing Benefits

Revive Your Nails with This Garlic Secret
17 Natural Habits to Keep Your Colon Healthy
7 Nettle benefits and uses

7 Benefits Of Papaya Seeds & How To Consume Them Correctly
How Water Fasting Can Regenerate the Immune System, Slow Aging, Reduce Heart Attack Risk and More
4 Reasons Why Cardiac Arrests Happen in The Bathroom
Shoulder Pain from Sleeping: Causes, Solutions and More