Stop blood sugar spikes—enjoy carbs without the crash!

You’re definitely not alone. Many people notice big swings in energy, cravings, or mood after meals and worry that their favorite carb-rich foods might be harming their long-term health. But here’s the good news: you don’t need to swear off bread, rice, fruit, or potatoes to keep your blood sugar steady. With a few smart strategies, you can continue enjoying the foods you love while avoiding the spikes that leave you feeling drained.
Blood sugar spikes occur when glucose levels rise to 180 mg/dL or higher after eating. They’re more common in people with diabetes or prediabetes, but they can also happen in people who don’t have these conditions—especially as they get older, carry extra weight, or live an inactive lifestyle. Keeping your blood sugar within a healthy range (ideally 70–140 mg/dL) is one of the most important steps you can take for metabolic and overall health. And the best part? You can prevent many of these spikes without cutting carbs.
I’m 51, and with a strong family history of obesity and type 2 diabetes, I’m aware of my risks. Yet my average blood sugar stays between 80 and 120 mg/dL—all while eating plenty of the usual carb suspects: bread, potatoes, rice, and fruit. The secret is not avoiding carbs altogether but understanding how to pair and prepare them. Drawing on the expertise of nutrition scientist Mario Kratz, PhD, here are six practical, science-backed strategies that actually work.
6. Minimize High Glycemic Index Foods
The glycemic index (GI) measures how quickly a food raises your blood sugar. High-GI foods—like white rice, corn flakes, white toast, or sugary drinks—cause fast, sharp spikes that can leave you feeling tired, jittery, or hungry soon after.
As a general guideline, try to limit foods with a GI above 60. You don’t need to eliminate them entirely, but choosing lower-GI alternatives can make a big difference:
-
Swap corn flakes for steel-cut oats
-
Replace white bread with sourdough rye
-
Choose sweet potatoes instead of white rice
Even if the carb amount stays the same, these swaps can dramatically reduce your glucose response. I’m not strict about it 100% of the time, but whenever I eat a higher-GI food, I always apply at least one of the other strategies below to help stabilize the impact.
5. Eat Starchy Foods After Retrogradation
“Retrogradation” sounds technical, but the idea is beautifully simple.
When you cook starchy foods—like rice, pasta, or potatoes—the starch is easy for your body to break down. But once these foods are cooled, especially overnight in the fridge, some of the starch transforms into resistant starch.
Why this matters:
-
Resistant starch acts more like fiber, not sugar
-
It slows digestion
-
It feeds beneficial gut bacteria
-
Your blood sugar rises 20%–40% less after eating it
This trick is effortless to use. I always cook extra potatoes or rice, refrigerate them, and incorporate them into meals the next day—like potato salad, fried rice, or hash browns. And yes, reheating them still keeps most of the resistant starch intact.
4. Don’t Eat “Naked” Carbs
“Naked carbs” refer to carbs eaten by themselves—without enough protein, fat, or fiber to slow digestion.
Examples:
-
Corn flakes with just milk
-
Jam on white bread
-
Instant oatmeal
-
Pasta with little else
These foods hit your bloodstream fast because there’s nothing to moderate their absorption.
But when you add protein, fat, or fiber, your body digests the meal more slowly, leading to a gentler rise in blood sugar. Here are great add-ons:
Protein: eggs, yogurt, cheese, chicken, fish, tofu, beans
Healthy fats: nuts, seeds, avocado, olives, olive oil
Fiber: leafy greens, broccoli, onions, cabbage, Brussels sprouts
For instance, if your go-to breakfast is white toast with jam, adding just two eggs can cut your blood sugar spike almost in half. I’ve seen this firsthand: one night I ate bread, ham, and cheese, and my glucose hit 170 mg/dL. Another night, I ate the same meal but added two boiled eggs—and my blood sugar barely rose.
A high-carb meal paired with non-starchy vegetables can make an even bigger difference. Think mashed potatoes + sauerkraut + smoked pork—a meal that kept my post-meal glucose around 120 mg/dL, thanks to protein, fat, and fiber.
3. Add Some Vinegar
Vinegar is one of the simplest, most researched tools for reducing post-meal glucose spikes.
Studies show that 2 tablespoons of vinegar, diluted in water right before a carb-heavy meal, can significantly blunt the blood sugar rise. But instead of drinking vinegar directly—which can irritate your teeth and throat—use it in food:
-
A small salad with vinaigrette
-
Pickled vegetables
-
Vinegar-based dressings
Any vinegar works—apple cider, red wine, white wine, rice vinegar—it’s the acetic acid that makes the magic happen.
Once, I ate leftover mashed potatoes with caramelized onions and sauerkraut. Because I no longer had the pork from the previous night, I added a small salad with vinaigrette. The result? My blood sugar only rose less than 20 mg/dL, thanks to the vinegar, the sauerkraut, and the resistant starch in the cooled potatoes.
2. Use the Second Meal Effect

The second meal effect is a fascinating metabolic phenomenon:
What you eat at one meal affects your blood sugar response at the next meal.
Example:
Eating carbs at lunch can help your body handle carbs more effectively at dinner. If someone eats the same high-carb dinner two days in a row, their blood sugar might rise more on the day they had a low-carb lunch.
Why?
Your body becomes more efficient when it’s accustomed to processing carbs.
This means:
-
If you eat low-carb, try to stay consistent rather than switching back and forth.
-
High-fiber or high-protein meals have carryover benefits.
-
A balanced breakfast can improve blood sugar control at lunch.
So if you plan to enjoy a big carb-heavy dinner, it may help to include some carbs, protein, and fiber at lunch instead of going low-carb all day.
1. Go on a Walk After the Meal
This is one of the most effective strategies of all—based on simple biology.
Your muscles can absorb glucose without insulin when they’re active. Even a short walk after meals helps clear glucose from your bloodstream.
-
Start walking within 30 minutes of finishing your meal
-
A 10–15 minute walk is good
-
For big carb-heavy meals, longer walks are even better
I tested this myself. After eating a ton of cake and cookies one Christmas morning, my blood sugar hit 190 mg/dL. But the next day, I ate the same sweets—this time adding a boiled egg first and taking a 60-minute walk afterward. My glucose peaked at 140 mg/dL, a full 50 mg/dL lower.
Even when I ate chips and bread on a four-hour drive (and spiked to 170 mg/dL), recreating the same meal with a walk kept my glucose around 150 mg/dL.
Movement matters. A little goes a long way.
Summary
Minimize High-GI Foods
Avoid foods with a GI over 60—or pair them with other strategies.
Eat Cooled Starches
Cook, cool, and reuse starchy foods to increase resistant starch.
Don’t Eat Naked Carbs
Always pair carbs with protein, fat, and vegetables.
Add Vinegar
Use vinaigrette or pickled foods to reduce glucose spikes.
Use the Second Meal Effect
Your previous meal shapes your next glucose response.
Walk After Meals
A short walk can dramatically reduce blood sugar spikes.
The Root Cause of Blood Sugar Spikes: Glucose Intolerance
While all these strategies help, persistent blood sugar spikes usually indicate some level of glucose intolerance—your body isn’t efficiently managing glucose on its own.
These techniques can definitely:
-
reduce spikes
-
improve average blood sugar
-
support weight and energy management
But achieving completely normal blood sugar levels often requires improving underlying glucose metabolism, which involves broader lifestyle approaches such as strength training, improving sleep, managing stress, and addressing diet quality.
This is a big topic—larger than this article—but recognizing early signs of glucose intolerance is the first step toward preventing or managing conditions like prediabetes and type 2 diabetes.
News in the same category


Scientifically Proven Benefits of Pumpkin Seeds (Pepitas) and Pumpkin Seed Oil

The single move that instantly clears congestion and drains your sinuses

11 Health Warnings Your Fingernails May Be Sending
The most powerful anti-cancer food you’ve probably never tried

🩺 Be Aware: If You Notice This Skin Change, It Could Be Skin Cancer — Here’s What to Look For

Gastroenterologist says this is the #1 drink for gut health
What your body does when you drink coffee every day

The 5 best supplements to soothe nerve pain and tingling

Doctor says this is the #1 supplement to take if you have arthritis
Stop blood sugar spikes—enjoy carbs without the crash!

Gastroenterologist says this is the #1 drink for gut health

6 Types of Warts (Signs, Symptoms, Home Remedies, and Treatment)

Many experts warn that this food may increase health dangers — stop eating it now!
Gentle Stretches to Relieve Sciatica Pain
93% of people won’t do this yet it lowers blood pressure quickly

What Happens to Your Body When You Eat Canned Tuna Every Day
This Tropical Fruit Could Help Protect Your Liver and Fight Cancer

6 Foods You Absolutely Need To Avoid If You Suffer From a Thyroid Disorder
News Post

Here’s the secret why everyone puts avocados on the fire!

Grow Date Trees From Seed (Start in a Pot → Plant Outdoors): The Complete, No-Stress Guide

Guava Leaves for Blood Sugar Control: Nature’s Gift for Diabetics
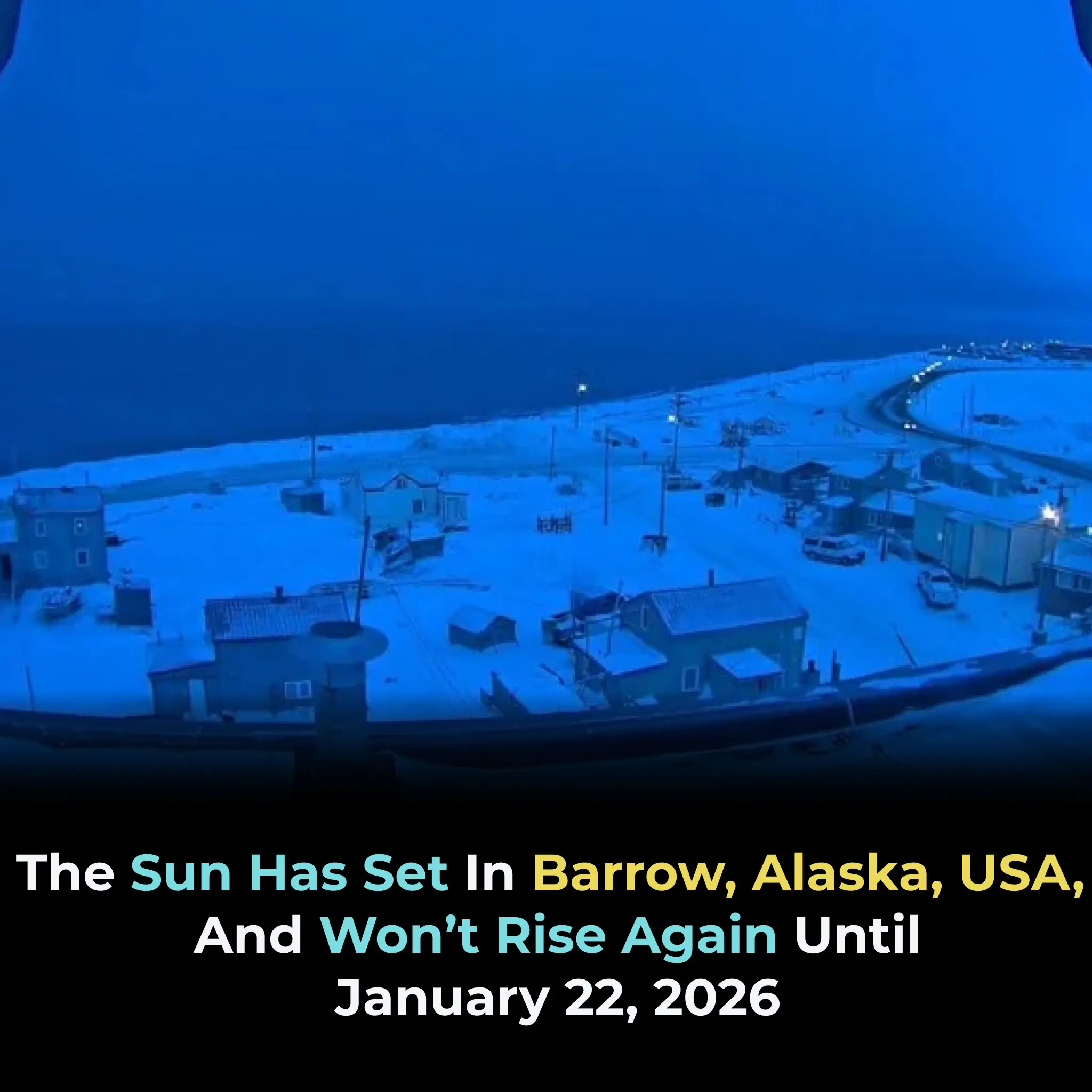
Utqiagvik Enters 64 Days of Darkness: Inside Alaska’s Annual Polar Night
The Versatility and Benefits of Orange Peel Powder

Here’s the secret why everyone puts avocados on the fire!

Natural Biotin Powder: Get New Hair in Bald Patch, Extreme Hair Growth
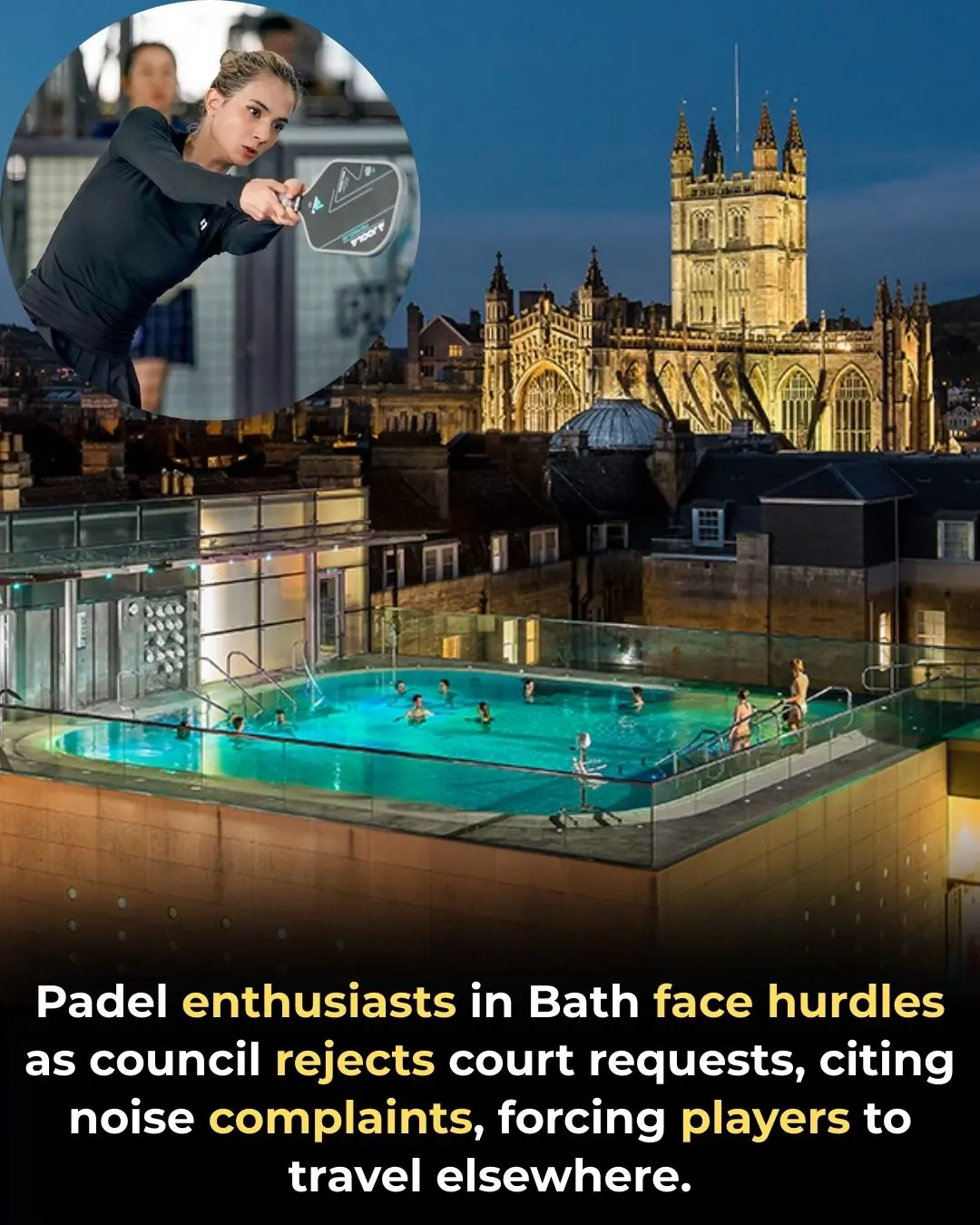
Community Backlash Stops Padel Court Plans in Bath Amid Rising Demand

Scientifically Proven Benefits of Pumpkin Seeds (Pepitas) and Pumpkin Seed Oil
26 Years, 214 Countries, 900,000 Kilometers: The Epic Journey of Gunther and Christine

My nana taught me this hack to get rid of dark circles in 5 mins with 0 work. Here’s how it works

The single move that instantly clears congestion and drains your sinuses
Put a cotton ball with VapoRub in your ear & get this remarkable effect
A Drink That May Help Reduce Cancer Risk: Not Tea or Coffee

Tips for preserving ginger without refrigeration

11 Health Warnings Your Fingernails May Be Sending
Whether It’s AA or AAA, Don’t Throw Them Away When They Run Out — Here’s a Simple Way to Revive Batteries in 10 Seconds

If the fan is dirty, you don't need to remove the frame or use water

Placing a Sock on Top of Your Air Conditioner: A Small Trick With Big Benefits—Especially on Scorching Days