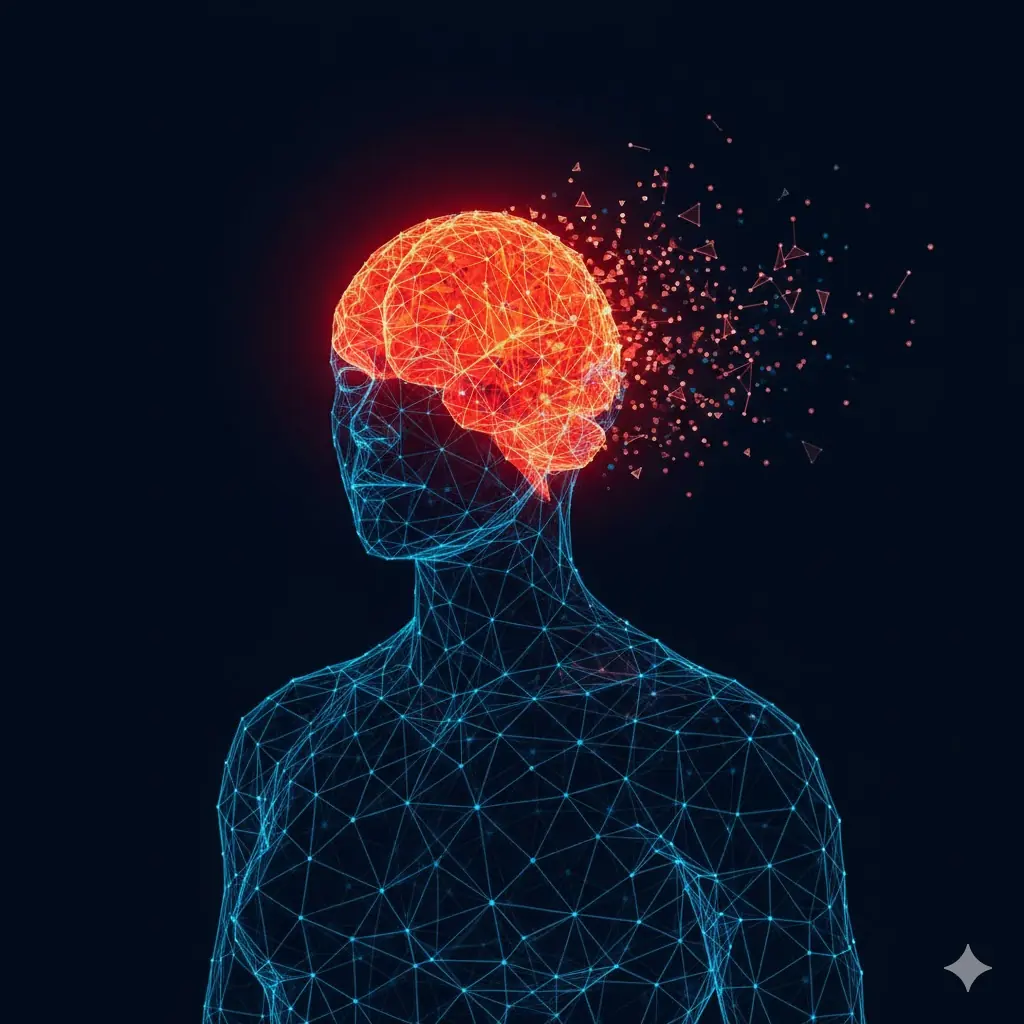
Surprise Finding: How the Immune System May Prevent Us From Burning Fat
For decades, the immune system and metabolism were studied as largely separate biological systems. Immunity was seen as the body’s defense against infection, while fat tissue was viewed mainly as an energy storage depot. However, a groundbreaking study published in Nature reveals that these two systems are far more intertwined than previously thought. Remarkably, the same white blood cells that rush to fight infections may also act to limit fat burning, preserving energy stores in times of scarcity.
This newly identified immune–metabolic partnership may have been essential for human survival during famine, but in today’s calorie-rich environment, it could be contributing to obesity and metabolic disease.
The Evolutionary Logic Behind Fat Preservation
From an evolutionary perspective, the ability to conserve fat was critical. For much of human history, food availability was unpredictable, and long periods of scarcity were common. Any biological mechanism that prevented excessive fat loss would have offered a powerful survival advantage.
The new research suggests that certain immune cells evolved not only to protect against pathogens but also to signal fat tissue to slow down energy release during times of stress or illness. Infections increase energy demands, and preventing rapid fat depletion may have helped ensure survival through prolonged challenges.
White Blood Cells With a Dual Role
The study focused on specific types of white blood cells—particularly immune cells found within adipose (fat) tissue. These cells, traditionally studied for their role in inflammation and immune defense, were shown to directly interact with fat cells.
Key Findings From the Study
-
Immune cells in fat tissue release signaling molecules that suppress lipolysis, the process by which stored fat is broken down and used for energy
-
This immune signaling reduces fat burning even when the body might otherwise rely on fat stores
-
The response appears to be tightly regulated and evolutionarily conserved
In essence, these immune cells act as metabolic gatekeepers, determining when fat should be preserved rather than burned.
Immune–Fat Crosstalk: A Protective but Costly Mechanism
The interaction between immune cells and fat tissue reflects a sophisticated biological balancing act. During infection or physiological stress, inflammation signals the body to prioritize survival over energy expenditure. Slowing fat loss may prevent excessive weight loss and muscle wasting during illness.
However, in modern societies—where infections are less deadly and food is readily available—this same mechanism may become maladaptive. Chronic low-grade inflammation, common in obesity, may continuously activate immune pathways that block fat burning, making weight loss more difficult.
Implications for Obesity and Metabolic Disease
These findings help explain why obesity is increasingly viewed as a complex biological condition, not simply the result of excess calorie intake or insufficient exercise.
Potential implications include:
-
Resistance to fat loss despite calorie restriction
-
A link between chronic inflammation and difficulty losing weight
-
New insights into why some individuals struggle to burn fat even with lifestyle interventions
This immune-mediated suppression of fat metabolism may contribute to insulin resistance, type 2 diabetes, and cardiovascular disease.
Rethinking Weight Loss Through an Immune Lens
Understanding the immune system’s role in fat metabolism opens new therapeutic possibilities. Instead of focusing exclusively on appetite suppression or calorie expenditure, future treatments may aim to modulate immune signaling within fat tissue.
Such approaches could:
-
Restore normal fat-burning pathways
-
Reduce inflammation without compromising immune defense
-
Improve the effectiveness of existing lifestyle and pharmacologic interventions
Importantly, this research does not suggest suppressing the immune system broadly, but rather targeting specific immune–metabolic pathways.
A New Frontier in Metabolic Research
The Nature study underscores a growing realization in biomedical science: metabolism, immunity, and inflammation are deeply interconnected. Fat tissue is not merely passive storage—it is an active immunological organ, constantly communicating with the rest of the body.
By revealing that immune cells may actively prevent fat burning, the research challenges long-held assumptions and offers a more nuanced understanding of energy balance and body weight regulation.
Conclusion
The discovery that white blood cells can limit fat burning highlights an unexpected but evolutionarily logical role of the immune system. What once helped our ancestors survive famine may now hinder metabolic health in an era of abundance. As researchers continue to unravel this immune–fat dialogue, new strategies may emerge to treat obesity and metabolic disease more effectively.
Understanding obesity, it turns out, may require looking not only at calories and exercise—but also at the immune system quietly working behind the scenes.
News in the same category

Radiation and Targeted Cancer Therapy Combination Shows Low Risk of Serious Side Effects

Can Metformin Protect Premature Infants After Antenatal Steroid Exposure?

Vaccines and Healthy Aging: Benefits That Go Beyond Infection Prevention

Drink Coconut Water for 7 Consecutive Days and Notice Remarkable Health Benefits

11 Fruits Rich in Iron That Help Improve Blood Health Naturally
Beyond Stroke, This Dangerous Disease Surges During Cold Weather
Why Do Older People Often Have More Age Spots on Their Skin?
What Role Do Methanogens Play in the Gut Microbiome?

The Best Times to Drink Coffee for Optimal Health Benefits

The Best Time to Drink Pomegranate Juice for Blood Pressure and Muscle Recovery
Why Your Cat Chooses to Sleep With You

10 Conditions Ginger Can Help Manage Naturally

How Often Do You Poop? New Research Shows Bowel Movement Frequency Linked to Overall Health

What Happens to Your Blood Pressure When You Drink Beetroot Juice Every Day

Signs and Symptoms of Oral Cancer

Obesity Is a Disease: Understanding Its Biology and Cardiovascular Impact

Exercise Linked to Better Outcomes in Patients With Hypertension

Adding Yoga to Opioid Use Disorder Care May Speed Recovery From Opioid Withdrawal
News Post
Are You Up to Date on Migraine Prevention?

Radiation and Targeted Cancer Therapy Combination Shows Low Risk of Serious Side Effects

Can Metformin Protect Premature Infants After Antenatal Steroid Exposure?

Choosing Compassion Over Cameras: A Young Man Saves a Shark by Removing a Fishhook

Abandoned at One Year Old: The Heartbreaking Reality Behind a Chihuahua Left at a Shelter

Pets Are Not Disposable: A Lifelong Commitment, Not a Temporary Choice

The 400-Year-Old Greenland Shark: One of the Oldest Living Vertebrates on Earth

Vaccines and Healthy Aging: Benefits That Go Beyond Infection Prevention
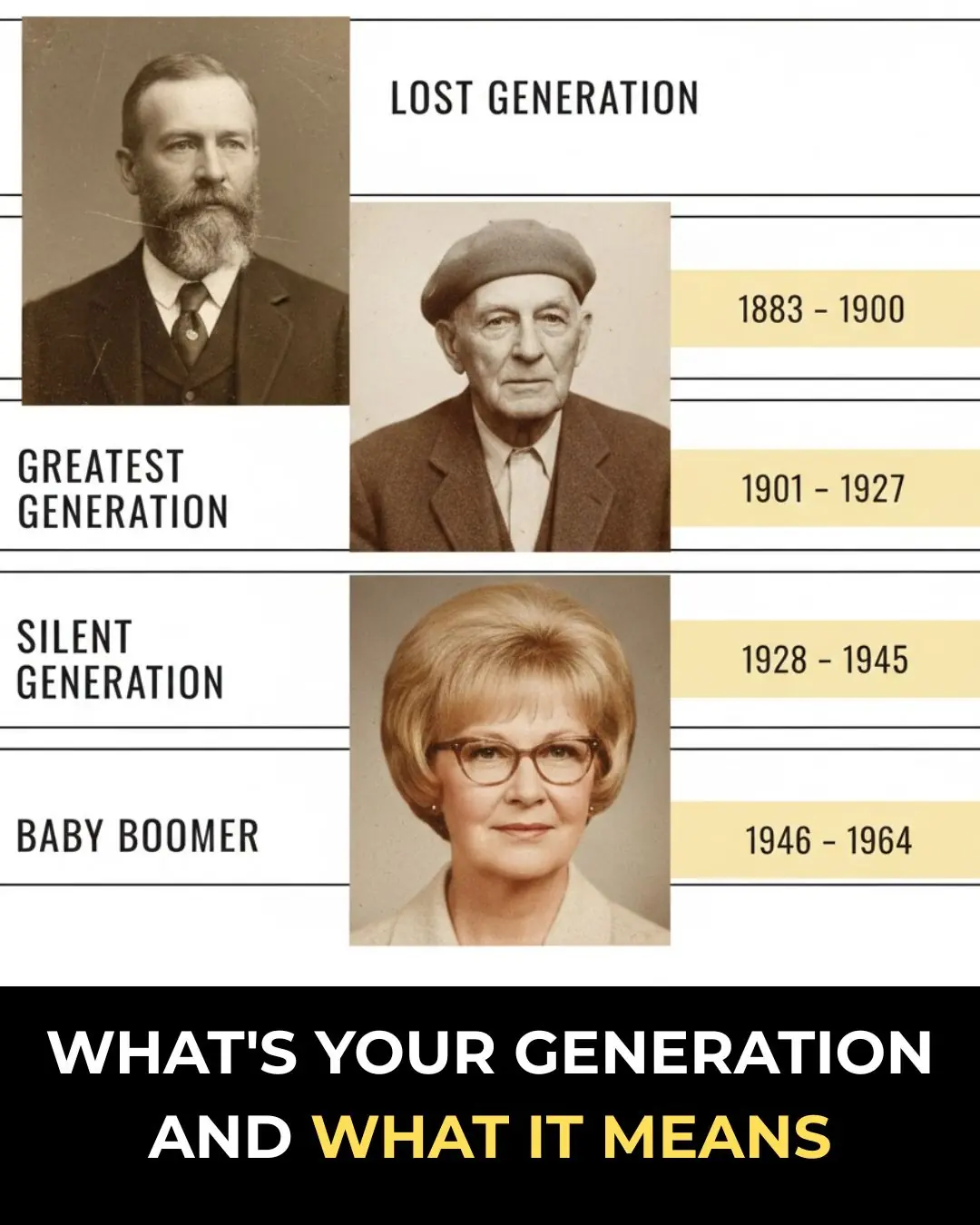
What’s Your Generation and What It Means

Drink Coconut Water for 7 Consecutive Days and Notice Remarkable Health Benefits

11 Fruits Rich in Iron That Help Improve Blood Health Naturally
Beyond Stroke, This Dangerous Disease Surges During Cold Weather
Why Do Older People Often Have More Age Spots on Their Skin?
What Role Do Methanogens Play in the Gut Microbiome?

The Best Times to Drink Coffee for Optimal Health Benefits

Bula Choudhury: A Masterclass in Resilience and the Quiet Pursuit of Greatness 🌊✨

Targeted Violence in Khulna: A Growing Crisis for Law and Order ⚠️🇧🇩

When One Moment Changes Everything: A Story of Love, Trust, and Betrayal 🎶⚡💔
