The Brainstem and Pain: New Research, New Understanding
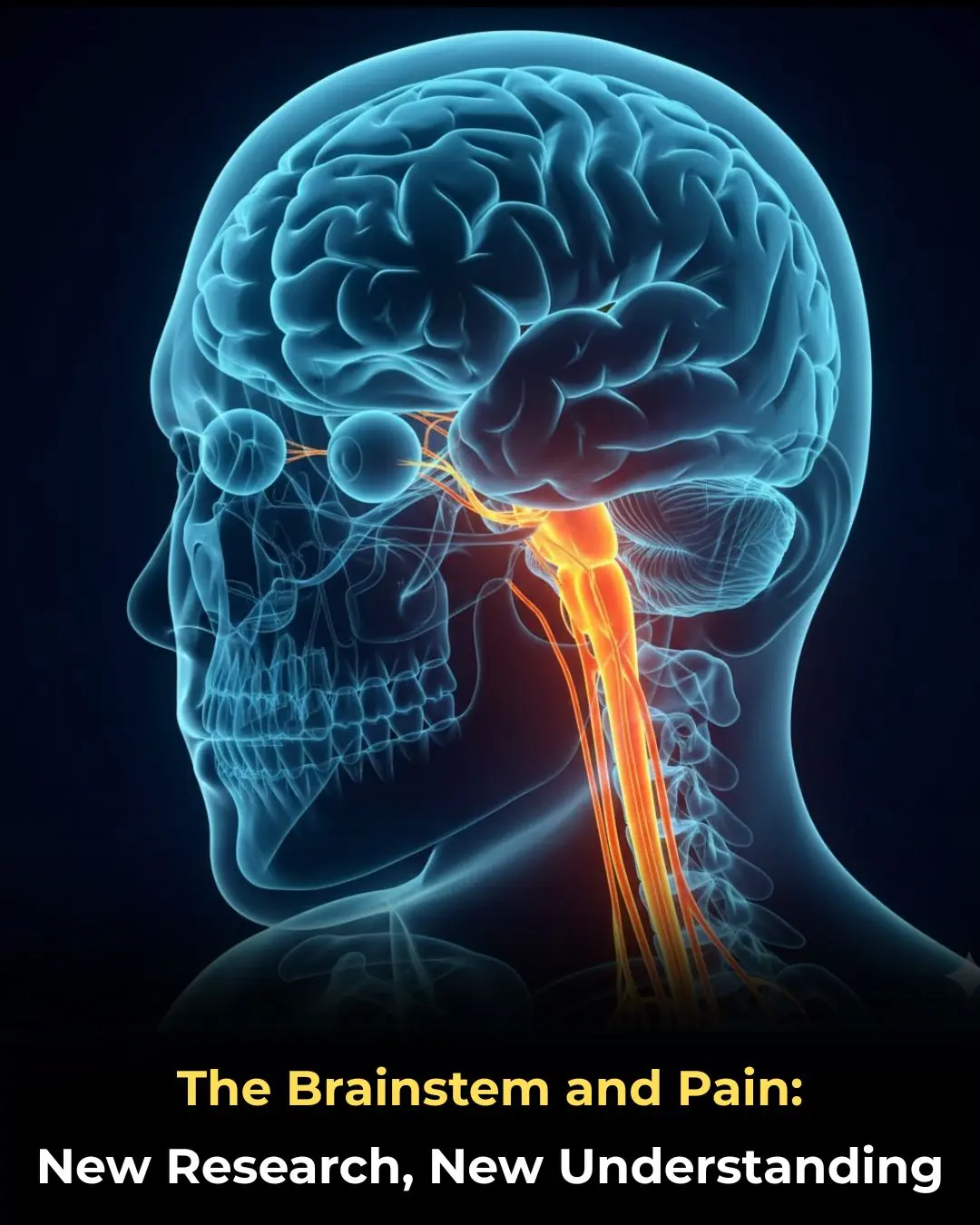
For decades, pain research has focused largely on the cortex and spinal cord, viewing the brainstem mainly as a relay station that simply transmits signals between the body and higher brain centers. However, a growing body of research is now reshaping that view. New evidence highlights the brainstem as an active and highly sophisticated regulator of pain—one that plays a decisive role in how pain is amplified, suppressed, and ultimately perceived.
These discoveries are changing fundamental assumptions about pain biology and opening the door to more precise, mechanism-based treatments for both acute and chronic pain conditions.
Moving Beyond the Traditional Pain Model
Traditionally, pain has been understood as a bottom-up process: noxious stimuli activate peripheral nerves, signals travel through the spinal cord, and the brain interprets those signals as pain. In this model, the brainstem was seen as a passive conduit rather than an active participant.
Recent research challenges this framework. Advanced neuroimaging, animal studies, and human experimental pain models now show that the brainstem contains specialized circuits that can either dampen pain signals or dramatically enhance them—sometimes before those signals even reach conscious awareness.
This shift in understanding helps explain why pain is not simply proportional to tissue damage and why individuals with similar injuries can experience vastly different pain levels.
The Brainstem as a Pain Modulator
The brainstem sits at a strategic crossroads between the spinal cord and higher brain regions. Within it lie multiple nuclei that are now recognized as central players in pain modulation.
Key functions of the brainstem in pain processing include:
-
Filtering incoming pain signals before they reach the cortex
-
Amplifying pain sensitivity under threat or stress
-
Suppressing pain during survival-critical situations
-
Integrating emotional and autonomic responses with sensory pain signals
This means the brainstem does not merely pass pain signals along—it actively decides how strong, persistent, or emotionally distressing those signals will be.
Descending Pain Control Pathways
One of the most important discoveries involves descending pain control systems that originate in the brainstem and project down to the spinal cord. These pathways can either inhibit or facilitate pain transmission at the spinal level.
Research shows that:
-
Some brainstem circuits release neurotransmitters that block pain signals, reducing sensitivity.
-
Other circuits enhance pain transmission, making sensations feel stronger or more unpleasant.
-
Dysfunction in these systems may contribute to chronic pain syndromes, where pain persists despite minimal or no ongoing tissue injury.
This dual capability helps explain why pain can fluctuate based on stress, mood, sleep quality, and overall health.
Implications for Chronic Pain Conditions
Chronic pain disorders such as fibromyalgia, migraine, neuropathic pain, and complex regional pain syndrome may involve abnormal brainstem activity rather than solely peripheral damage.
Studies suggest that in many chronic pain patients:
-
Pain-facilitating brainstem circuits may be overactive
-
Pain-inhibiting pathways may be weakened
-
Normal sensory input may be interpreted as painful
This perspective reframes chronic pain as a disorder of neural regulation rather than a purely structural problem—an insight that could reduce stigma and improve treatment strategies.
Why This Matters for Treatment Development
Understanding the brainstem’s role in pain opens new therapeutic possibilities beyond conventional analgesics.
Potential future approaches include:
-
Targeted neuromodulation to rebalance pain-inhibitory and pain-facilitatory circuits
-
More precise pharmacologic therapies aimed at specific neurotransmitter systems within the brainstem
-
Personalized pain treatment, based on individual neural pain profiles rather than symptom severity alone
Importantly, these advances may reduce reliance on broad-acting pain medications, including opioids, which often come with significant risks and limited long-term effectiveness.
Toward Mechanism-Based Pain Medicine
Experts increasingly emphasize the need to move from symptom-based pain management to mechanism-based care. The brainstem’s newly recognized role supports this shift.
Instead of asking only “How much pain does the patient report?”, clinicians may soon ask:
-
Which pain modulation systems are malfunctioning?
-
Is pain being amplified centrally rather than driven peripherally?
-
Can treatment be tailored to normalize neural processing rather than suppress symptoms?
Such an approach could transform pain medicine from trial-and-error prescribing to targeted intervention.
The Road Ahead
While these findings are promising, researchers caution that much remains to be learned. Brainstem circuits are complex, highly interconnected, and influenced by genetics, environment, and life experience. Translating laboratory discoveries into safe and effective clinical treatments will require time and careful study.
Nevertheless, the emerging science marks a turning point. By placing the brainstem at the center of pain research, scientists are uncovering mechanisms that help explain the subjective, variable, and deeply personal nature of pain.
Conclusion
New research is redefining the brainstem as a powerful regulator of pain rather than a passive relay. Its ability to shape pain sensitivity, emotional impact, and persistence offers critical insights into why pain behaves so differently across individuals and conditions.
As this knowledge continues to evolve, it holds the promise of more precise, personalized, and effective pain treatments—bringing medicine closer to addressing pain at its neural roots rather than merely silencing its symptoms.
News in the same category

What Can Happen When Women Lack Sexual Intimacy?

Tapering Antidepressants: What Strategy Works Best?
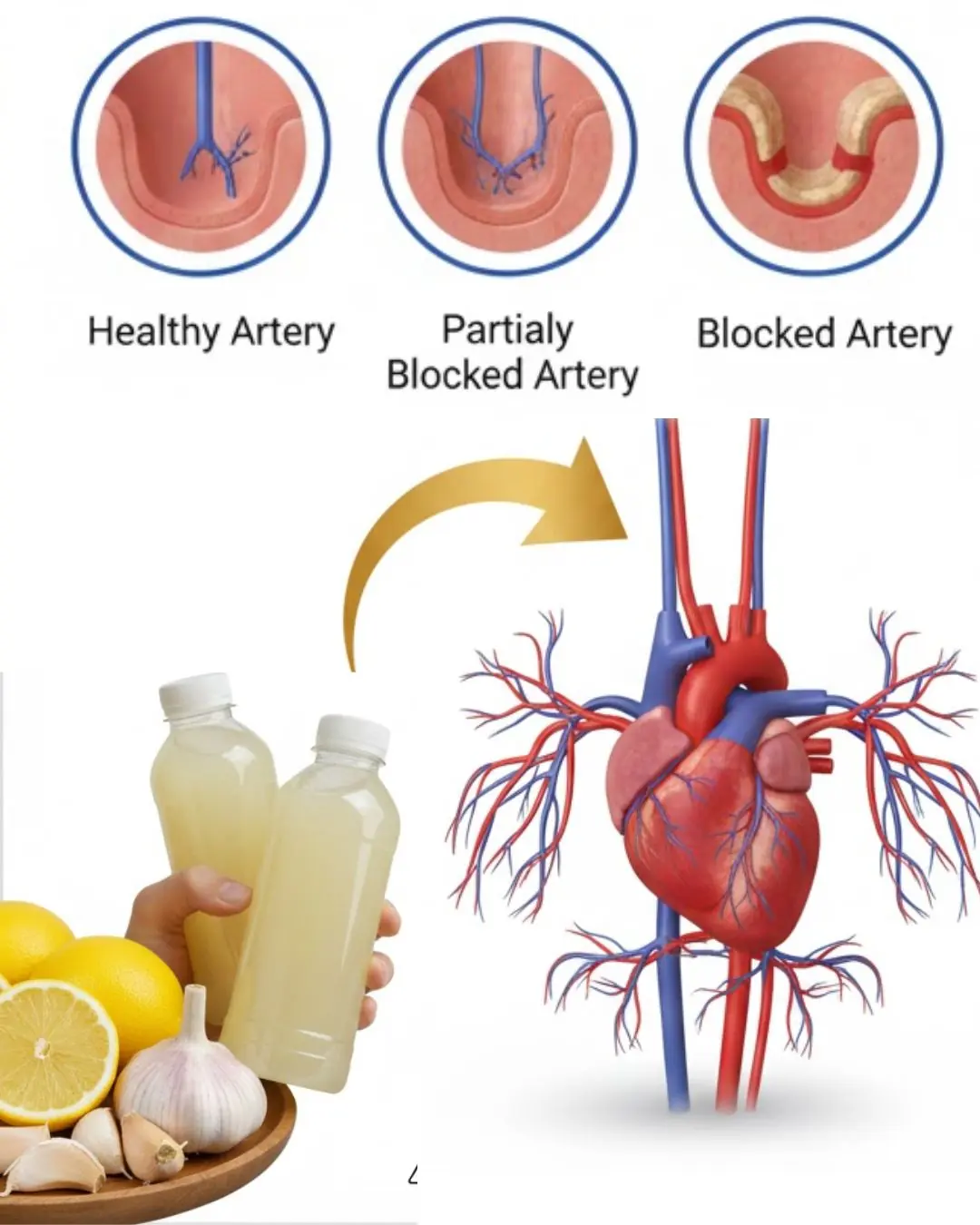
Could a Simple Bedtime Drink with Three Common Ingredients Support Your Heart Health?
Between Supplement Hype and Evidence: A Clinical Guide for Informed Use
Current Cardiac Screening Tools Miss Nearly Half of First Heart Attacks, Study Finds

Could Bone Broth Support Healthy Knee Cartilage as You Age?

Top 7 Best Drinks Diabetics Can Enjoy at Night to Support Healthy Blood Sugar Levels!

Papaya Leaves for Hair: A Natural Way to Support Healthier, Shinier Strands
Protect Your Eyes Naturally: 3 Powerful Seeds and 1 Fruit Every Senior Should Know About

Power Naps: The Benefits, How Long They Should Be, and When They Work Best
5 Early Signs and Symptoms of Ulcerative Colitis

8 Potential Health Benefits of Kombucha

Diagnosed with End-Stage Stomach Cancer, I Painfully Realized: 3 Foods Left Too Long in the Refrigerator Can Become “Accomplices” to Cancer

5 Detox Baths to Remove Aches, Pains and Toxins + Fragrant Bath Melts Recipe
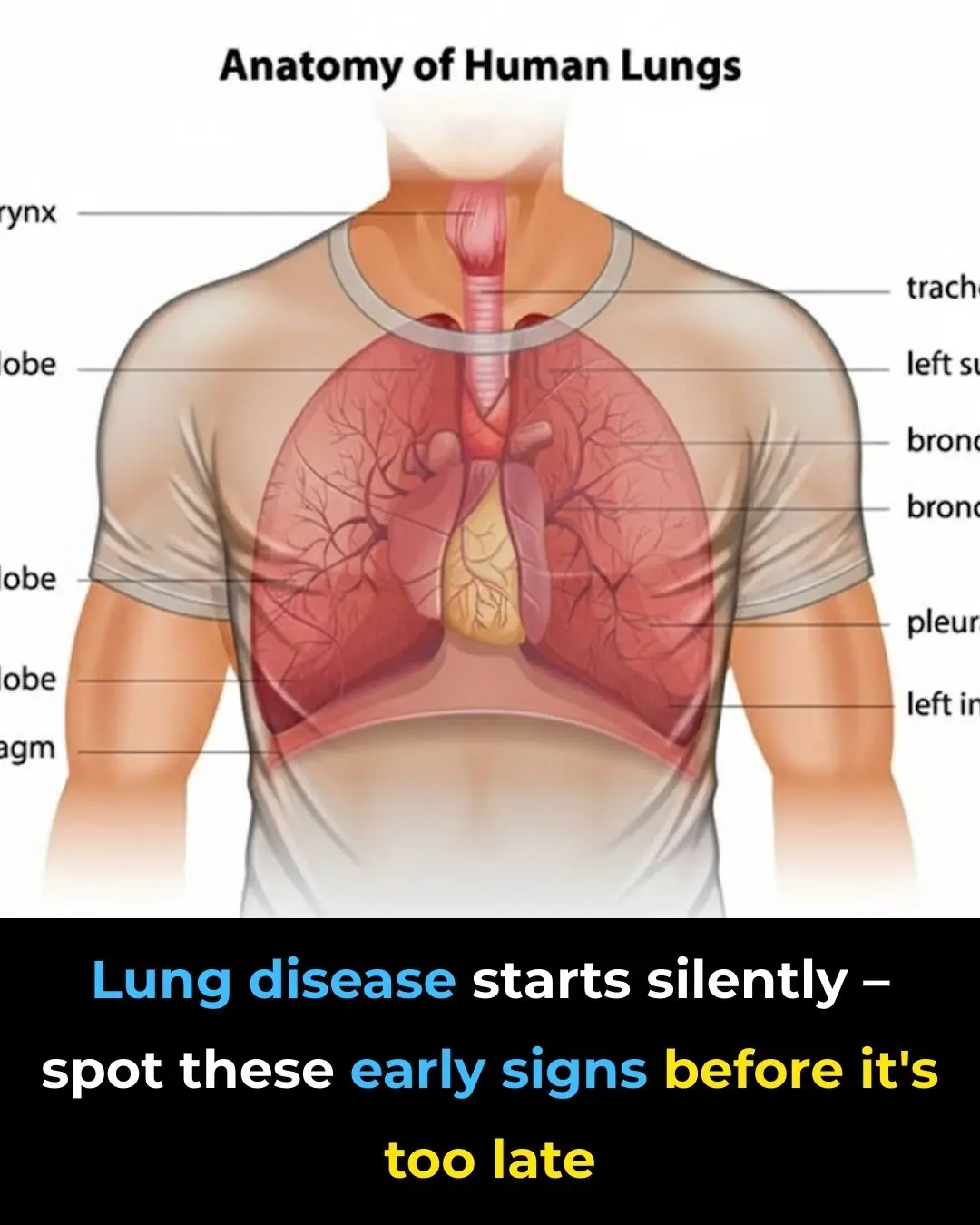
Early Signs of Lung Disease & How to Strengthen Your Lungs

5 things you absolutely SHOULDN'T do in the morning if you don't want your cancer cells to "grow like wildfire"

Emerging Flu Variant ‘Subclade K’ Raises Global Health Concerns Across the US, UK, and Beyond
A New Alternative to Reading Glasses: Eye Drops for Age-Related Near-Vision Loss
News Post

Bananas, Garlic, and Dates: The Powerful Health Combo
A Complete Guide to Breast Cancer Prevention

What Can Happen When Women Lack Sexual Intimacy?
After 30 years of my life, I learned that microwave ovens have this function

Tapering Antidepressants: What Strategy Works Best?
Black Mold on Refrigerator Door Seals? Use This Simple Trick to Clean It in Just 5 Minutes

Five Extremely Dangerous Types of Meat You Should Avoid
10 Probiotic Foods to Improve Your Gut Health Naturally
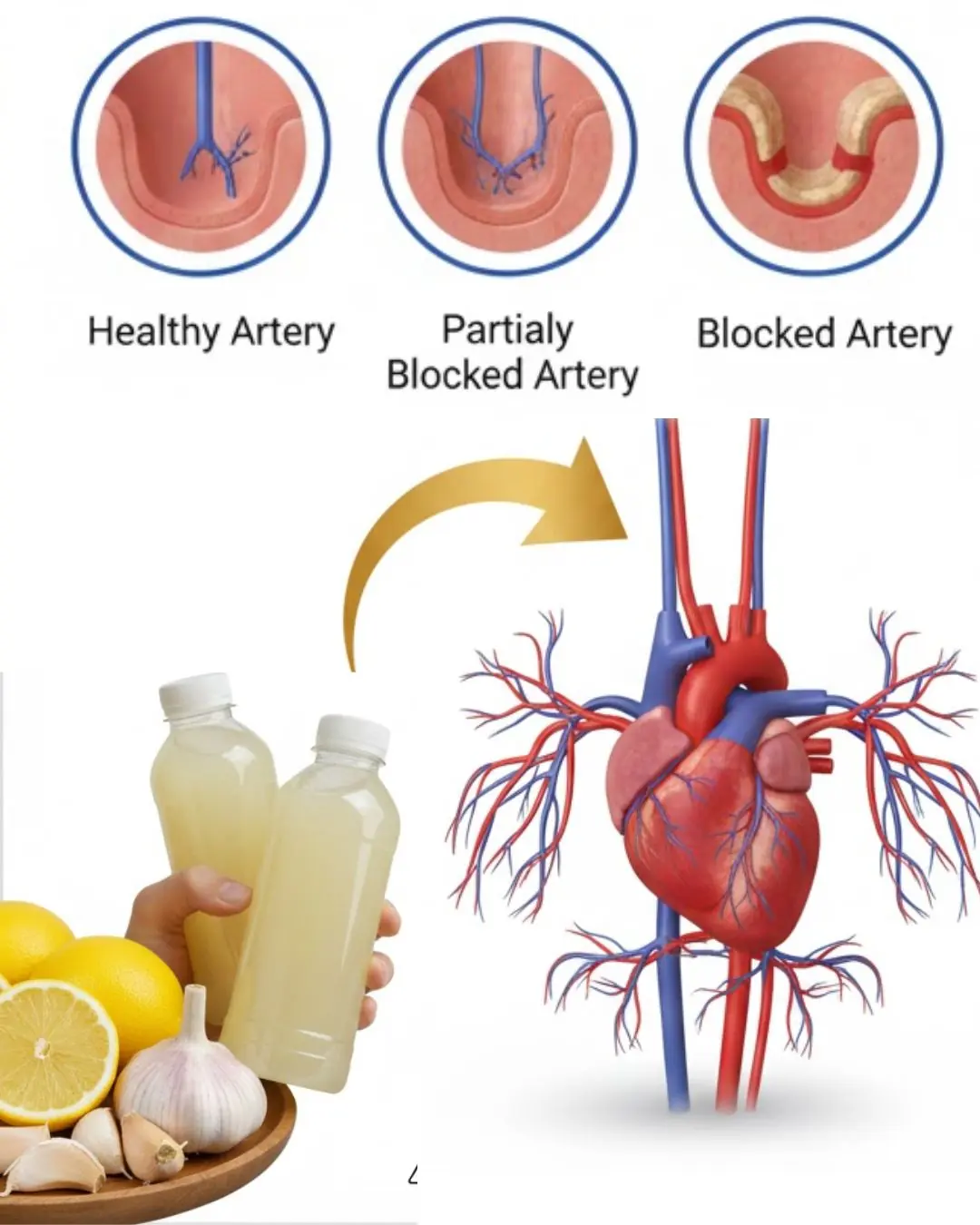
Could a Simple Bedtime Drink with Three Common Ingredients Support Your Heart Health?
What kind of fruit is so familiar that most people eat it when it's ripe but don't know that the green fruit is considered the "architect" of the intestines?

A TV Viewer’s Sharp Eye Helped Save Flip or Flop Star Tarek El Moussa’s Life
Graduate Kneels to Thank Brother Who Gave Up School for Her

32 Years of Service: Community Saves Elderly Carabao in the Philippines From Slaughter

A Father at Work, a Baby’s Smile, and a Moment That Touched Millions
Jordyn Woods is engaged to Karl-Anthony Towns — see the massive engagement ring set to spark trends in 2026
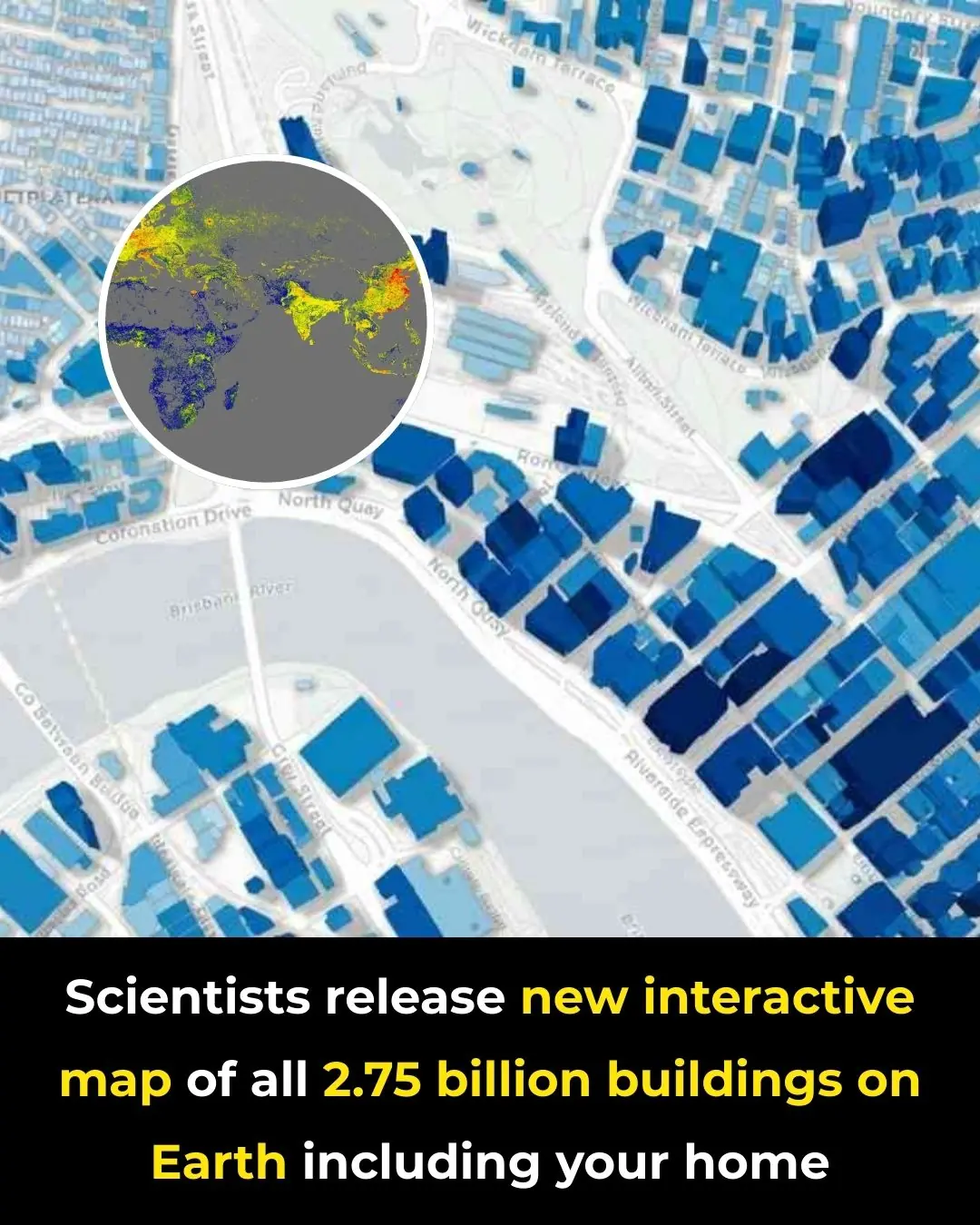
A New Global Atlas Maps Every Building on the Planet in Unprecedented Detail

A Bed on Wheels: A Chinese Inventor’s Unusual Take on Personal Transportation
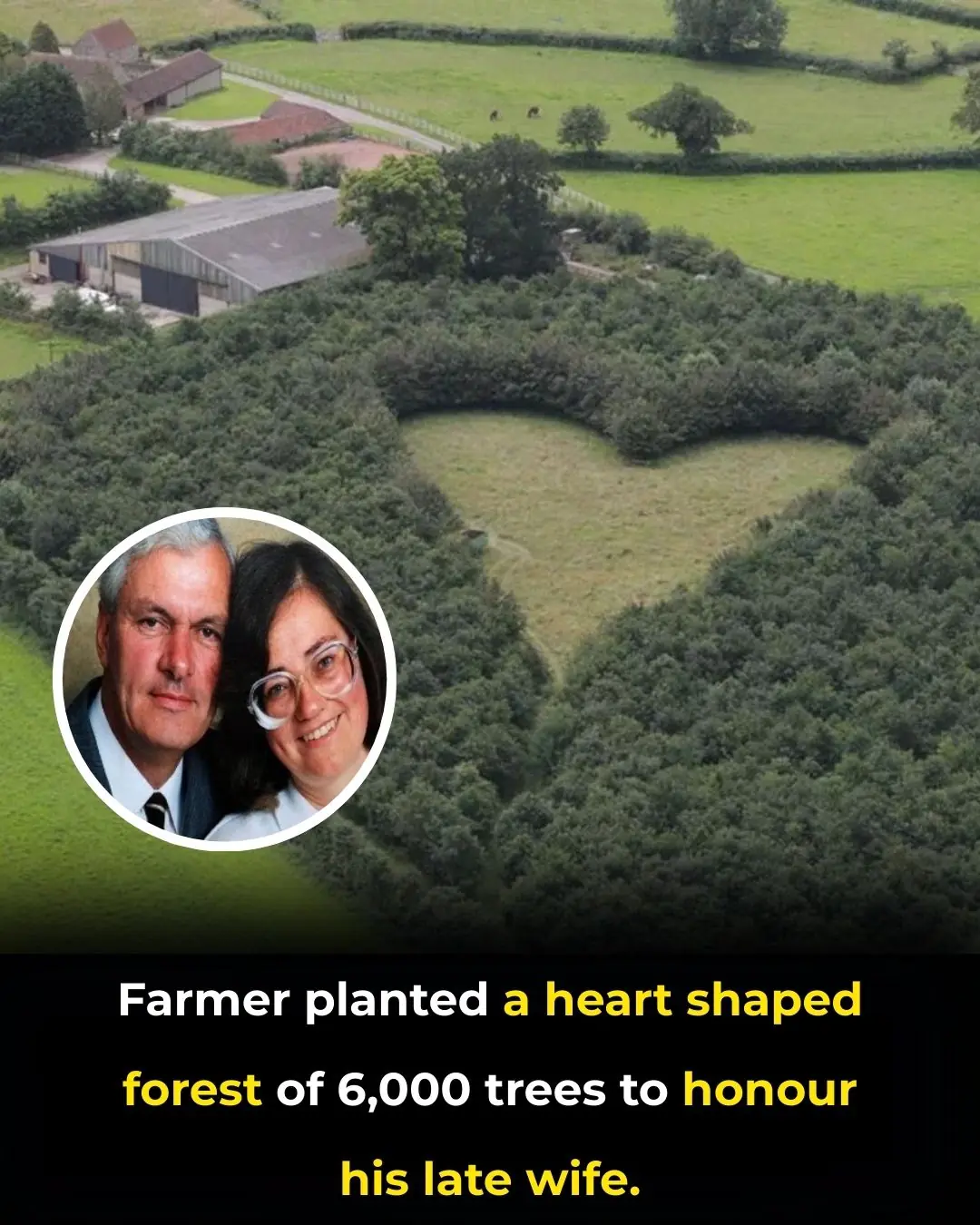
Planting Love That Endures: The Heart-Shaped Forest of Winston Howes