The new vitamin D findings forcing experts to rethink heart health
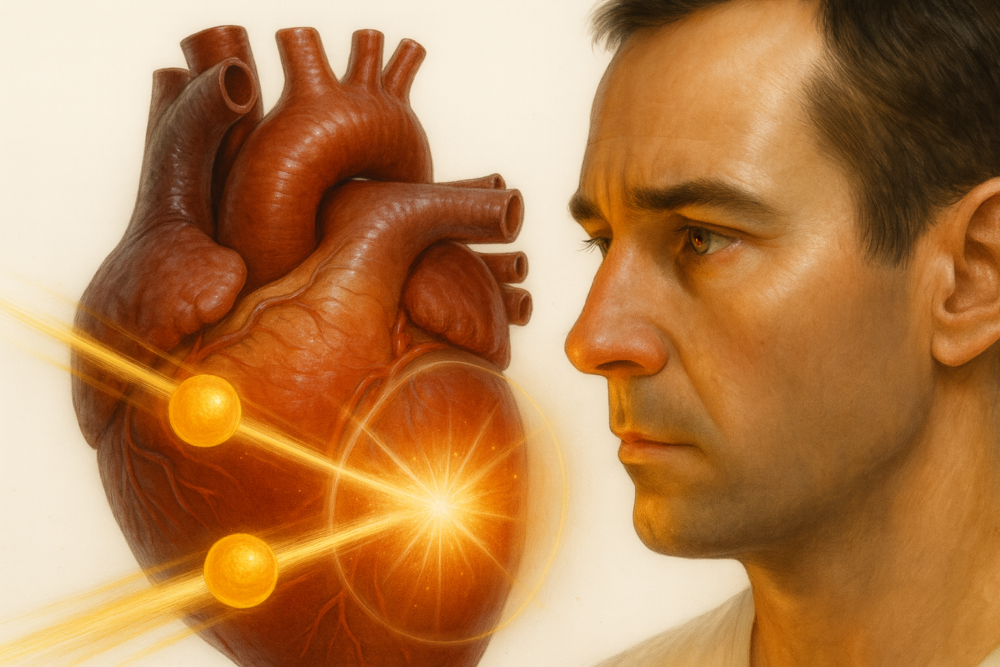
Could Vitamin D Be the Overlooked Key in Preventing Heart Attacks and Strokes? The Truth May Surprise You
Could something as simple and inexpensive as vitamin D be the hidden tool we’ve been overlooking in the battle against heart attacks and strokes? It sounds almost too good to be true—but recent research suggests the story is more complicated, and more intriguing, than we once believed.
For years, vitamin D has been at the center of countless health discussions. It shows up in conversations about bone strength, immune support, mood regulation, and even potential links to lower rates of cancer. Yet when it comes to heart disease—the world’s leading cause of death—the evidence has been anything but clear. Confusion, debate, and conflicting studies have left both physicians and patients wondering: Does vitamin D really matter for heart health?
A new study, however, is shaking up old assumptions. If you've ever questioned whether you’re getting enough vitamin D, or whether blood tests and supplements are worth the fuss, this is a conversation you’ll want to pay attention to. (Inspired by insights from Dr. Brad Stanfield.)
Key Takeaways
-
Early research suggested widespread vitamin D deficiency was linked to many serious diseases.
-
Large, high-quality clinical trials later found no strong evidence that routine vitamin D supplements prevent heart disease or cancer.
-
A new study—the TARGET D trial—focused specifically on high-risk heart patients and uncovered surprising patterns.
-
While results were mixed, patients who optimized their vitamin D levels experienced a significant drop in repeat heart attacks.
-
Whether routine vitamin D testing or aggressive supplementation should be standard is still unclear, but this new data is challenging long-held beliefs.
1. The Early Hype: Was Vitamin D Deficiency a Global Health Crisis?
About a decade ago, it seemed like nearly everyone was suddenly “low” in vitamin D. Observational studies painted a dramatic picture: people with low vitamin D levels were more likely to suffer from infections, diabetes, autoimmune conditions, certain cancers, and especially cardiovascular disease. The media ran with the story, doctors ordered millions of blood tests, and supplement sales skyrocketed.
The idea was simple and appealing: low vitamin D equals higher disease risk, so raising vitamin D should fix the problem. But science is rarely that straightforward.
2. A Reality Check: Large Trials Fail to Deliver the Promised Benefits
When researchers conducted massive, well-designed clinical trials—like the VITAL trial, which included more than 25,000 adults—the results were far less impressive. People who took vitamin D supplements did not show clear reductions in heart attacks, strokes, or cancer rates compared to those who didn’t supplement at all.
These findings led major medical groups, including the Endocrine Society, to dial back earlier enthusiasm. Instead of high doses and routine testing, they recommended that most people simply meet the standard daily intake of around 800 IU. Unless you had specific risk factors—like certain medical conditions or severely limited sun exposure—doctors were advised not to order vitamin D tests for everyone.
3. A New Twist: The TARGET D Trial Challenges the Old Narrative
Here’s where things get interesting. The TARGET D trial looked at a group very different from the general population—people at extremely high risk of heart complications, such as individuals who had just suffered a heart attack.
In this study, patients had their vitamin D levels measured, and many were found to have less-than-optimal levels. Half of the participants then received personalized vitamin D supplementation designed to bring their blood levels above 40 ng/mL, with adjustments made throughout the four-year study. The other group simply received standard care without vitamin D targeting.
This “precision medicine” approach is something previous large trials didn’t explore.
4. Mixed Overall Results… But a Striking Drop in Repeat Heart Attacks
When researchers evaluated the main endpoints—death, second heart attacks, heart failure hospitalizations, or strokes—they didn’t find a statistically significant difference between the two groups.
But buried in the data was a surprising and potentially important finding:
Patients who achieved optimal vitamin D levels had about a 52% lower risk of experiencing another heart attack.
To put it another way: for every 100 patients like “John” in the study, about four fewer repeat heart attacks occurred over four years in the vitamin-D-optimized group. While not a massive number, it’s meaningful—especially for people who are already high-risk.
This pattern suggests that vitamin D may not prevent heart disease in everyone, but it might play a role in preventing recurrent heart problems in vulnerable individuals.
5. Why This Study Stands Out: Tailored Supplementation, Not One-Size-Fits-All
Unlike earlier trials that simply gave everyone the same generic dose, the TARGET D trial aimed to reach a specific blood level in each participant. This approach recognizes a crucial nuance: the benefits of vitamin D supplementation may only appear when you correct true deficiency, not when you supplement people who are already sufficient.
This personalized method mirrors modern medical trends—moving from broad recommendations to targeted, data-driven decisions.
6. But Don’t Jump to Conclusions: Important Limitations Remain
Before you rush to the pharmacy or schedule a vitamin D test, it’s essential to understand the study’s limitations.
-
It wasn’t blinded. Both patients and doctors knew who was receiving vitamin D optimization, which can unconsciously influence behavior and outcomes.
-
The main outcome wasn’t statistically significant. The most important measures didn’t show clear benefits.
-
Some positive findings may be due to chance. Subgroup analyses can uncover patterns that don’t always hold up in future research.
In short: the results are intriguing—but far from definitive.
7. Potential Risks: Vitamin D Isn’t Always Harmless
Although vitamin D is often seen as safe, more isn’t always better. Vitamin D acts like a hormone in the body, and excessively high levels can trigger unwanted effects.
In the TARGET D trial, there were hints (though not statistically meaningful) of higher rates of heart failure and strokes in the vitamin D group. This serves as a reminder that even “natural” supplements can have downsides when used aggressively.
8. Current Recommendations: No Reason to Abandon Official Guidelines Yet
Despite the buzz around new findings, medical organizations have not updated their recommendations. For most adults:
-
A standard daily dose of around 800 IU is adequate.
-
Routine vitamin D testing is unnecessary unless you have clear risk factors.
-
Supplements should be used thoughtfully—not as a cure-all.
Given the mixed evidence, experts agree that widespread testing or high-dose supplementation isn’t justified at this time.
9. What Should You Do? A Personalized, Balanced Approach
If you’ve recently had a heart attack or know you’re at high cardiovascular risk, the TARGET D results may be worth discussing with your doctor. For certain individuals, a vitamin D test—paired with a personalized treatment plan—might make sense.
For everyone else, the smartest strategy remains simple:
-
Get reasonable sun exposure.
-
Eat a balanced, nutrient-rich diet.
-
Use modest supplements if you belong to an at-risk group.
Until stronger evidence emerges, vitamin D should be considered one part of a much bigger picture—not a magic bullet.
10. What I’m Doing—And What You Might Consider
Inspired by this new research, my approach has become more nuanced. With high-risk patients, I’m more open to discussing personalized vitamin D testing and supplementation. For my own health, I’m considering checking my vitamin D level for the first time—but I’m still avoiding extreme doses and sticking to evidence-based practice.
Vitamin D remains one of the most fascinating and debated nutrients in modern medicine. The story is evolving, and future studies will help clarify how much it truly matters for heart health. If you or someone you care about is at high risk for cardiovascular disease, having an informed, individualized conversation with a healthcare provider is the best step forward.
In the meantime, remember: long-term heart health still depends most on lifestyle—nutritious eating, regular activity, quality sleep, and following proven medical advice. Supplements may help, but healthy habits remain the real foundation.
News in the same category
Diabetes? Just Boil These Leaves to Lower Blood Sugar (Without Medications!)

These 9 Nutrients Will Shockingly Heal Nerve Damage!
6 Physical Changes That Happen When Your Heart is In Serious Danger
5 Common Habits That Quietly Damage Your Kidneys

Rosemary Tea: Drink It for 15 Days and See What Happens

What happens to the body after gallbladder removal? 3 diseases that may follow — avoid surgery if possible
If Your Kidneys Are In Danger, The Body Will Show These 10 Signs

Prostate health expert reveals the 5 daily habits men over 50 shouldn’t ignore
7 Powerful Anti-Cancer Foods You Should Start Including in Your Diet
THIS IS WHAT HAPPENS TO YOUR LUNGS, MOOD, AND BLOOD CIRCULATION WHEN YOU USE A HIMALAYAN SALT LAMP
🍯 Clear Mucus Naturally: The 2-Ingredient Soothing Remedy 🍋
15 visible signs of low thyroid you can see – don’t ignore #7!

8 powerful anti-cancer foods you should start including in your diet

Prostate health expert reveals the 5 daily habits men over 50 shouldn’t ignore
The 4 hidden causes of persistent phlegm in your throat (& how to fix it naturally)

Canada Loses Measles-Free Status After Nearly 30 Years as the U.S. Faces Growing Risk
How a Blood Protein May Be the Key to Slowing Aging

Drinking a Cola Could Shorten Your Lifespan by This Exact Amount, According to Scientists
News Post

Yellow Stains on Toilet Seats and Bowls: Sprinkle This to Remove Stains and Eliminate Odors

Whoa, had no clue about this!

A True Story of Unexpected Ocean Heroism

My nana taught me this hack to deodorize trash cans in 2 mins with 0 work. Here’s how it works

9 Foods You Should Eat Regularly to Prevent Memory Loss and Keep Your Brain Sharp as You Age

I Just Learned This: Adding a Handful of Salt to Your Washing Machine Works Wonders!

5 Types of Eggs You Should Avoid Eating Too Often — They May Harm Your Health

Why Do Elevators Have Mirrors? The Surprising Benefits Behind a Simple Design
Why Okra Is Considered “Green Gold” for Your Health

5 Drinks That May Help Break Down Kidney Stones and Support Easier Elimination

It’s Time to Save Your Heart by STOPPING These 5 Foods at Night

Boiled Banana Tea With Cinnamon & Ginger: The Nighttime Remedy Everyone Is Talking About

Say Goodbye to Swelling
15 visible signs of low thyroid you can see – don’t ignore #7!

Growing Kindness and Sustainability: New Zealand’s School Programs Teach Kids to Plant, Harvest, and Share

Jermaine's Heroic Climb: A Story of Unwavering Love and Courage in West Philadelphia

Groundbreaking Stem Cell Therapy Could Provide Lifelong Immunity Against Cancer
Kanye West’s $3,900 Curry Delivery: The Wildest Food Craving in Celebrity History