
Thyroid Cancer Is Quietly Rising Among Young Women Often Showing Subtle Signs Before Detection
The Hidden Climb of Thyroid Cancer in Younger Women (Expanded Edition)
This post may contain affiliate links. As an Amazon Associate, I earn from qualifying purchases. Read my disclosure policy here.
Thyroid cancer has quietly become one of the most unsettling medical trends of the past several decades. Even as healthcare advances and diagnostic tools become more refined, the number of cases continues to climb—and the most notable shift is occurring in a demographic few expected. Increasingly, younger women are facing a disease historically associated with older adults. Many receive their diagnosis only after months or even years of unexplained fatigue, subtle voice changes or a small neck lump they attributed to stress, thyroid imbalance or the demands of daily life.
This rise has perplexed researchers, oncologists and public health experts worldwide. On one hand, the outlook for most thyroid cancer patients remains highly favorable: survival rates are among the highest of all cancers. On the other hand, the reasons behind the growing number of cases are far more complex than simple overdiagnosis or improved screening. A combination of environmental exposures, metabolic shifts, lifestyle patterns, hormonal influences and advances in imaging all appear to contribute to this trend (National Cancer Institute).
Behind the statistics lies a deeper reflection on modern health—and how our bodies adapt, sometimes painfully, to the pressures of contemporary life. Understanding why this is happening requires more than a scan of symptoms or numbers. It asks us to consider the intersections between environment, physiology and behavior while recognizing that early symptoms are often subtle enough to blend invisibly into the routines of work, family and stress.
The Rising Trend in Thyroid Cancer
Thyroid cancer is increasing more rapidly than many other major cancers. In the United States, incidence rates tripled between 1980 and 2016 (American Cancer Society). This trend is mirrored across numerous countries, including those without widespread ultrasound screening programs—indicating that the rise cannot be explained solely by increased detection.
The thyroid, located at the base of the neck, regulates metabolism, energy, temperature and heart rate. When its cells grow uncontrollably, tumors form. Papillary thyroid carcinoma, the most common type, generally grows slowly and is highly treatable. Less common forms—follicular, medullary and the rare anaplastic type—behave more aggressively and may spread earlier (Mayo Clinic).
For years, improved detection was considered the primary cause of rising diagnoses. Ultrasound technology and fine-needle aspiration biopsy, introduced widely in the 1980s and 1990s, made it possible to detect tiny tumors that previously went unnoticed. Many of these small papillary cancers grow so slowly that they would never have caused symptoms or affected lifespan.
However, more recent data show that this explanation is incomplete. Larger and more advanced tumors are also increasing, and mortality rates have not declined as much as experts once predicted. Even regions with limited imaging capabilities report similar trends. This points to underlying forces beyond better detection (Journal of Clinical Oncology).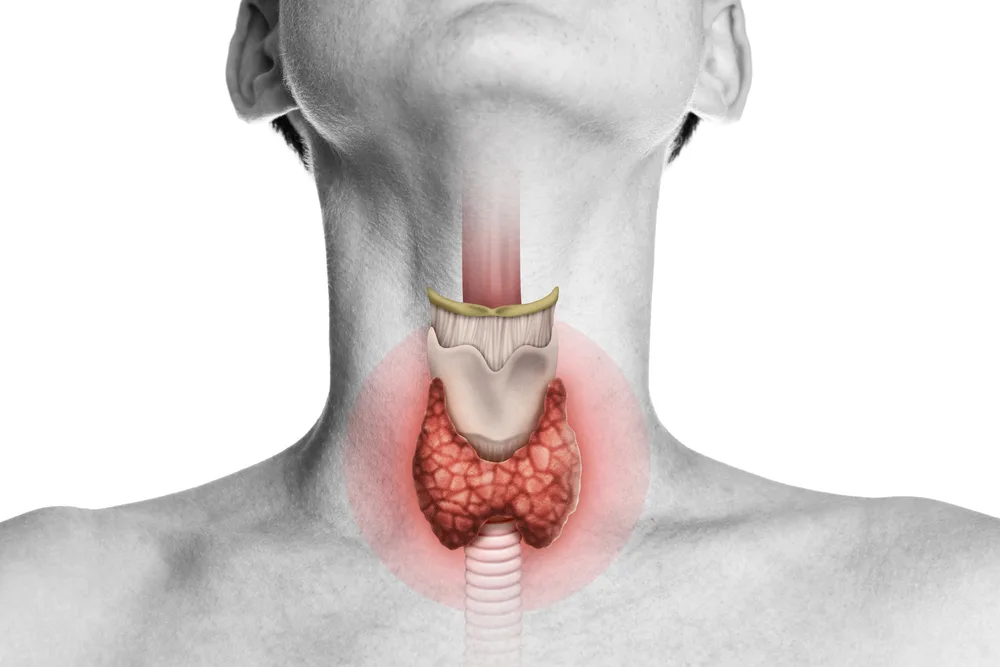
Why Young Women Are Most Affected
The gender gap in thyroid cancer is striking:
Women develop thyroid cancer three times more often than men, and the highest risk group includes women in their 30s, 40s and 50s (Endocrine Society).
Several factors may explain this pattern:
1. Hormonal Influences
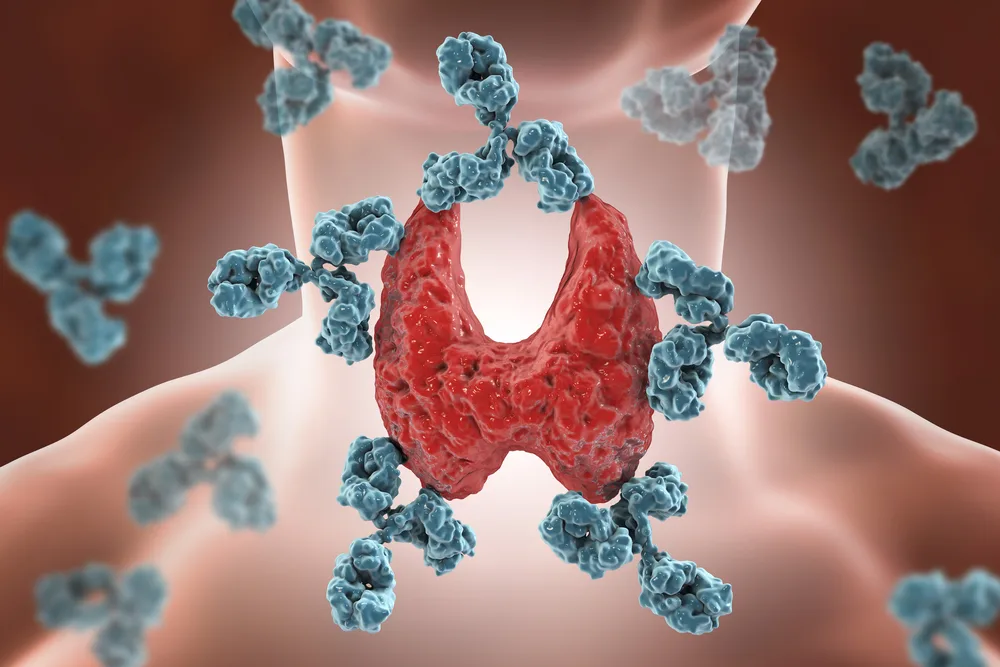
The thyroid is intimately connected to the endocrine system. Women experience ongoing hormonal shifts—monthly cycles, pregnancy, postpartum changes and perimenopause—all of which create additional stress on thyroid regulation. Estrogen may also influence thyroid cell growth and immune function (Journal of Endocrinology).
2. Higher Nodule Prevalence
Up to 80% of women develop thyroid nodules in their lifetime. Most are benign, but a larger population with nodules increases the number of cancers detected (American Thyroid Association).
3. Blurred Symptoms
Neck lumps, fatigue and mild throat pressure often get misattributed to stress, viral illness or hormonal imbalance—especially among busy younger women. By the time symptoms escalate, tumors may have grown or begun spreading.
Subtle Symptoms That Go Unnoticed

Early signs of thyroid cancer often blend into the background of everyday life. Common symptoms include:
-
A lump or swelling in the neck
-
Persistent hoarseness or voice changes
-
Difficulty swallowing or a sensation of throat pressure
-
Chronic fatigue not explained by lifestyle
-
Unexplained weight loss
-
Swollen lymph nodes near the collarbone
Fatigue—one of the earliest symptoms—is easy to dismiss in women managing careers, families and social pressure. Because thyroid cancer is usually slow growing, symptoms can remain subtle for long periods, delaying diagnosis.
Overdiagnosis vs. a True Increase in Cases
Initially, experts believed the surge in thyroid cancer stemmed primarily from overdiagnosis—the detection of small cancers unlikely to affect health or longevity. Indeed, ultrasound and biopsy identified countless tiny papillary tumors that historically would have gone unnoticed.
But the picture has shifted. Aggressive and metastatic cases are also rising, suggesting that a genuine increase is occurring. Mortality rates have slightly increased in several regions despite improved treatments (International Journal of Cancer).
Medical practice has responded. Instead of immediately treating all small tumors, many physicians now use:
-
Active surveillance rather than surgery
-
Partial thyroidectomy instead of full removal
-
Selective use of radioactive iodine
These changes reduce overtreatment but do not explain the continued rise in large or advanced tumors.
Obesity and Metabolic Stress
A significant body of research now links high body mass index (BMI) with increased thyroid cancer risk. Individuals with obesity are more likely not only to develop thyroid cancer but also to present with more aggressive disease (The Lancet Diabetes & Endocrinology).
Potential mechanisms include:
-
Elevated levels of thyroid-stimulating hormone (TSH)
-
Chronic inflammation
-
Insulin resistance
-
Altered cellular metabolism
These metabolic conditions create an environment that may encourage abnormal thyroid cell growth. Notably, obesity rates began rising globally around the same time thyroid cancer rates climbed—a parallel that continues to draw scientific attention.
Environmental Exposures and Chemical Disruptors
Thyroid function is extremely sensitive to environmental chemicals. Endocrine-disrupting chemicals (EDCs)—including those found in plastics, cookware, receipts, cosmetics, carpeting and pesticides—can mimic hormones or interfere with natural hormonal messaging.
Substances of concern include:
-
PFAS chemicals (PFOA, PFOS)
-
Flame retardants
-
Pesticides
-
Phthalates
-
Bisphenol-A (BPA)
Although the evidence remains mixed, long-term exposure—even at low levels—may impact thyroid function and potentially increase cancer susceptibility (Environmental Health Perspectives).
Another emerging theory links thyroid cancer prevalence to volcanic regions. Volcanic soils can contain trace elements such as vanadium or boron that may influence thyroid behavior. Research is ongoing and remains inconclusive.
Medical Radiation and Childhood Exposure
Exposure to medical radiation during childhood—especially repeated CT scans of the head, neck or chest—has been associated with a higher risk of developing thyroid cancer later in life (British Medical Journal). The thyroid gland is particularly sensitive to ionizing radiation during growth phases.
While modern imaging is safer than earlier technologies, cumulative exposure remains an important consideration, particularly for younger patients.
How Thyroid Cancer Is Diagnosed Today
Diagnosis typically involves:
-
Physical examination and medical history
-
Thyroid function blood tests
-
High-resolution ultrasound (the gold standard for nodule evaluation)
-
Fine-needle aspiration biopsy for suspicious nodules
-
Molecular testing for unclear biopsy results
-
CT, MRI or PET scans in rare or advanced cases
Advances in imaging and pathology interpretation have significantly improved accuracy. In some cases, second opinions or repeat imaging prevent missed or delayed diagnoses.
Treatment Approaches and Emerging Innovations
Thyroid cancer treatment is increasingly personalized.
Traditional Approaches
-
Surgery (partial or total thyroidectomy)
-
Radioactive iodine therapy
-
Hormone replacement therapy
-
External radiation or chemotherapy (for aggressive or recurrent disease)
-
Targeted therapies for tumors with specific genetic mutations
Newer Technologies
Radiofrequency ablation (RFA) has emerged as a minimally invasive option for shrinking benign nodules or treating certain recurrent cancers. It requires minimal recovery time and avoids neck scarring, making it an attractive alternative for selected patients (Radiology Society of North America).
Advances in Genetics
Molecular research has identified genetic signatures that influence prognosis and treatment choice. Targeted therapies based on tumor mutations are improving outcomes, especially for cancers resistant to standard treatments.
The Emotional Journey for Women
Although thyroid cancer is often slow growing, the emotional experience can be overwhelming. Women must navigate:
-
The shock of diagnosis
-
The frustration of years of subtle symptoms dismissed as stress
-
Recovery from surgery
-
Lifelong medication adjustments
-
Anxiety about recurrence
Many describe the journey as learning to understand a “new” body. Compassionate medical care, strong support systems and informed self-advocacy play crucial roles in emotional and physical healing.
Toward Better Awareness and Prevention
Prevention remains challenging because thyroid cancer stems from a combination of genetic, hormonal, environmental and metabolic factors. However, increased awareness can lead to earlier diagnosis and improved outcomes.
Key steps include:
-
Paying attention to neck changes
-
Monitoring fatigue or voice alterations
-
Understanding personal risk factors
-
Advocating for appropriate imaging when symptoms persist
-
Managing metabolic health through diet, exercise and stress reduction
-
Reducing unnecessary radiation exposure
Women who trust their instincts often detect problems earlier than tests alone would reveal.
Where Awareness Meets Action
The rise of thyroid cancer in younger women reflects the interplay of modern lifestyle pressures, environmental exposures, hormonal patterns and evolving medical practices. While improved imaging uncovered many small and harmless nodules, a deeper shift is at work—one that mirrors the complexities of contemporary health.
The encouraging news: most thyroid cancers are highly treatable, and survival rates remain exceptional. The greater challenge lies in recognizing the quiet early signs, understanding the unseen stressors shaping thyroid health and empowering women to advocate for care even when symptoms seem small.
This rise is not a narrative of fear but a reminder that the body communicates continuously—even in whispers—and those whispers deserve attention.
Sources
-
American Cancer Society
-
National Cancer Institute
-
Mayo Clinic
-
Journal of Clinical Oncology
-
Endocrine Society
-
American Thyroid Association
-
Journal of Endocrinology
-
International Journal of Cancer
-
The Lancet Diabetes & Endocrinology
-
Environmental Health Perspectives
-
British Medical Journal
-
Radiology Society of North America
If you’d like, I can also shorten this into a blog-ready version, create a PDF, or format it for social media or newsletter publication.
News in the same category


Watercress: The World’s Top Anti-Cancer Vegetable You Can Find in Vietnamese Markets
4 Plants That Snakes Absolutely Love — Remove Them Immediately to Keep Your Home Safe
The 4 “Golden Hours” to Drink Coffee for Maximum Health Benefits — Cleaner Liver, Better Digestion, Sharper Mind
Don’t Rip This Out — Treat It Like Gold Instead. Here’s Why.

Say Goodbye to Bare Branches: Revive Your Christmas Cactus Blooms with These Expert-Backed Hacks

Were You Aware of This? A Surprisingly Simple Spoon Trick Can Stop Mosquito Bite Itching
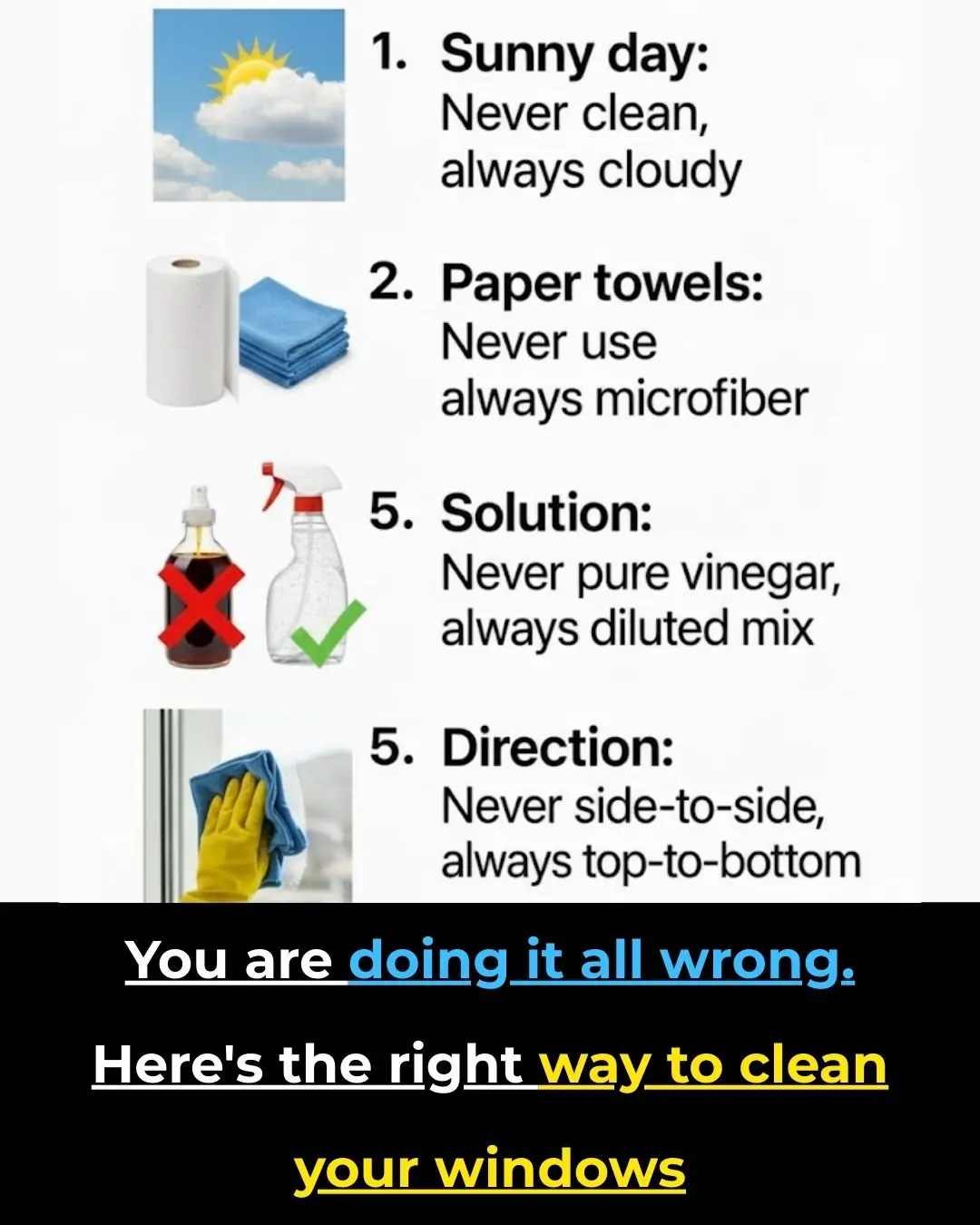
You’re Doing It All Wrong — Here’s the Right Way to Clean Your Windows

Get Ready for the Final Supermoon of 2025: The Cold Moon Shines Bright

Vaping Linked to Rare and Irreversible Lung Damage: What New Research Reveals
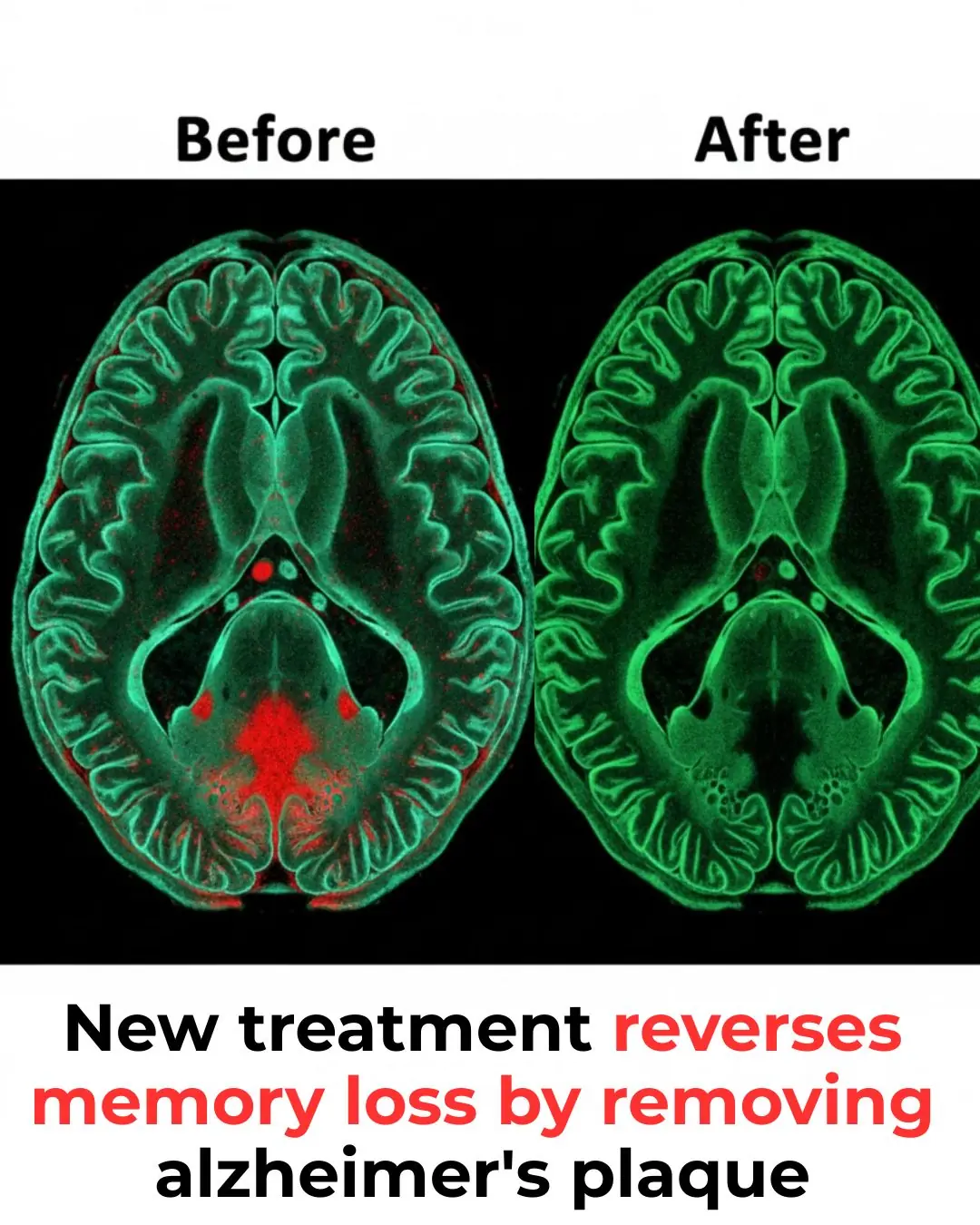
Alzheimer’s Breakthrough: A New Era in Reversing Memory Loss
A Flash of Light at the Start of Life: The Mystery of the Zinc Spark

The Psychological Meaning of Leaving Dirty Dishes
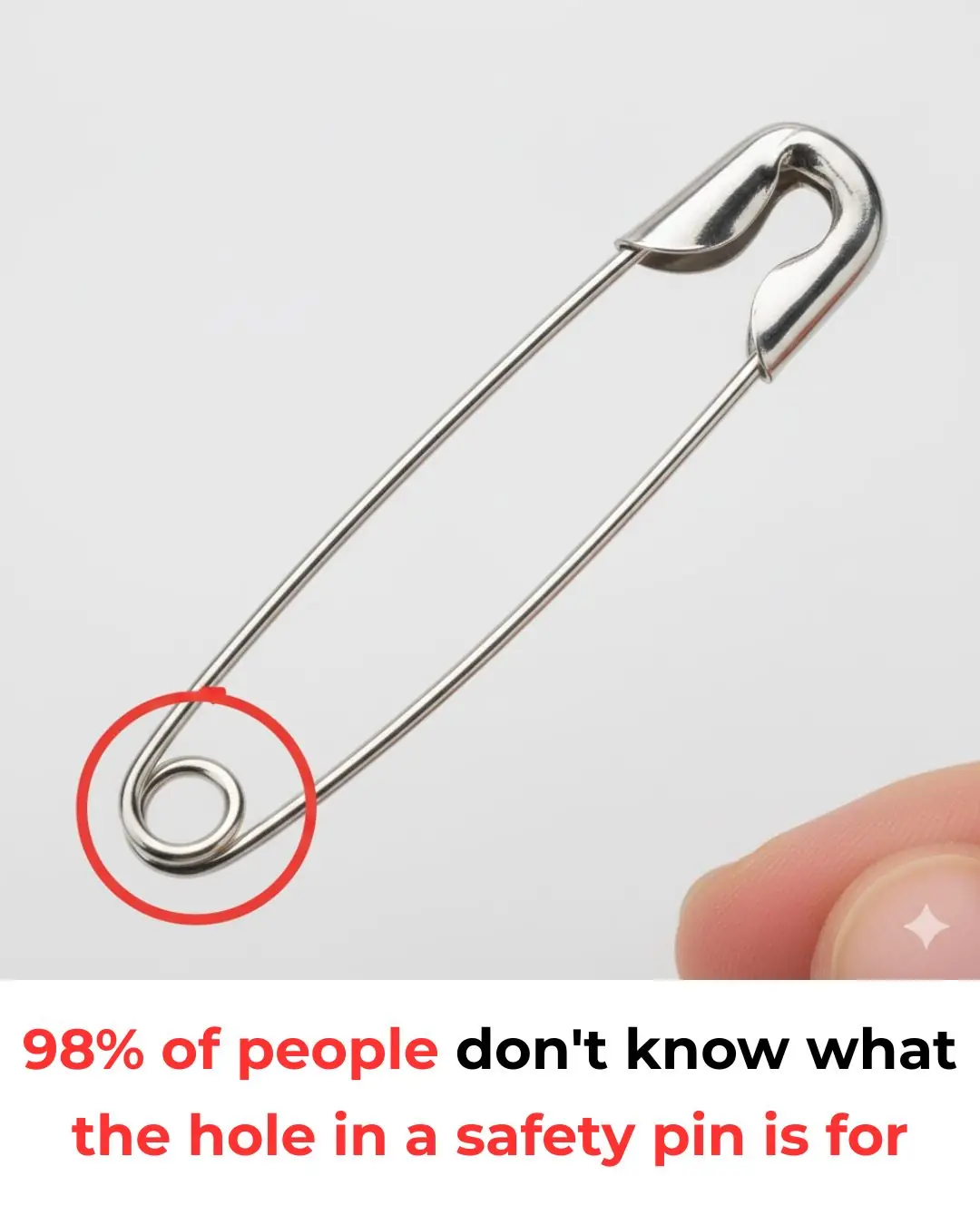
What’s the Purpose of That Tiny Hole in a Safety Pin
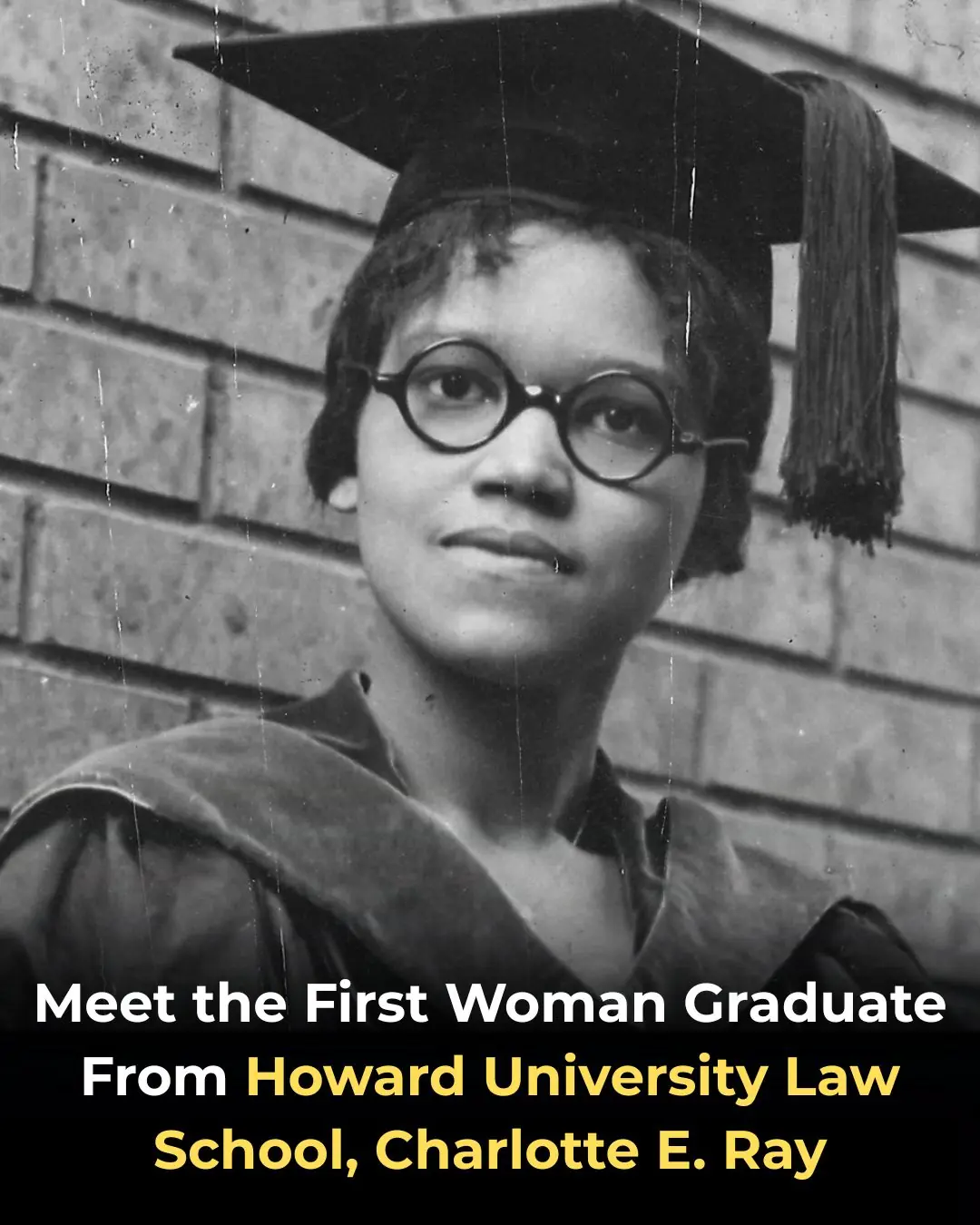
Meet the First Woman Graduate From Howard University Law School, Charlotte E. Ray
Beating Seasonal Depression: 8 Directories To Help You Find An Affordable Black Therapist

Hip-Hop Pioneer Rakim Launches New ‘Notes’ Fintech Platform to Empower Independent Artists
New ‘Eddie’ Documentary About Comedy Legend Eddie Murphy Is Coming to Netflix
Remembering Roberta Flack, Legendary Songstress, Educator, and Howard University Alumna
News Post

A Breakthrough in the Global Search for an HIV Vaccine: From Impossible to Truly Hopeful

This Old-School Home Remedy Could Ease Back, Joint & Knee Pain in Just 7 Day

The Daily Drink That Helps Clear Blocked Arteries Naturally

12 Benefits of Bull Thistle Root and How to Use It Naturally

8 Warning Signs of Colon Cancer You Should Never Ignore

Explore Canada from Coast to Coast by Train for Just $558 🇨🇦: A 3,946-Mile Adventure Through Stunning Landscapes

Golden Snub-Nosed Monkeys: A Glimpse of Wild Beauty in the Misty Mountains of China

Understanding the Extended Recovery Journey After Pregnancy
Study: nearly all heart attacks and strokes linked to 4 preventable factors
4 Things You Should Never Throw Away After a Funeral — And Why They Matter More Than You Realize

Stop adding butter — eat these 3 foods instead for faster weight loss

Chicken Eggs with Mugwort: Highly Beneficial but Certain People Should Avoid Them

Watercress: The World’s Top Anti-Cancer Vegetable You Can Find in Vietnamese Markets
4 Plants That Snakes Absolutely Love — Remove Them Immediately to Keep Your Home Safe
The 4 “Golden Hours” to Drink Coffee for Maximum Health Benefits — Cleaner Liver, Better Digestion, Sharper Mind
Don’t Rip This Out — Treat It Like Gold Instead. Here’s Why.

Say Goodbye to Bare Branches: Revive Your Christmas Cactus Blooms with These Expert-Backed Hacks

Were You Aware of This? A Surprisingly Simple Spoon Trick Can Stop Mosquito Bite Itching
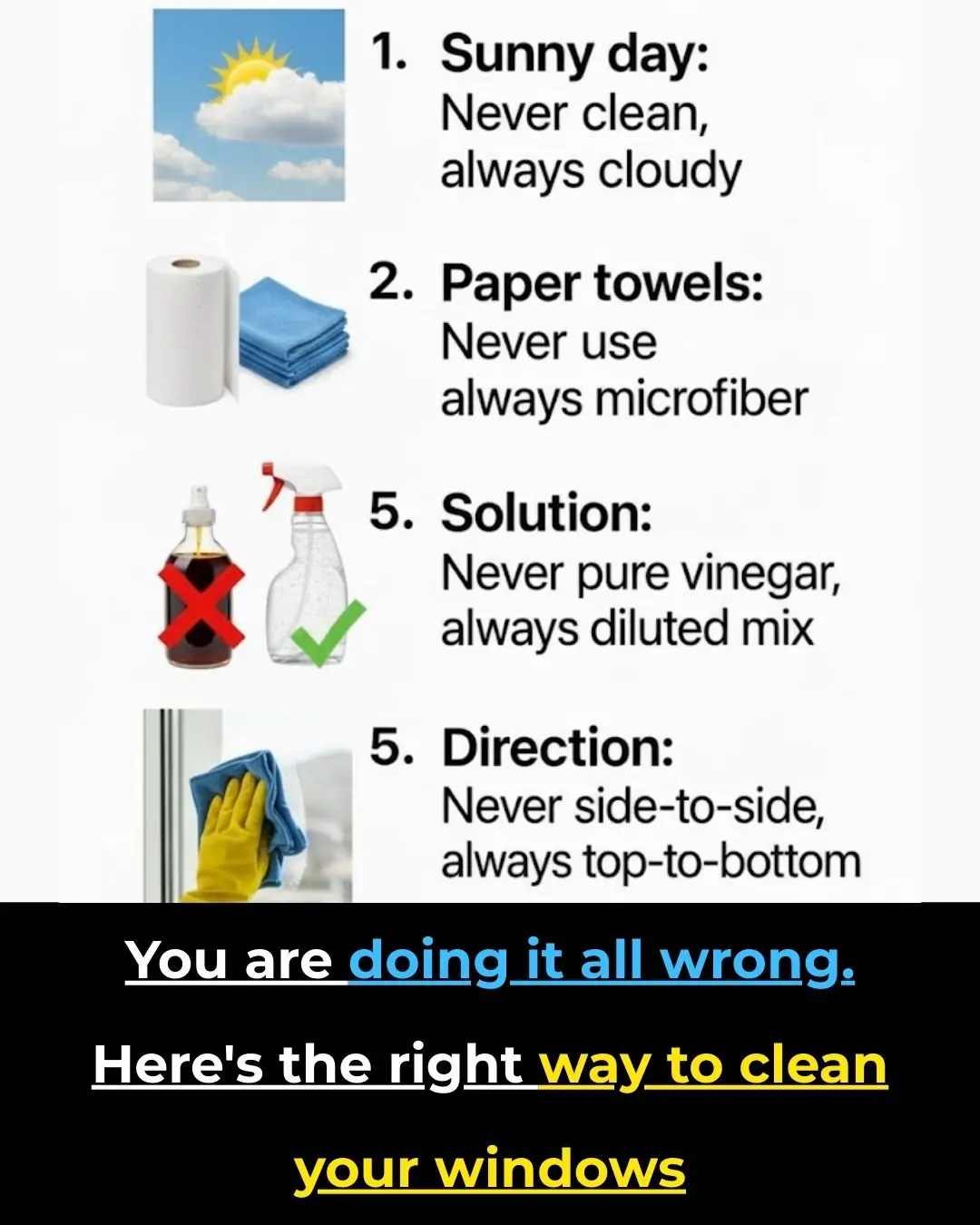
You’re Doing It All Wrong — Here’s the Right Way to Clean Your Windows
