What to Expect After Gallbladder Surgery: Side Effects and Dietary Tips
Gallbladder surgery, while common, can bring about surprising changes in your digestion, energy, and eating habits. Understanding what’s normal—and what’s not—after the procedure can help you recover faster and avoid long-term discomfort.
Here’s a detailed look at the potential side effects, why they happen, and the best dietary adjustments to support your digestive health after gallbladder removal.

Understanding Your Gallbladder and Why It’s Removed
Your gallbladder is a small, pear-shaped organ located just beneath your liver. Its main job is to store and release bile—a digestive fluid that helps break down dietary fats—into the duodenum. While small, this organ can be affected by a variety of conditions, including gallstones, acute cholecystitis (inflammation), gallstone-related pancreatitis, and in rare cases, gallbladder tumors.
When gallbladder function is compromised or becomes a source of recurring health issues, the most common treatment is a cholecystectomy, or surgical removal of the gallbladder. Although the body can function without it, patients may experience several short-term and, occasionally, long-term effects that require lifestyle adjustments.
Physical Changes After Gallbladder Surgery
Most people live a completely normal life without a gallbladder, but the absence of this organ alters how bile is delivered to your digestive system. Instead of being stored and released in measured amounts, bile now flows continuously into the small intestine. While this might not sound like a big deal, it can cause:
- Diarrhea and loose stools – According to the Mayo Clinic, up to 20% of patients report ongoing diarrhea after surgery due to bile irritating the bowel lining.
- Bloating and gas – Without a gallbladder to regulate bile release, fat digestion is less efficient, often leading to indigestion and uncomfortable bloating in the first few weeks.
- Post-Cholecystectomy Syndrome – Around 5–40% of patients develop this condition, which can cause nausea, abdominal discomfort, and upper right-side pain due to irregular bile flow.
- Bile duct stones (Choledocholithiasis) – Even without a gallbladder, stones can form in the bile duct, leading to infection or pain—though this is rare.
- Bile acid malabsorption – Experienced by 5–10% of patients, this occurs when excess bile enters the colon faster than it can be reabsorbed, sometimes resulting in chronic diarrhea and reduced fat absorption.

Appetite and Weight Changes
After surgery, some individuals find that their digestive system reacts strongly to fatty or greasy foods. For many, this is a temporary adjustment, but some need to permanently limit high-fat meals. Weight fluctuations can also occur—not because of the surgery itself, but due to changes in appetite, food tolerance, and dietary choices during recovery.
In the immediate days post-surgery, doctors typically recommend:
- First 1–3 days: Clear liquids, broth, and gelatin to allow the digestive system to rest.
- Avoiding alcohol for at least 48 hours to reduce strain on the liver and digestive tract.
- Gradually reintroducing solids with small, frequent meals that are gentle on the stomach.
Best Foods to Eat After Gallbladder Surgery
While there’s no universal “gallbladder removal diet,” certain foods can help reduce discomfort and aid recovery:
- Hydration is key – Drink water, herbal teas, or electrolyte-rich broths to replace fluids lost from diarrhea.
- Low-fat options – Beans, oatmeal, whole grains, vegetables, fruits, and fat-free dairy reduce the risk of bloating and diarrhea.
- High-fiber foods (introduced gradually) – Prunes, oat bran, chickpeas, beets, and okra help regulate digestion.
- Soluble fiber sources – Wheat germ, legumes, carrots, nuts, potatoes, and spinach support smoother bowel movements.
Foods to Limit or Avoid During Recovery
To minimize discomfort, steer clear of:
- High-fat items – Bacon fat, lard, butter, processed meats, and fried snacks.
- Spicy foods with capsaicin – Can irritate the stomach lining.
- Dairy with high fat content – Such as whole milk, cream, or rich cheeses.
- Sugary or caffeinated products – These can worsen diarrhea and digestive upset.
Keeping a food journal can help identify specific triggers, making it easier to transition back to a normal diet. Most patients resume a regular eating pattern within 4–6 weeks, although long-term moderation of fatty foods often benefits digestion.
News in the same category


The Power of Fig Leaves: Hidden Health Benefits You Should Know

The One Leaf That Naturally Supports Blood Sugar, Blood Pressure & More

Seniors: Discover These 3 Everyday Seeds That May Support Healthy Eyes & Retina as You Age

A refreshing natural drink packed with eye-supporting nutrients like beta-carotene, lutein, and zeaxanthin from fresh carrots, cucumber, and ginger might just become your new daily habit for supporting healthy vision.

Doctor issues warning about eating too much rice
Colonoscopy: The key question you should ask your doctor before the procedure

Itchy Breasts? Here Are 6 Health Issues That Could Be Behind It

Woman lost both kidneys before turning 30: Doctor warns of 2 habits that cause kidney failure

Doctors reveal that eating bananas before bed can lead to... See more

The Silent Signal: What Your Legs May Reveal About Pancreatic Health
Does Sniffing Rosemary Really Boost Memory
Number Of Triangles You See Will Reveal Your True Personality
8 Foods You Should Eat Instead of Taking a Vitamin C Supplement

Right-Side Abdominal Pain in Women: Could It Be Gallstones?
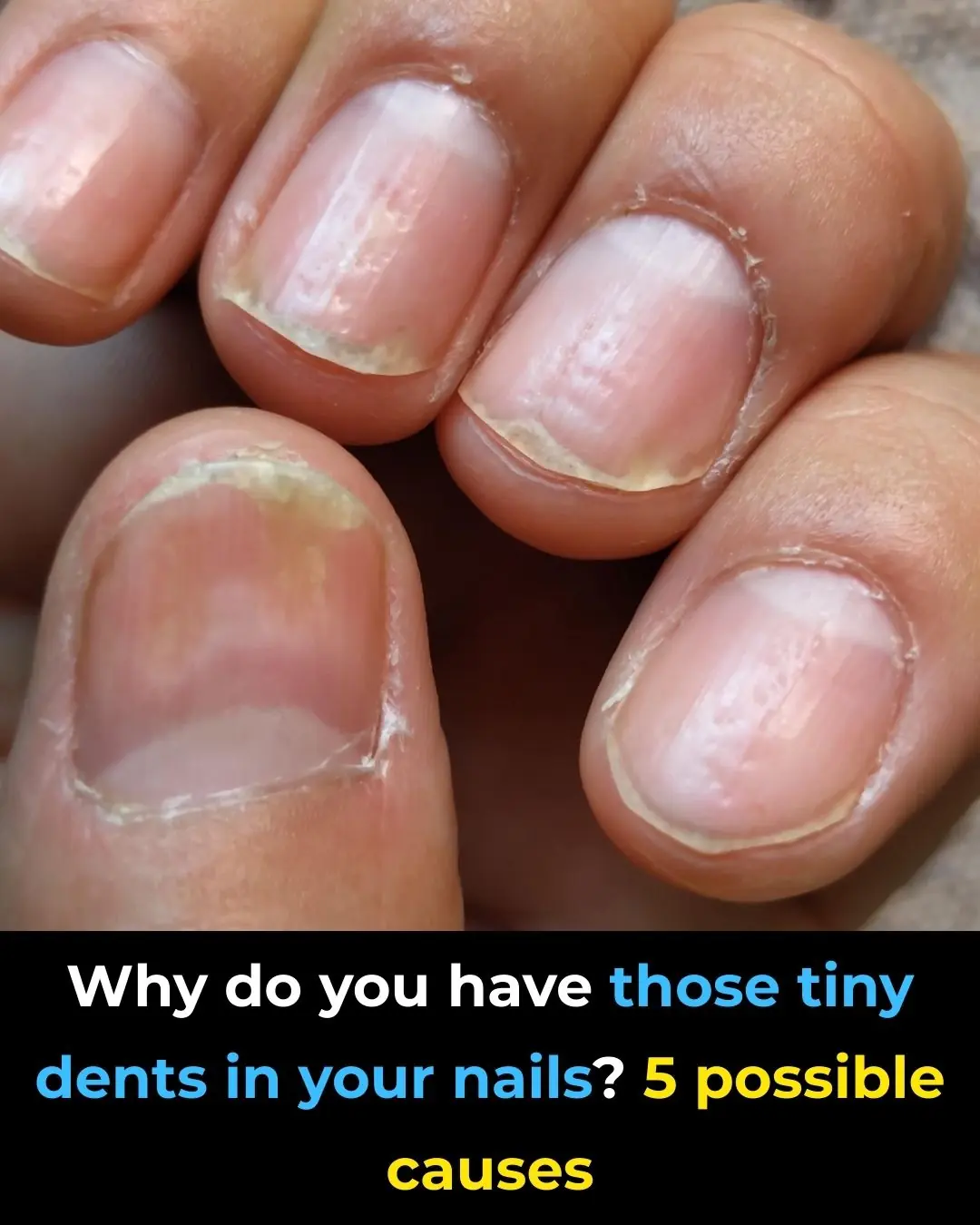
Everything You Need To Know About Nail Pitting
🧠 8 Strange (But Real) Signs Your Body Is Begging for More Vitamin B12 – Don’t Ignore These Red Flags

Discovering Smart Protein Choices: 4 to Include and 5 to Limit for Kidney Health Support

How I Improved the Appearance of My Legs: Smoother, Brighter & Healthier-Looking Skin with Simple Habits

Discover 5 Everyday Foods That May Increase Cancer Risk and Simple Swaps for Better Health
News Post

Flight Attendant Tortured Black Twins Until They Passed Out, Crew Freezes When Their CEO Dad Arrives.

Blood sugar drops instantly with this red onion recipe! A true culinary treasure that few know about!

I Am A Billionaire Ceo, But I Was Completely Powerless When My Baby Wouldn’t Stop Screaming On A 10-hour Flight

The Power of Fig Leaves: Hidden Health Benefits You Should Know

The One Leaf That Naturally Supports Blood Sugar, Blood Pressure & More

Seniors: Discover These 3 Everyday Seeds That May Support Healthy Eyes & Retina as You Age

A refreshing natural drink packed with eye-supporting nutrients like beta-carotene, lutein, and zeaxanthin from fresh carrots, cucumber, and ginger might just become your new daily habit for supporting healthy vision.

POOR TWIN SISTERS BUY GROCERIES AND FIND A BILLIONAIRE IN THE BASEMENT–WHAT HAPPENS NEXT SHOCKS ALL

For two decades, I was the neighbor no one noticed—the quiet man who trimmed his hedges, fixed bikes, and never argued

Here is what this little hole on the ear mean

Doctor issues warning about eating too much rice
Colonoscopy: The key question you should ask your doctor before the procedure

Itchy Breasts? Here Are 6 Health Issues That Could Be Behind It

Woman lost both kidneys before turning 30: Doctor warns of 2 habits that cause kidney failure

Understanding the Body After 70
A Father’s Unexpected Return Exposed Everything

Doctors reveal that eating bananas before bed can lead to... See more

Racist Passenger Insulted Black Man in Economy — Turns Out He Owns the Airline

The Silent Signal: What Your Legs May Reveal About Pancreatic Health