
Chronic Gut and Metabolic Disorders May Signal Alzheimer’s and Parkinson’s Years in Advance
Chronic Health Conditions May Signal Alzheimer’s and Parkinson’s Years in Advance
A recent large-scale study published in Science Advances suggests that certain chronic health conditions—particularly those related to gut function and metabolic health—may act as early warning signs for Alzheimer’s and Parkinson’s diseases. By systematically analyzing data from more than 150 different health disorders, researchers found that several non-neurological conditions were associated with a significantly higher risk of developing these neurodegenerative diseases many years before classic symptoms such as memory loss or movement difficulties become apparent.
Neurodegenerative diseases like Alzheimer’s and Parkinson’s are typically diagnosed only after noticeable brain-related symptoms emerge, at which point substantial and often irreversible damage has already occurred. Identifying early indicators outside the brain could therefore be crucial for prevention and early intervention. The new findings support a growing scientific consensus that these diseases are not confined to the brain alone, but are closely connected to broader systemic changes throughout the body.
For Alzheimer’s disease, the study identified several conditions that were consistently associated with increased risk. These include irritable bowel syndrome (IBS), vitamin D deficiency, type 2 diabetes, and a range of gastrointestinal disorders. Individuals diagnosed with these conditions were more likely to develop Alzheimer’s later in life compared to those without such health issues. Similarly, for Parkinson’s disease, researchers found strong associations with IBS, vitamin D deficiency, and type 2 diabetes, highlighting notable overlaps in early risk factors between the two disorders.
One of the most striking aspects of the study is the importance of timing. Chronic conditions diagnosed approximately 10 to 15 years before the onset of neurological symptoms showed the strongest links to both Alzheimer’s and Parkinson’s diseases. This suggests that the disease process may begin decades earlier than previously assumed, reinforcing the idea that neurodegeneration is a long, gradual process rather than a sudden event. These findings align with earlier research reported in Nature Reviews Neurology, which emphasizes the extended preclinical phase of neurodegenerative diseases.
The gut-brain connection appears to play a particularly important role. Increasing evidence indicates that the gut microbiome influences inflammation, immune responses, and even the production of neurotransmitters. Disruptions in gut health, such as those seen in IBS and other gastrointestinal disorders, may contribute to chronic inflammation that affects the brain over time. Institutions such as the U.S. National Institutes of Health (NIH) and the World Health Organization (WHO) have highlighted systemic inflammation and metabolic dysfunction as key contributors to age-related brain diseases.
Metabolic conditions, especially type 2 diabetes, are also of growing concern. Poor blood sugar control has been linked to vascular damage, insulin resistance in the brain, and increased inflammation—all factors associated with cognitive decline. Some researchers have even referred to Alzheimer’s disease as “type 3 diabetes,” a concept discussed by experts cited by the Alzheimer’s Association. Meanwhile, vitamin D deficiency has been associated with impaired immune regulation and neuroprotection, further underscoring its potential role in neurodegenerative risk.
The study strongly emphasizes the importance of early detection and proactive management of chronic health conditions. Addressing gut health, maintaining adequate vitamin D levels, and controlling blood sugar may not only improve overall well-being but could also reduce the long-term risk of developing Alzheimer’s or Parkinson’s disease. Organizations such as the Parkinson’s Foundation and the Alzheimer’s Association increasingly advocate for a holistic, whole-body approach to brain health, rather than focusing solely on neurological symptoms.
Overall, this research highlights the deep interconnectedness of bodily systems and their collective influence on brain health. It suggests that protecting the brain may begin far earlier than previously thought—through routine management of chronic conditions that, at first glance, seem unrelated to neurodegeneration. As scientists continue to uncover these early links, such insights could transform how Alzheimer’s and Parkinson’s diseases are predicted, prevented, and ultimately treated.
News in the same category

The First-Ever Leucistic Iberian Lynx Captured on Camera: A Rare and Powerful Symbol of Hope

Ultra-Processed Foods Linked to Increased Psoriasis Flare-Ups, Study Finds

Giant Pandas Officially Move Off the Endangered Species List: A Historic Conservation Triumph

Mexico City Passes Landmark Law Banning Violent Practices in Bullfighting: A Controversial Move Toward "Bullfighting Without Violence"

A Magical Bond: The Unlikely Friendship Between a Blind Dog and a Stray Cat in Wales

Syros Cats: A Sanctuary for Feline Rescue and Compassion in Greece

The World Bids Farewell to Bobi, the World's Oldest Dog, at the Age of 31

The Cost of a Trip to Tokyo Disney is Now Cheaper Than Going to Disney in Florida
Loss of Smell May Be One of the Earliest Warning Signs of Alzheimer’s Disease
Groundbreaking Stem Cell Discovery Offers Hope for Rebuilding Myelin and Reversing Nerve Damage in Multiple Sclerosis

China Breaks Magnetic Field Record with Groundbreaking 351,000 Gauss Achievement
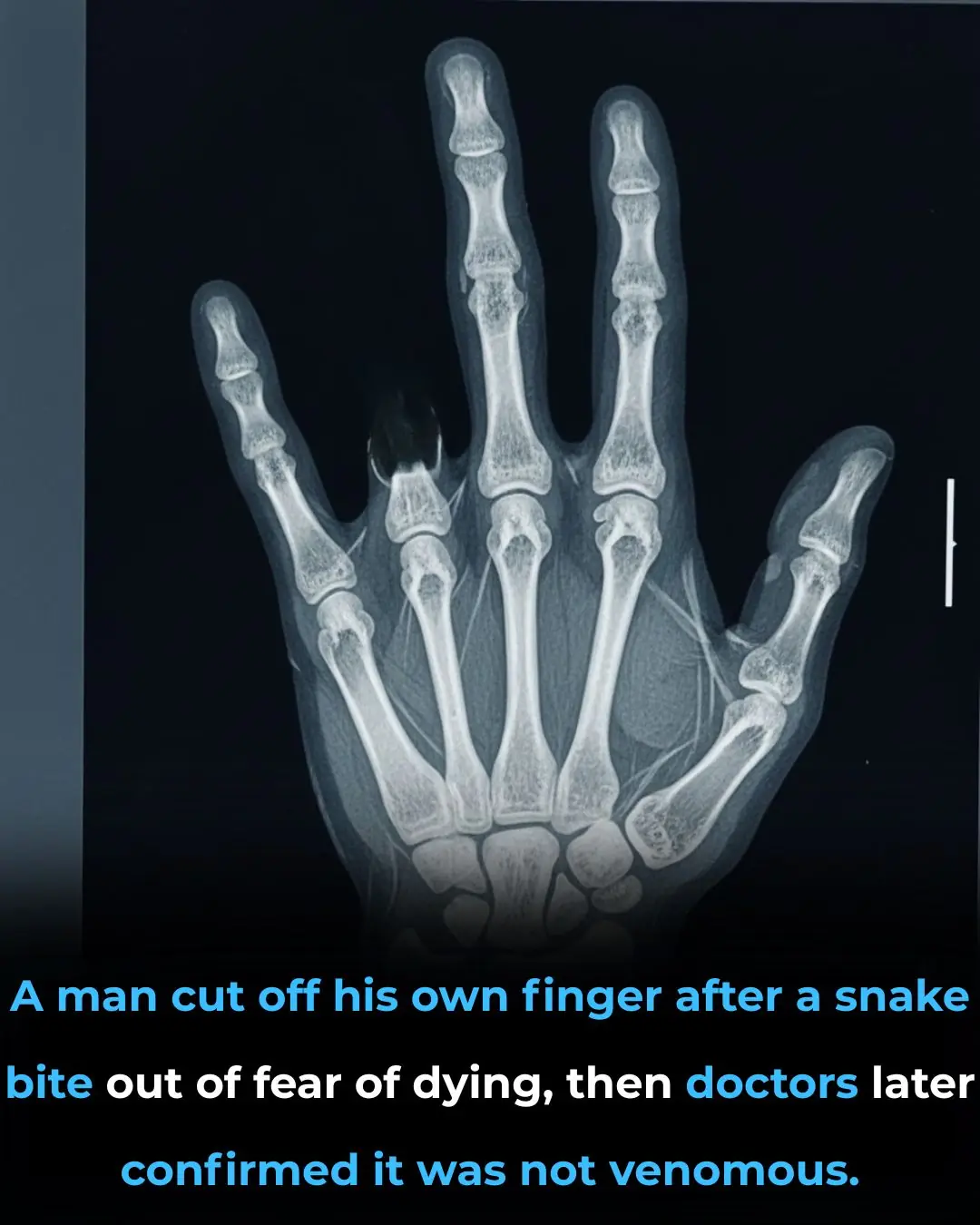
Man in China Cuts Off Finger After Snake Bite, Fearing Venomous Attack – Doctors Confirm It Was Harmless
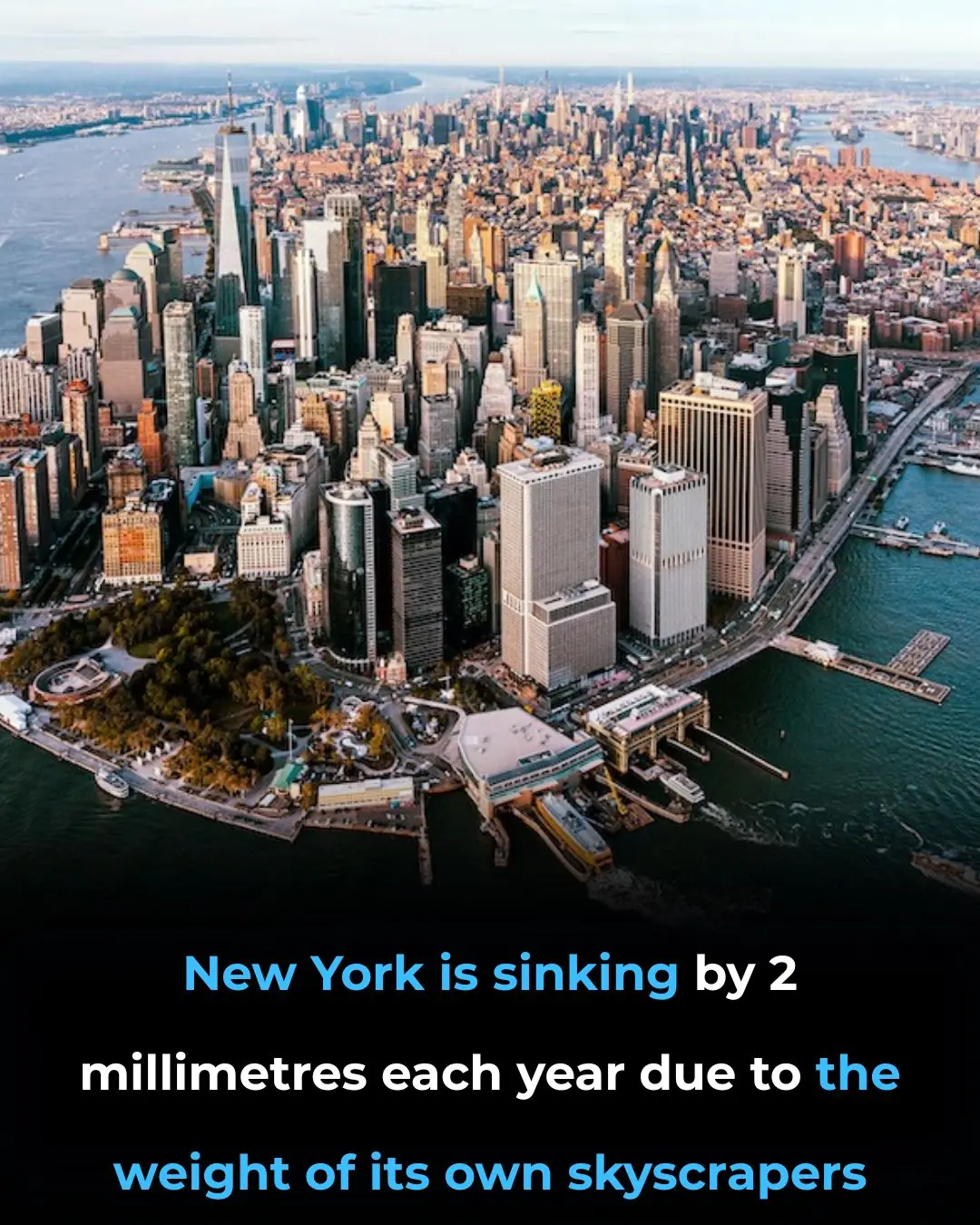
New Study Reveals New York City is Sinking: A Growing Threat from Subsidence and Rising Seas

Russia Blocks Access to Roblox Amid Growing Crackdown on Foreign Tech and LGBTQ+ Content

Mercedes Launches Premium Strollers in Collaboration with Hartan, Targeting the Luxury Baby Gear Market
Promising Signs of a Potential Long-Term HIV Cure: A Breakthrough Study from UCSF
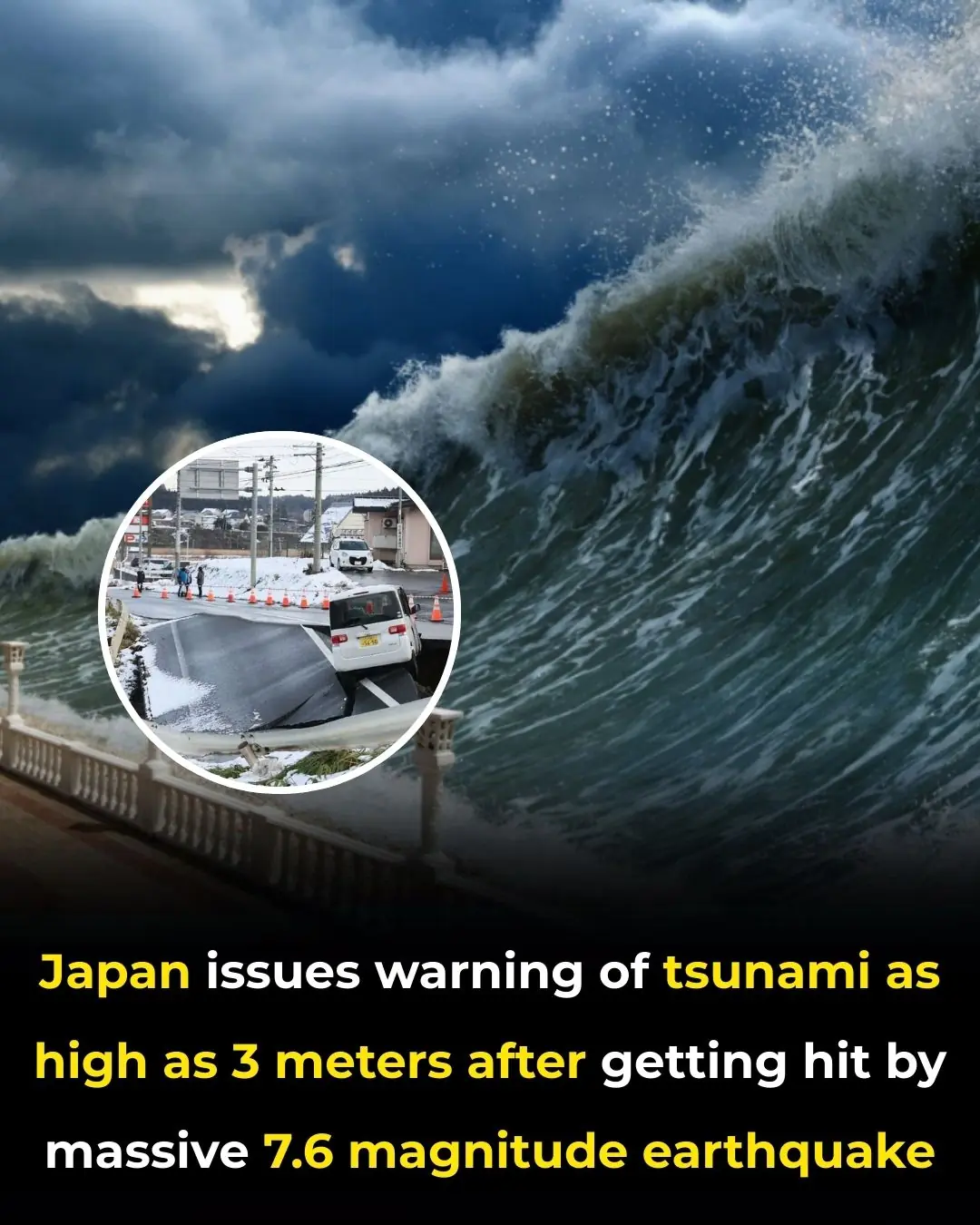
Japan Issues Tsunami Warning Following 7.6 Magnitude Offshore Earthquake

Elephant Burial Practices: A Deep and Emotional Connection to the Dead
News Post

Over 1,800 Lawsuits Filed Against Ozempic, Alleging Severe Side Effects and Misleading Marketing
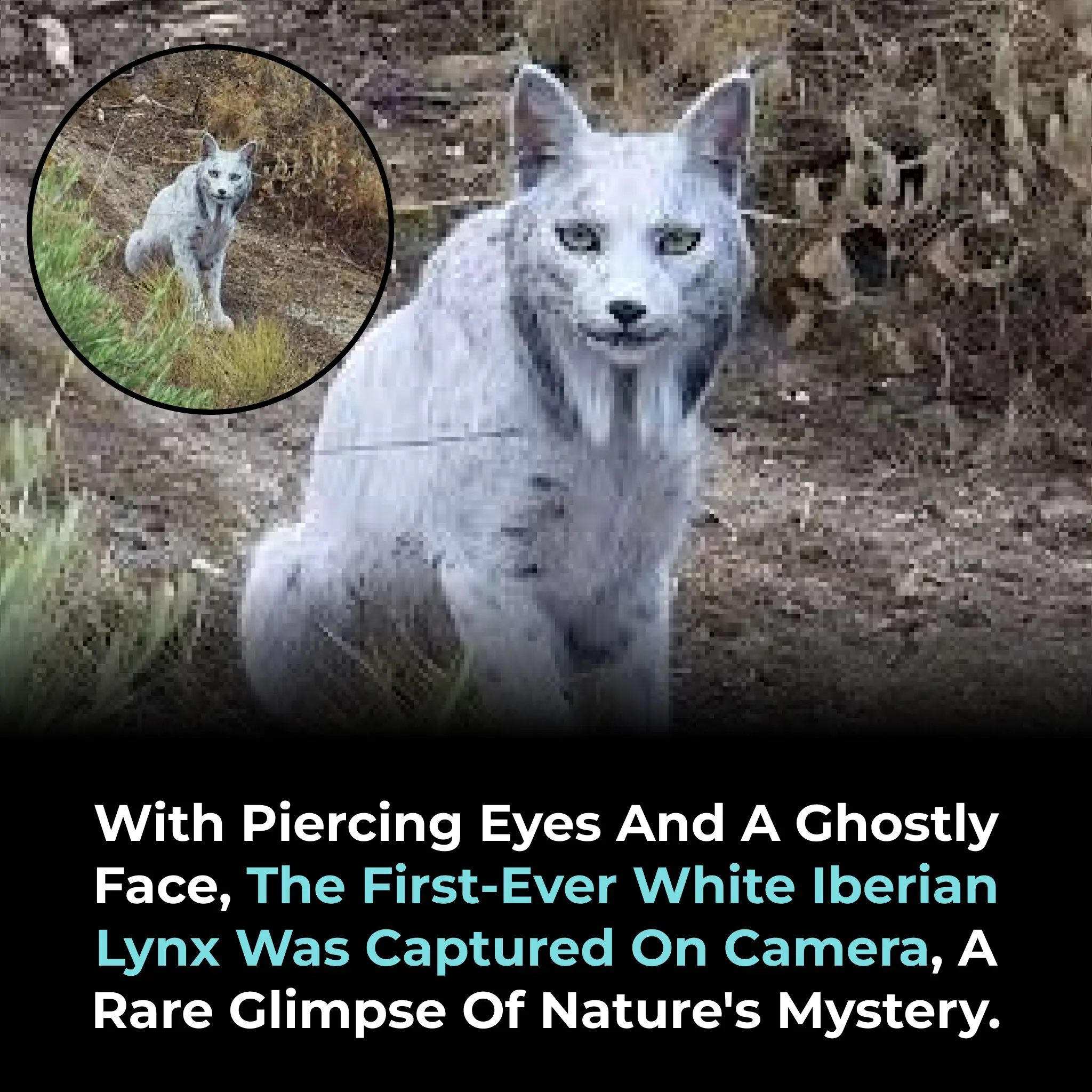
The First-Ever Leucistic Iberian Lynx Captured on Camera: A Rare and Powerful Symbol of Hope

Ultra-Processed Foods Linked to Increased Psoriasis Flare-Ups, Study Finds

Giant Pandas Officially Move Off the Endangered Species List: A Historic Conservation Triumph

Twin Study Reveals Gut Microbiome's Role in Multiple Sclerosis Development

Mexico City Passes Landmark Law Banning Violent Practices in Bullfighting: A Controversial Move Toward "Bullfighting Without Violence"

World-First Breakthrough: Base-Edited Gene Therapy Reverses "Incurable" T-Cell Leukemia

Daily Tefillin Use Linked to Improved Blood Flow and Lower Inflammation

A Magical Bond: The Unlikely Friendship Between a Blind Dog and a Stray Cat in Wales

Daily Whole Orange Consumption Associated with 30% Reduction in Fatty Liver Prevalence

Phase I Trial: White Button Mushroom Powder Induces Long-Lasting PSA Responses in Prostate Cancer
Tea Supports Bone Density While High Coffee Intake Linked to Bone Loss in Older Women

Syros Cats: A Sanctuary for Feline Rescue and Compassion in Greece
Rapamycin Reduces Lung Tumor Count by Up to 90% in Tobacco-Exposed Models
51-Year-Old Man Declared Cured of HIV Following Stem Cell Transplant for Leukaemia
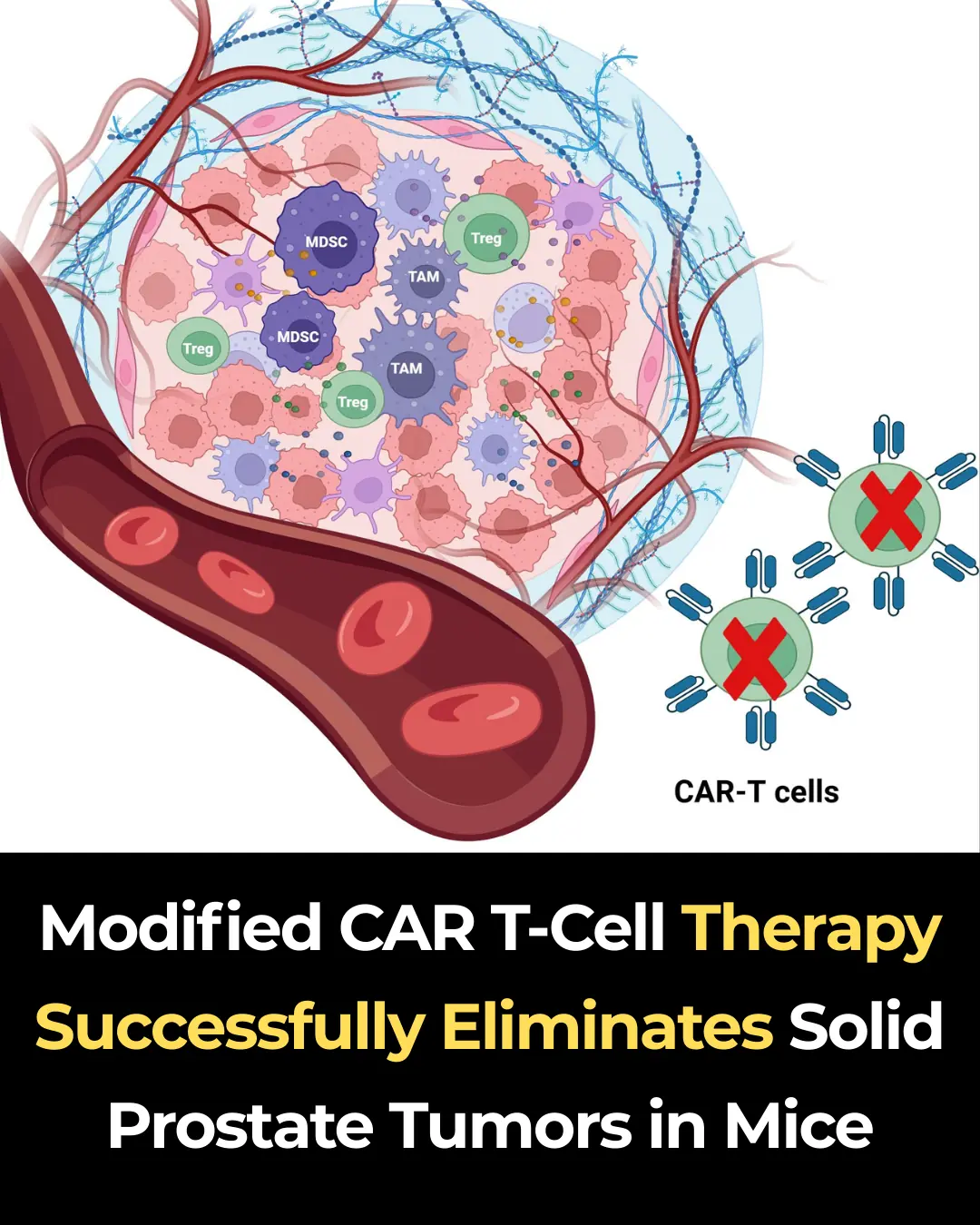
Modified CAR T-Cell Therapy Successfully Eliminates Solid Prostate Tumors in Mice

The World Bids Farewell to Bobi, the World's Oldest Dog, at the Age of 31

The Gut-First Approach: Berberine’s Impact on Microbiome Balance and Barrier Integrity
