Epstein–Barr Virus May Reprogram B Cells and Drive Autoimmunity in Lupus
Epstein–Barr virus (EBV), one of the most common human viruses worldwide, may play a direct and active role in the development of systemic lupus erythematosus (SLE) by reprogramming autoreactive B cells, according to new research. The findings provide important mechanistic insight into how chronic viral infection could trigger and sustain autoimmune disease.
Systemic lupus erythematosus is a complex autoimmune disorder characterized by widespread inflammation and the production of autoantibodies that attack the body’s own tissues. Although genetic susceptibility is known to contribute to SLE risk, environmental triggers—including viral infections—have long been suspected to play a crucial role in disease onset and progression.
A Long-Suspected Link Between EBV and Lupus
Epstein–Barr virus infects more than 90% of the global population and typically persists for life in a latent form within B lymphocytes. Previous epidemiologic studies have shown that nearly all patients with SLE have evidence of prior EBV infection, often with higher viral loads and altered immune responses compared with healthy individuals.
However, until recently, the precise biological mechanisms linking EBV infection to lupus pathogenesis remained unclear.
New Insights Into B Cell Reprogramming
Recent research reveals that EBV does not merely infect B cells passively in patients with lupus. Instead, the virus appears to actively reprogram autoreactive B cells, transforming them into highly activated antigen-presenting cells capable of amplifying autoimmune responses.
In patients with SLE, EBV-infected B cells demonstrated markedly increased antigen-presenting capabilities compared with EBV-infected B cells from healthy controls. These altered cells were more effective at presenting self-antigens to T cells, a key step in initiating and sustaining autoimmune inflammation.
This phenomenon was not observed in individuals without autoimmune disease, suggesting that EBV interacts differently with the immune system in genetically or immunologically susceptible hosts.
How EBV May Drive Autoimmune Activation
The study suggests several mechanisms by which EBV-infected B cells may contribute to lupus:
-
Enhanced antigen presentation, increasing activation of autoreactive T cells
-
Persistent immune stimulation, preventing immune tolerance
-
Promotion of inflammatory signaling pathways, sustaining chronic immune activation
-
Expansion of autoreactive B cell populations, leading to increased autoantibody production
By converting normally regulated B cells into potent immune activators, EBV may act as a continuous driver of systemic autoimmunity rather than a one-time trigger.
Differences Between Lupus Patients and Healthy Individuals
A key finding of the research was the stark contrast between EBV-infected B cells in patients with SLE and those in healthy individuals. While EBV infection is common in both groups, only lupus patients exhibited B cells with abnormal immune activation and antigen-presenting behavior.
This distinction suggests that host immune context matters greatly. Genetic predisposition, altered immune regulation, or defects in viral control may allow EBV to exert pathogenic effects specifically in patients with lupus.
Implications for Understanding Lupus Pathogenesis
These findings strengthen the hypothesis that lupus is not driven solely by intrinsic immune dysfunction but may also be fueled by chronic viral interactions. EBV’s ability to manipulate immune cells adds a critical environmental dimension to the disease.
Understanding this relationship could help explain why lupus flares are often associated with immune stressors and why the disease is difficult to control once established.
Potential Therapeutic Implications
If EBV-infected B cells are confirmed as key drivers of lupus activity, new therapeutic strategies may emerge, including:
-
Targeting EBV-infected B cells specifically
-
Developing antiviral therapies aimed at EBV latency
-
Designing vaccines to prevent or modify EBV infection
-
Refining B cell–directed therapies to disrupt antigen presentation
Current lupus treatments largely focus on suppressing immune activity broadly. Targeting the viral–immune interaction could offer more precise and potentially safer treatment options.
Broader Significance for Autoimmune Disease Research
Beyond lupus, the findings may have implications for other autoimmune diseases that have been linked to EBV, including multiple sclerosis and rheumatoid arthritis. The study supports the broader concept that chronic viral infections can reshape immune cell function in ways that promote autoimmunity.
Conclusion
Emerging evidence suggests that Epstein–Barr virus may play an active and ongoing role in systemic lupus erythematosus by reprogramming autoreactive B cells into highly effective antigen-presenting cells. This viral-driven immune dysregulation may help explain the persistence and severity of autoimmune responses in lupus patients.
While further research is needed to confirm these findings and translate them into clinical therapies, the study marks a significant step forward in understanding how viral infections and immune dysfunction intersect to drive complex autoimmune diseases like lupus.
News in the same category


The Best Scientifically Proven Foods to Cleanse Your Liver

5 Common Habits That Quietly Damage Your Knees
Why Hot Dogs and Processed Meat Might Be the Most Dangerous Foods of All Time
Oral Semaglutide Fails to Slow Cognitive Decline in Early Alzheimer’s Disease, Phase 3 Trials Show
Early Use of Glucocorticoids May Reduce Mortality in Community-Acquired Pneumonia
11 Best and Worst Foods for Boosting Metabolism

Three Ideal Times to Eat Boiled Eggs for Effective Weight Loss and Stable Blood Sugar
A 58-Year-Old Man Ate One Clove of Garlic Every Morning — His Medical Checkup Six Months Later Surprised Doctors
Periodontal Treatment as a Strategy for Cardiovascular and Cerebrovascular Protection
Frequency-Specific Electromagnetic Fields and Cancer Cell Behavior: Evidence and Limitations

Saffron as a Potential Antidepressant: Evidence from Clinical Trials
Metabolic Effects and Limitations of an Extreme Single-Food Diet: Insights from a Sardine-Based Experiment
The Therapeutic Role of Glutamine in Post-Infectious Irritable Bowel Syndrome
The Anti-Inflammatory Potential of Yogurt in Human Health
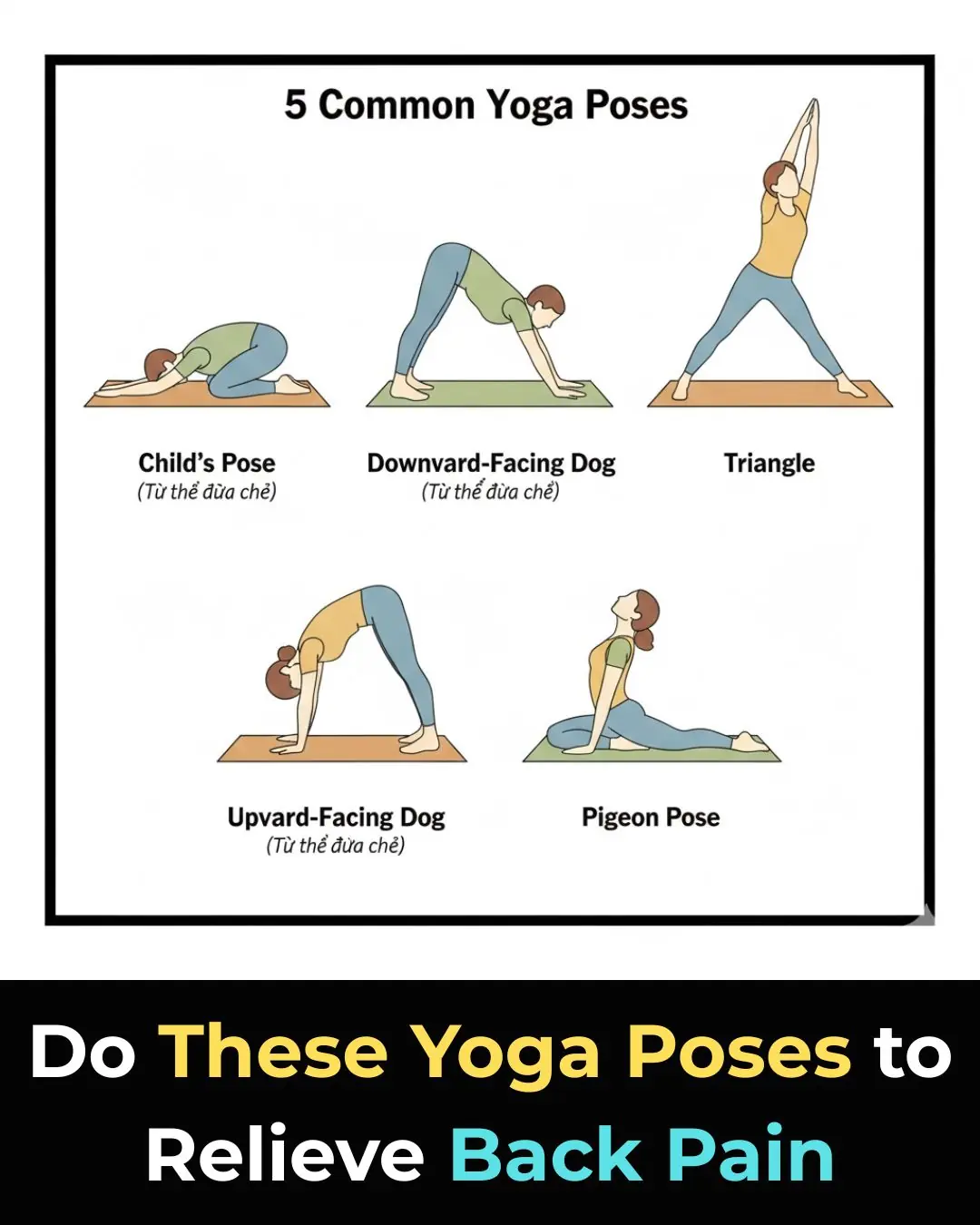
7 Yoga Poses That Can Help Relieve Lower Back Pain

How To Get Rid Of Eczema: 13 Natural Remedies Backed By Research

Scientists Explain The Effects of Eating Too Much Sugar
10 Simple Ways to Help Your Body Detoxify and Cleanse Itself
News Post

Best Vitamins & Foods for Hair Growth

Homemade Carrot Gel for Glowing Skin & Wrinkles

Potato Toner for Face – Dark Spots, Clear Skin & Pigmentation

after an argument, my husband kicked me out and left me at a bus stop outside the city with no money.

after receiving a huge inheritance, natalya decided to see her husband’s true colors.

after the divorce, my husband threw me out the door without a single penny. i decided to check the old card that my father once gave me, but the banker turned pale and whispered: “madam… you need to see this!” i froze in shock when i found out that

My husband went on a secret trip with his lover and 4 members of her family. When they returned, the house had already been sold. I had packed everything up and moved abroad…

I want to divorce my cheating husband, but the husband of the other woman showed up and gave me $100M, saying: ‘Don’t divorce him just yet, just wait for 3 more months.

My husband SLAPPED my mouth in front of his COWORKERS because of a JOKE. He did not realize that he just ended his own CAREER.

Why Walking After Eating Is So Good for You
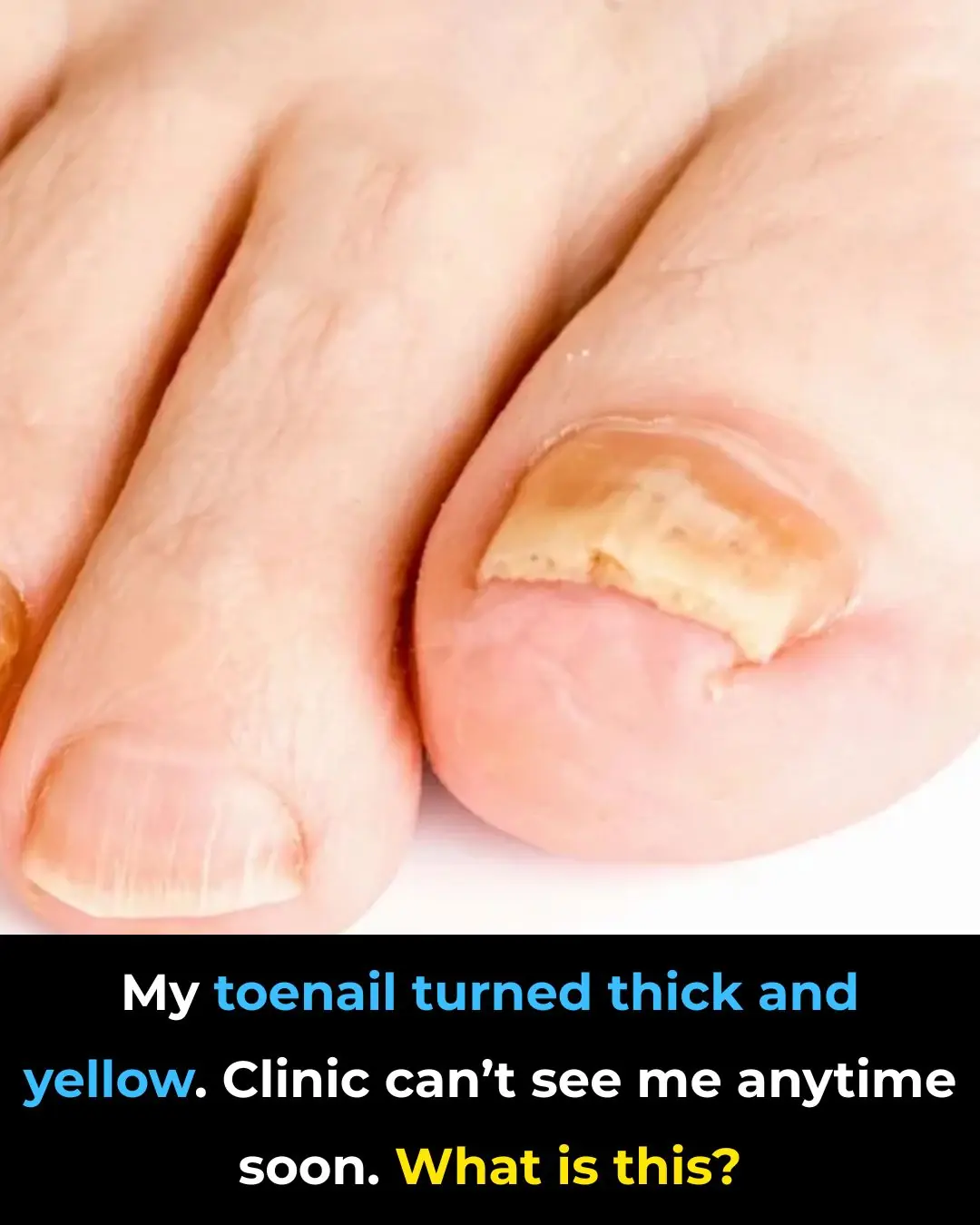
My toenail turned thick and yellow. Clinic can’t see me anytime soon. What is this?

This changes everything

The Best Scientifically Proven Foods to Cleanse Your Liver

5 Common Habits That Quietly Damage Your Knees
Why Hot Dogs and Processed Meat Might Be the Most Dangerous Foods of All Time
Oral Semaglutide Fails to Slow Cognitive Decline in Early Alzheimer’s Disease, Phase 3 Trials Show

Tips for stir-frying noodles to make them chewy and delicious with less oil: Don't blanch the noodles in boiling water.
Early Use of Glucocorticoids May Reduce Mortality in Community-Acquired Pneumonia