Foodborne Pathways of Urinary Tract Infections: The Emerging Role of Meat Consumption
Emerging scientific evidence suggests that diet—particularly the consumption of certain meats—may play a larger role in urinary tract infections (UTIs) than previously understood. Traditionally, UTIs have been viewed as infections caused by bacteria already present in the body, especially those originating from the bladder or gastrointestinal tract. However, new research indicates that a significant proportion of UTIs may actually be linked to foodborne exposure, especially through contaminated meat.
A large-scale study analyzing thousands of Escherichia coli (E. coli) samples from patients diagnosed with UTIs compared these strains with E. coli found in retail meat from the same geographic communities. The findings were striking: approximately 18–20 percent of UTIs were associated with bacterial strains genetically traced back to meat sources. Poultry products, particularly chicken and turkey, were identified as the most common contributors. The study also noted that women and older men living in lower-income neighborhoods faced a disproportionately higher risk of these so-called “foodborne UTIs.”
The biological pathway behind this phenomenon is relatively straightforward. E. coli naturally resides in the intestines of animals and humans. During slaughtering and meat processing, these bacteria can contaminate raw meat if hygiene controls are insufficient. When contaminated meat is consumed undercooked, or when it is handled improperly in the kitchen, E. coli can be transferred to the human digestive system. Once established in the gut, certain strains can migrate to the urinary tract, where they may cause infection.
This risk is particularly pronounced in women due to anatomical factors, as the urethra is shorter and located closer to the anus, making bacterial transfer easier. Inadequate handwashing, cross-contamination of kitchen surfaces, and improper food storage further increase the likelihood of exposure. These findings highlight how everyday food preparation practices may influence infection risk in ways that are often overlooked.
Importantly, the study does not suggest that eating meat inevitably leads to UTIs. Rather, it underscores the importance of food safety as part of infection prevention. To reduce the risk of food-associated UTIs, experts recommend thoroughly cooking all meats, especially poultry, washing hands and kitchen surfaces after handling raw meat, and storing raw meat separately from ready-to-eat foods. Maintaining adequate hydration, urinating regularly, and practicing good personal hygiene can also help flush bacteria from the urinary tract.
While these measures cannot prevent all UTIs—since many infections still arise from non-food-related causes—they address an underrecognized source of exposure. As antibiotic resistance continues to rise globally, preventing infections at their source is becoming increasingly critical.
Overall, this research challenges conventional assumptions about UTIs and emphasizes the interconnectedness of food safety, socioeconomic conditions, and public health. Recognizing foodborne pathways of infection may help improve prevention strategies, particularly for vulnerable populations.
References
-
Liu, C. M., et al. (2023). Foodborne transmission of extraintestinal pathogenic Escherichia coli causing urinary tract infections. mBio, 14(4). PMID: 37363239.
-
Centers for Disease Control and Prevention (CDC). (2023). Urinary tract infection (UTI): Causes and prevention.
-
World Health Organization. (2022). Antimicrobial resistance and food safety. WHO Press.
-
European Food Safety Authority (EFSA). (2021). Risks associated with E. coli in food-producing animals and meat.
-
Harvard T.H. Chan School of Public Health. (2022). Food safety and bacterial contamination in meat products.
News in the same category
10 Foods To Eat for a Stronger Immune System
Top 10 Superfoods That Fight Proteinuria and Give Your Kidneys New Life – Starting in as Little as 7 Days
These 10 Foods May Support Cellular Health: What Research Suggests About Natural Antioxidant Power!
9 Urgent Warning Signs Your Body Is Sending – Ignoring These Could Be Dangerous!

Joint Pain? The Ultimate Guide to Rebuilding Your Joints Naturally: 8 Powerful Fruits You Must Know!
Over 60? 10 Early Dementia Warning Signs You Must NEVER Ignore (Catch Them Before It’s Too Late)

These are the consequences of wearing used…

What Happens to Your Body When You Eat Honey Every Day

What Happens to Your Body When You Eat Spinach Regularly

Daily Aloe Vera Juice Consumption and Improved Thyroid Function in Women with Subclinical Hashimoto’s Hypothyroidism

The Gut–Brain Connection: How Digestive Health Influences Mood and Mental Well-Being
A Complete Guide to Breast Cancer Prevention

What Can Happen When Women Lack Sexual Intimacy?

Tapering Antidepressants: What Strategy Works Best?
The Brainstem and Pain: New Research, New Understanding
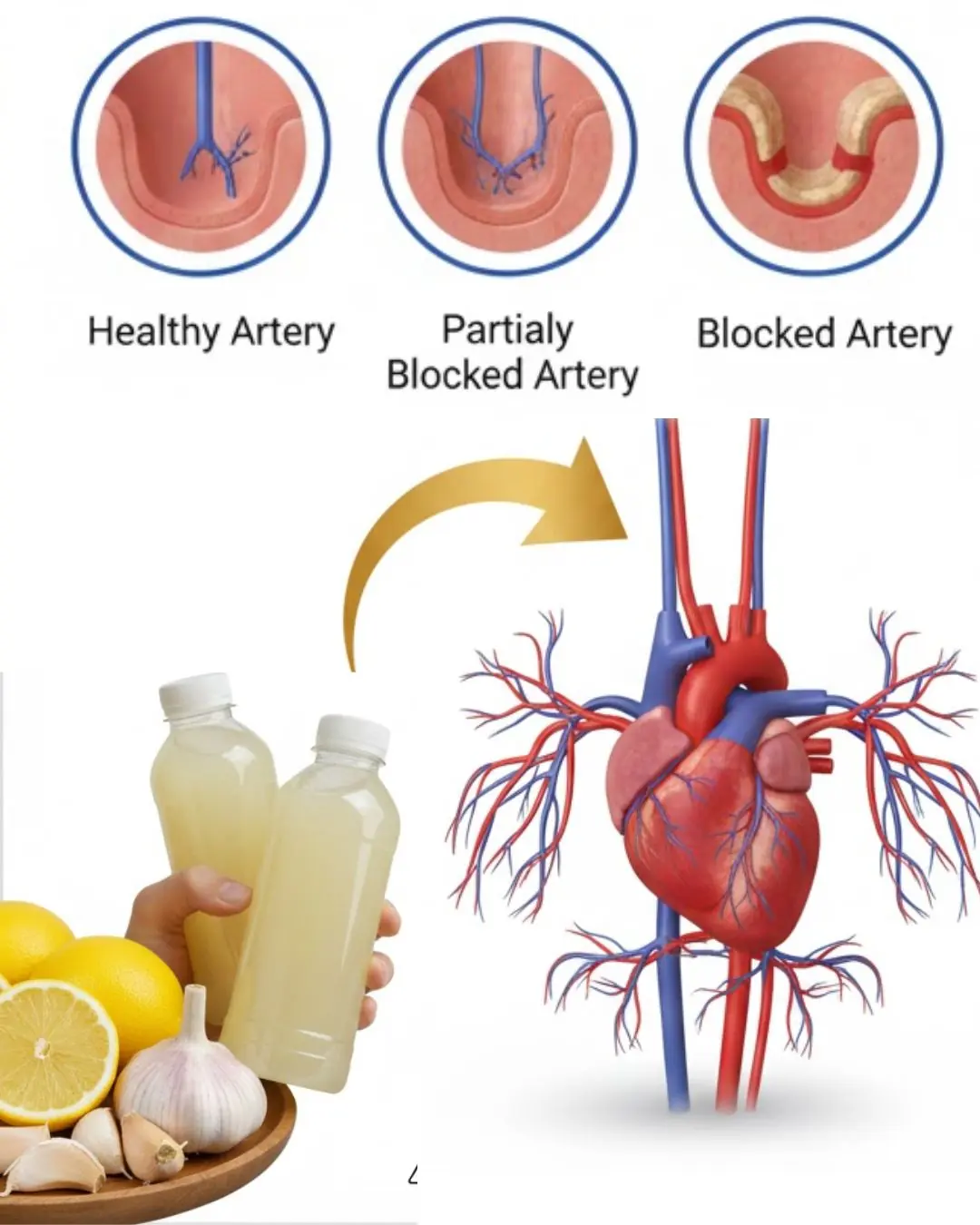
Could a Simple Bedtime Drink with Three Common Ingredients Support Your Heart Health?
Between Supplement Hype and Evidence: A Clinical Guide for Informed Use
Current Cardiac Screening Tools Miss Nearly Half of First Heart Attacks, Study Finds
News Post

Multiple people dead after explosion at Swiss Alps resort bar during New Year's celebrations

Most contagious disease in the world reported at two major US airports
What Causes a Shart?
10 Foods To Eat for a Stronger Immune System
Top 10 Superfoods That Fight Proteinuria and Give Your Kidneys New Life – Starting in as Little as 7 Days
These 10 Foods May Support Cellular Health: What Research Suggests About Natural Antioxidant Power!
9 Urgent Warning Signs Your Body Is Sending – Ignoring These Could Be Dangerous!

Joint Pain? The Ultimate Guide to Rebuilding Your Joints Naturally: 8 Powerful Fruits You Must Know!
Over 60? 10 Early Dementia Warning Signs You Must NEVER Ignore (Catch Them Before It’s Too Late)

Top 3 Nutrients Seniors Need to Stop Leg Cramps and Restore Strength: Reclaim Your Steady Steps Today!

12 Surprising Potential Benefits of Moringa Seeds You Might Not Hear About – But Research Suggests They’re Worth Knowing!

Discover the Timeless Secret of a 95-Year-Old Chinese Doctor: How He Stays Vibrant and Healthy

Urgent Advisory for New Smart Device Users: What You Need to Know About Privacy and Security

Urgent Warnings Over Smart Devices: What New Owners Need to Know About Privacy and Security

Therapy Dogs in the Courtroom: Bringing Compassion and Healing to the Justice System

Growing Organs from Stem Cells: A Breakthrough That Could Transform Organ Transplantation

California’s Solar Canals: A Dual Solution for Water Conservation and Clean Energy
Limberlost Place: How Canada Is Redefining Skyscrapers with Mass Timber Architecture
