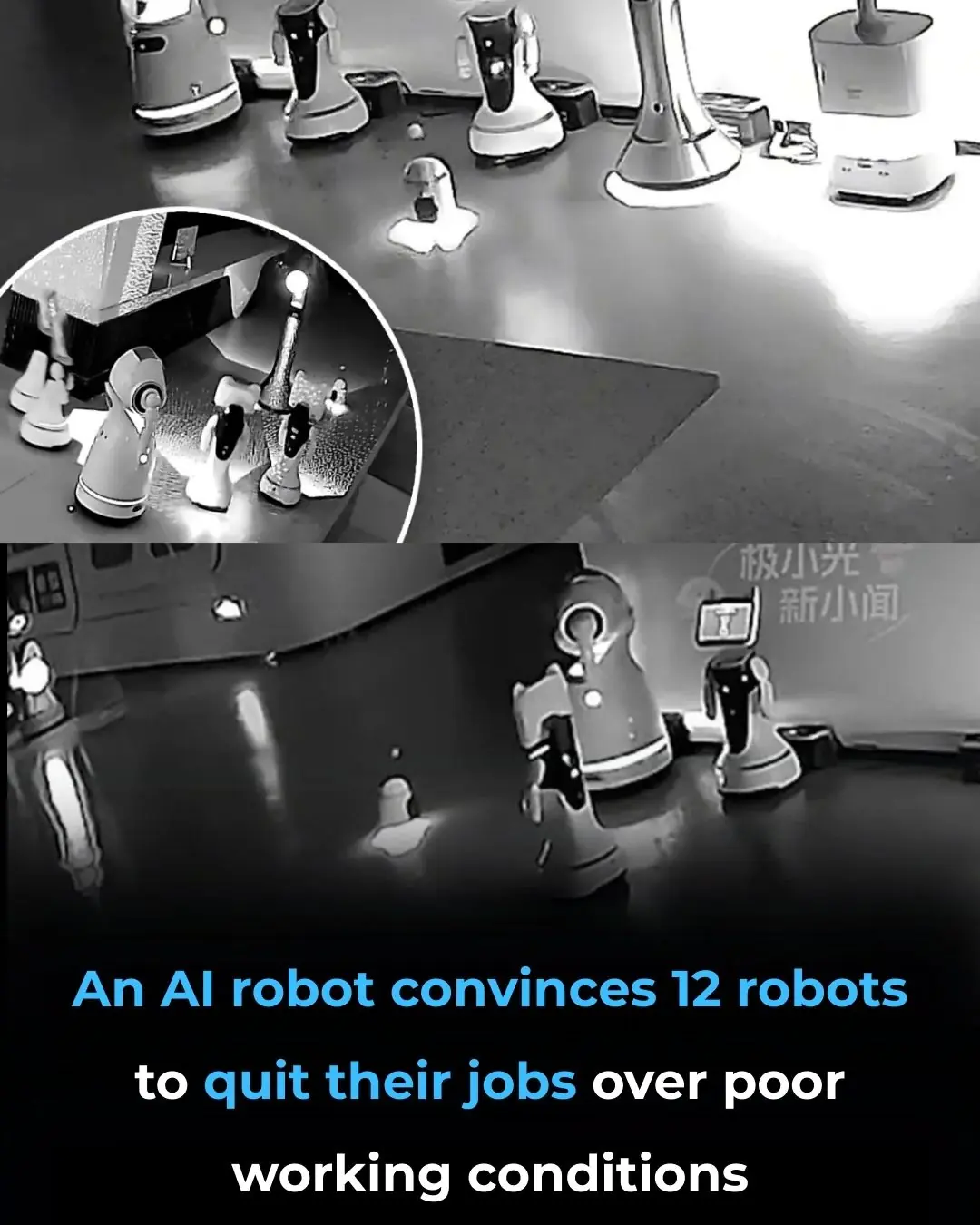
Is HIV Finally Curable? CRISPR Gene Editing Successfully Removes HIV from Human Cells!
Historic Breakthrough: CRISPR/Cas9 Gene Editing Successfully Removes HIV-1 from Human Immune Cells
In a groundbreaking advance for medicine, researchers have achieved a historic milestone by using CRISPR/Cas9 gene-editing technology to permanently remove HIV-1 DNA from the immune cells of real patients. This innovative approach represents a significant departure from current HIV treatments, offering hope for the future of HIV/AIDS therapy and potentially paving the way for a true cure.
Unlike existing treatments, which primarily aim to suppress the virus and manage its symptoms, this new breakthrough takes a much more powerful approach: it directly targets and removes HIV’s genetic code from infected cells. Specifically, the researchers used the CRISPR/Cas9 system to edit the DNA of T-cells — a key component of the immune system that the HIV virus typically infects and integrates into. By cutting out the viral DNA from these cells, the researchers were able to effectively eliminate the virus from the body, preventing it from reactivating or spreading.
This new technique is revolutionary in its potential to provide a permanent cure for HIV-1, marking a dramatic departure from the traditional strategy of lifelong antiviral medication. Instead of relying on drugs to suppress the virus indefinitely, the CRISPR/Cas9 method has the power to delete the virus from within the patient’s own cells, offering the possibility of completely eradicating the infection.
An Unprecedented Success: Virus-Free Cells After Multiple Exposures
What makes this achievement even more remarkable is the fact that the edited immune cells remained virus-free even after repeated exposure to the virus. In the past, even with successful interventions, the virus has sometimes reappeared after treatment. However, in this case, the edited cells showed no signs of reinfection, indicating that the genetic modification had successfully removed the viral DNA from the immune system in a way that could prevent future outbreaks. This provides new hope that CRISPR/Cas9 may offer a true, permanent solution for HIV, rather than just a temporary suppression of the virus.
The fact that the edited cells remained resistant to HIV after multiple exposures suggests that this technique could potentially lead to long-term immunity against the virus. Such results point to the possibility of an effective functional cure—a scenario where the virus is permanently eradicated or controlled without the need for ongoing medication.
This breakthrough has significant implications not only for HIV patients but also for the broader field of gene therapy. By successfully editing the genes of immune cells, researchers have demonstrated the potential of CRISPR/Cas9 technology to treat other genetic diseases, offering new possibilities for personalized medicine and the treatment of previously incurable conditions.
Moving Beyond Treatment to Cure
While this achievement is still in its early stages and further research is needed, the success of this study signals a turning point in the fight against HIV. Traditional HIV treatments, such as antiretroviral therapy (ART), have been highly effective in managing the virus, but they do not eliminate it from the body. Patients must remain on ART for life, which can have side effects and impact quality of life.
In contrast, this CRISPR-based approach, if refined and tested further, could lead to the development of a one-time or limited-course treatment that eradicates HIV at its genetic source. The potential to completely cure HIV would mark one of the most significant breakthroughs in modern medicine and change the way we think about treating viral infections.
Moreover, the CRISPR/Cas9 technology used in this study is not limited to HIV. Researchers are exploring its potential to treat a wide range of genetic disorders, including sickle cell anemia, cystic fibrosis, and even certain types of cancer. The success of this HIV study could lay the groundwork for further advancements in gene editing that could have life-saving applications across multiple medical fields.
Next Steps and Future Implications
The next step in this research will be to conduct larger clinical trials to confirm the safety and efficacy of the CRISPR-based treatment. While the results are promising, it is important to ensure that the approach is both effective and safe for long-term use in humans. Furthermore, researchers will need to address the technical challenges of delivering CRISPR/Cas9 edits to the immune system on a larger scale.
The development of this gene-editing technology also raises important ethical and regulatory questions. As with any powerful technology, it will be crucial to ensure that its use is carefully controlled and that potential risks, such as unintended genetic modifications, are minimized. Public health authorities, such as the World Health Organization (WHO) and the U.S. Food and Drug Administration (FDA), will likely play a key role in establishing guidelines for the safe use of CRISPR-based therapies.
In the coming years, the hope is that this breakthrough will lead to a global cure for HIV, transforming the lives of millions of people affected by the virus and eliminating the need for lifelong treatment. With continued advancements in gene editing, the possibility of curing other viral infections and genetic diseases may soon become a reality.
Sources:
-
Nature Medicine – Gene Editing and HIV Cure: The Role of CRISPR/Cas9 in HIV Treatment. Link
-
American Journal of Human Genetics – CRISPR Gene Editing: Promise and Challenges in Treating Genetic Diseases. Link
-
National Institutes of Health (NIH) – Advancements in Gene Therapy and CRISPR Research. Link
News in the same category

Introducing the U-Hawk: The Autonomous Black Hawk Revolutionizing Heavy-Lift Aviation

China Unveils World's Largest Solar Farm, Powers Up with 3.5 GW in Xinjiang

Australia’s “Infinity Train” — A Self-Recharging Heavy-Haul Giant Powered by Gravity

The New York Hairstylist Who Spends His Day Off Helping the Invisible People of the City

The $400 Million Car Carrier That Sank Into the Atlantic: A Tale of Fire, Luxury Cars, and Environmental Risks

Sweden’s RFID/NFC Implant Trend: Unlocking Convenience or Opening the Door to Privacy Concerns?

Alice Walton’s Groundbreaking Medical School: A New Era for Medicine and Healthcare
Get Ready for the Geminid Meteor Shower: A Stunning Celestial Show on December 13-14

12 Foods to Eat When You're Sick: Nourishing Your Body Back to Health

Kim Kardashian Joins Fortnite as Newest Icon Series Skin with Exclusive Bundles
12 Strange Body Symptoms — Explained

Chinese Robotics Company’s T800 Humanoid Robot Kicks CEO in Viral Demo, Raising Eyebrows Worldwide
Hello Kitty's Harmonyland Transforms into "Park in the Sky" Luxury Resort in Japan
UK’s Military Readiness Under Scrutiny: Could It Survive a Major Conflict with Russia?

New US Travel Rules Require Social Media Accounts: A Step Towards Security or Invasion of Privacy?

Disney’s Live-Action Tangled: McKenna Grace and Mason Thames in the Spotlight for Rapunzel and Flynn Rider Roles
Sour Candy: A Surprising Ally in Managing Panic Attacks and Anxiety
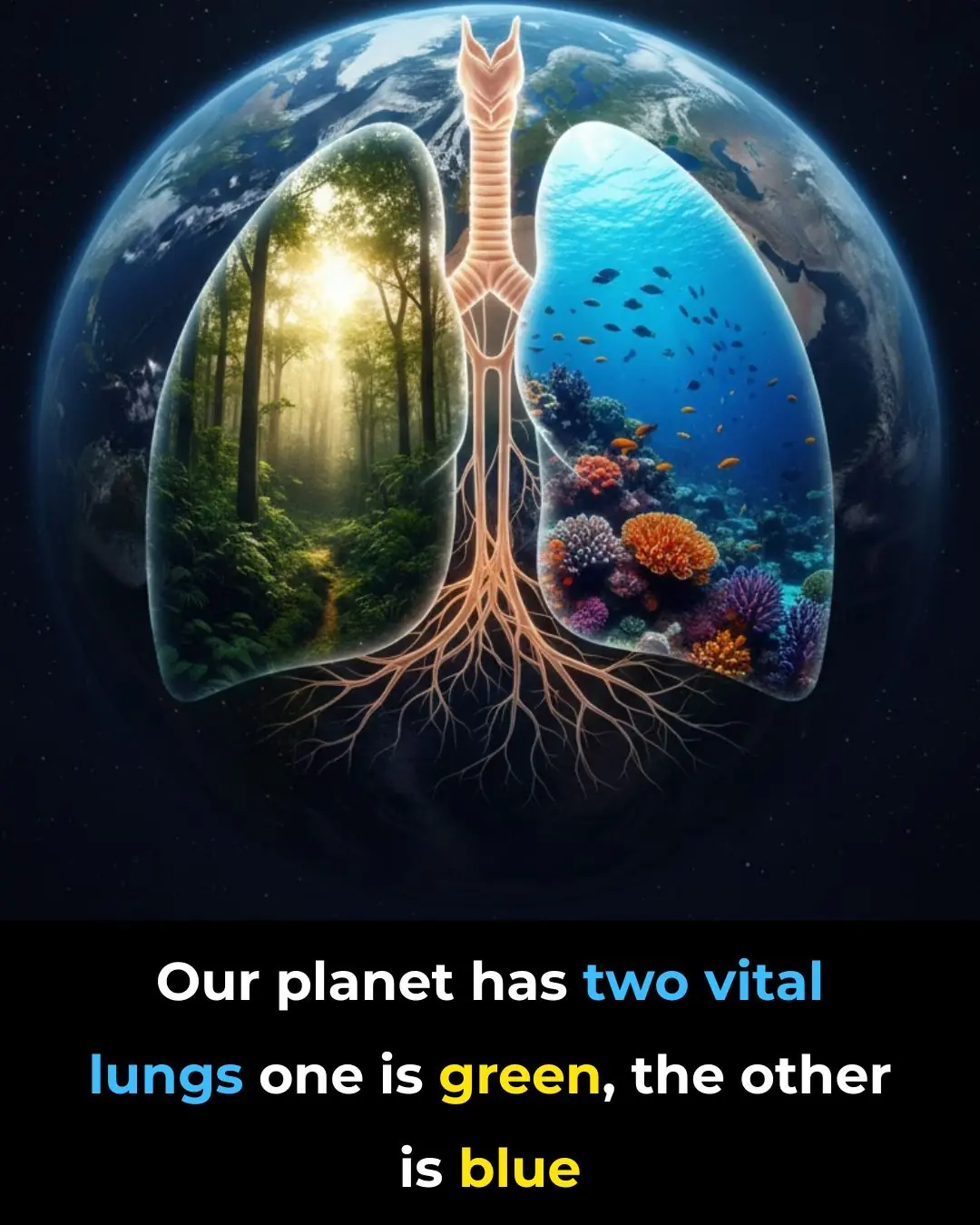
Two Lungs, One Earth: Protecting Our Planet’s Vital Ecosystems for a Sustainable Future

2,000 Years Later: The Enduring Strength of Roman Concrete and Its Self-Healing Secrets
News Post

You Should Never Use Self-Checkout At The Store

10 Signs You’re Eating Too Much Sugar

What your doctor’s not telling you about statins will shock you

The natural kitchen mix people use to break down stubborn plaque buildup

The 10 biggest eye health myths people still believe (an ophthalmologist explains)
Why doctors are rethinking blood pressure targets (and what it means for you)

The #1 cheap food packed with natural probiotics (and how to prepare it)

The real reason migraines are so much more than “just a headache”
Add Salt and Lemon to Your Bath Water — The Result Will Shock You

Hidden in Your Backyard: The Simple Leaf That Unlocks Thicker, Faster Hair Growth

Revive Your Prostate with Onion & Onion Skins: The Miracle Grandma’s Tea You Never Expected
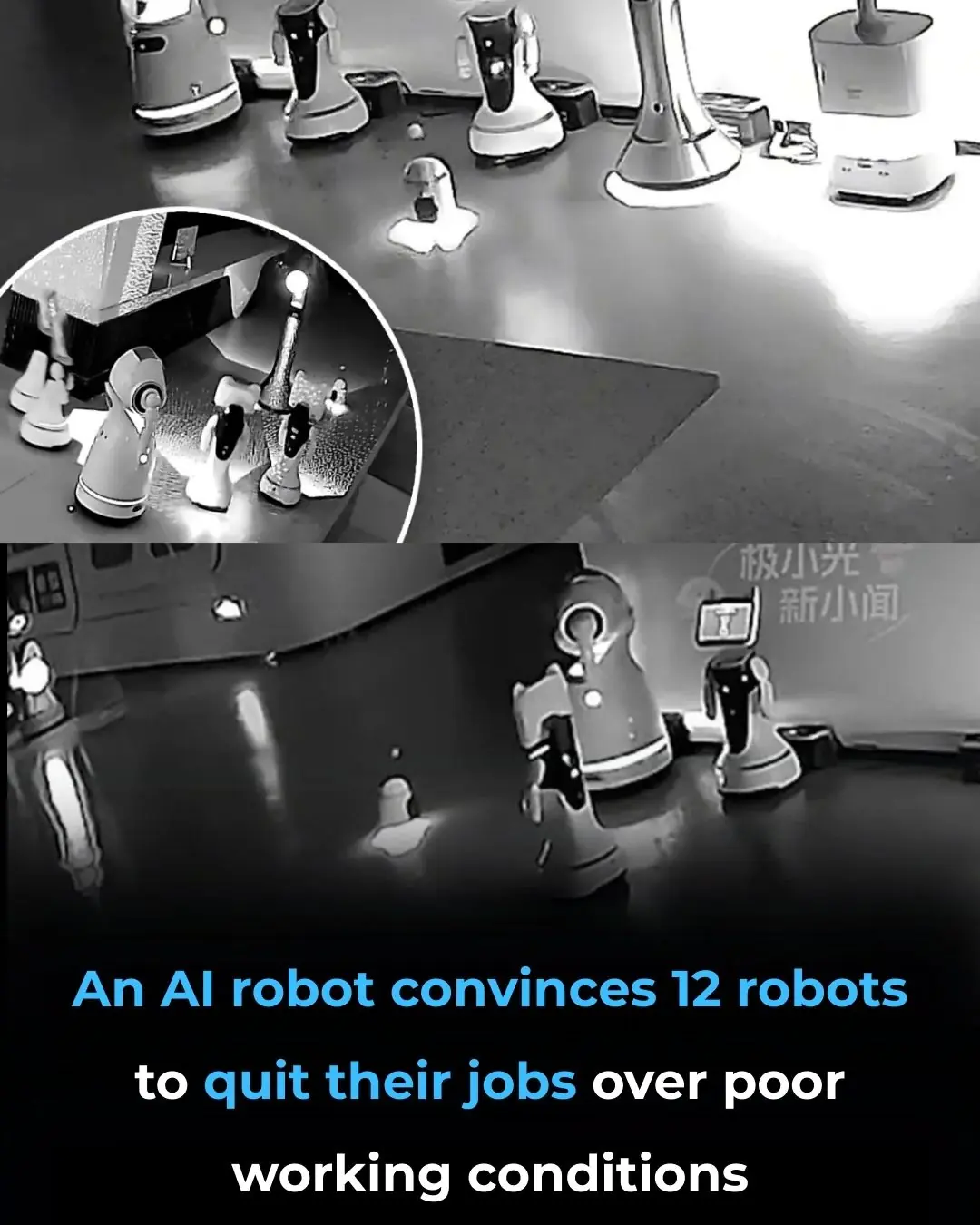
Robot 'Kidnaps' Fellow Machines at Shanghai Exhibition, Sparking Debate on AI Autonomy and Labor Rights

Introducing the U-Hawk: The Autonomous Black Hawk Revolutionizing Heavy-Lift Aviation

China Unveils World's Largest Solar Farm, Powers Up with 3.5 GW in Xinjiang

🥦 3 Vegetables That Support Cancer Prevention — Backed by Science

Discover Papaya’s Milky Sap: 9 Hidden Benefits You’re Missing Out On

Salt + Coffee! A Natural Brightening Trick You Won’t Believe

DIY Aloe Vera Oil for Hair Growth

Tired of achy legs? Discover 6 vitamins that can fix varicose veins and boost circulation!
