
Miracle Cure? Woman’s Tumor Practically Vanishes in Just 5 Days Thanks to New Cancer Treatment!
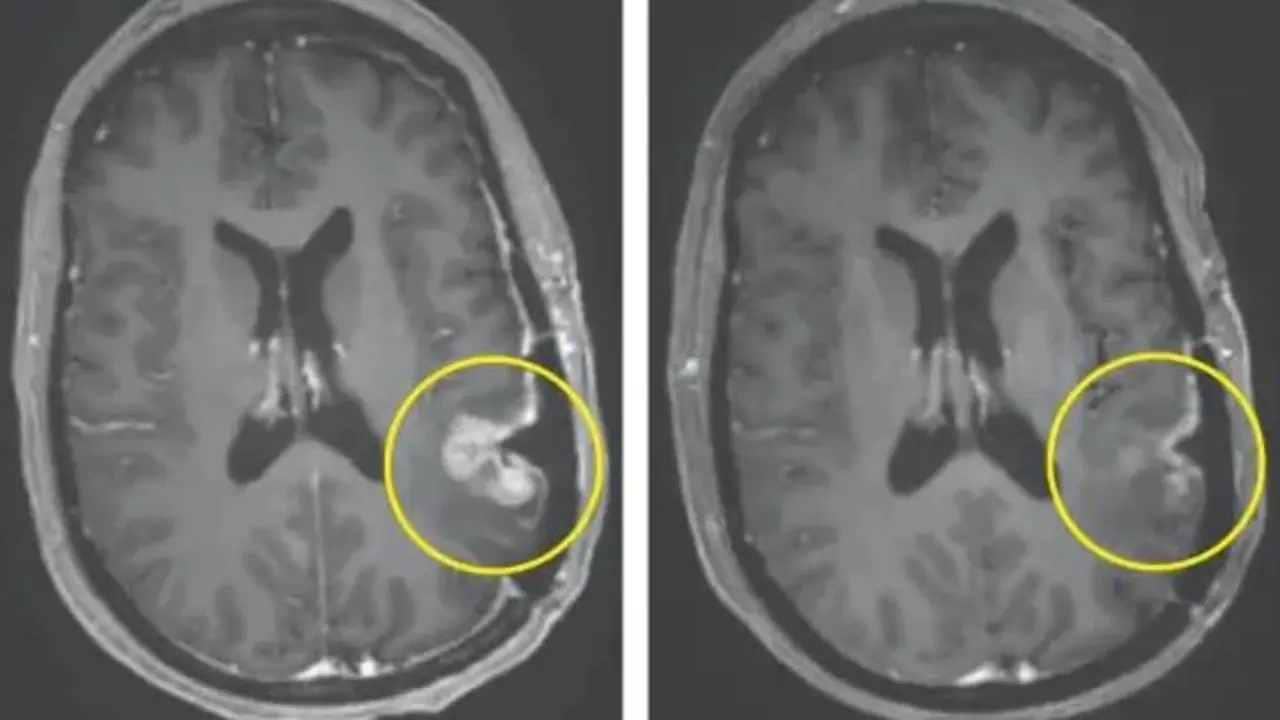
In a stunning medical advancement that could revolutionize how the world treats one of the deadliest forms of brain cancer, a new trial has revealed that a personalized immunotherapy technique caused a woman’s aggressive brain tumor to nearly vanish in just five days. The clinical success, reported in March 2024, marks a significant milestone in the decades-long fight against glioblastoma, a notoriously aggressive and largely incurable brain cancer.
This breakthrough comes from a team of pioneering researchers and surgeons at Mass General Brigham, who have developed a new variant of CAR-T cell therapy, adapted specifically to target solid tumors like glioblastoma - a feat once thought nearly impossible.
What Is CAR-T Therapy and Why Is This Different?
CAR-T (Chimeric Antigen Receptor T-cell) therapy is an advanced form of immunotherapy that involves harvesting a patient’s own T-cells - the immune system’s natural defenders - and genetically reprogramming them in a lab to recognize and attack cancer cells. Once re-engineered, these T-cells are infused back into the patient’s bloodstream, where they begin hunting down cancerous cells with high precision.
This technique has previously shown remarkable success in treating blood cancers such as leukemia and lymphoma. However, solid tumors like glioblastoma have proven far more elusive.
“The CAR-T platform has revolutionized how we think about treating patients with cancer, but solid tumors like glioblastoma have remained challenging to treat because not all cancer cells are exactly alike and cells within the tumor vary,” explained Dr. Bryan Choi, MD, PhD, a neurosurgeon and associate director of the Center for Brain Tumor Immunology and Immunotherapy at the Mass General Cancer Center.
To overcome this barrier, the Mass General Brigham team enhanced the traditional CAR-T therapy by adding specific antibodies to target a broader spectrum of cancer cell variants. This hybridized approach allows the immune cells to better recognize and destroy diverse types of glioblastoma cells.

The Study That Shocked the Medical World
The clinical trial, recently published in The New England Journal of Medicine, involved just three patients - all of whom were battling recurrent glioblastoma, a cancer that has a median survival rate of only 15 months even with treatment. Despite the small size of the study, the results were nothing short of astonishing.
One patient exhibited an 18.5% reduction in tumor size just two days after receiving the CAR-T infusion, followed by a 60.7% reduction by day 69. Another patient saw their tumor “regress rapidly,” as described by the research team.
But perhaps the most remarkable outcome came from the third patient. According to MRI scans, this individual experienced a “near-complete tumor regression” within just five days of receiving a single CAR-T infusion.
These are not just small improvements. In the world of glioblastoma treatment - where tumors typically grow back even after surgery, chemotherapy, and radiation - such a rapid and dramatic response is unprecedented.

Why Glioblastoma Has Been So Difficult to Treat
Glioblastoma is often described as one of the most aggressive and complex forms of cancer. It infiltrates healthy brain tissue with microscopic tentacles, making it nearly impossible to remove completely with surgery. Traditional therapies like radiation and chemotherapy can slow its progress but rarely succeed in eliminating the tumor entirely.
Part of what makes glioblastoma so deadly is its high level of heterogeneity - meaning the cancer cells within a single tumor can differ greatly from one another. That makes it extremely difficult to develop a single drug or treatment that works uniformly.
As Dr. Choi put it, “Our approach combines two forms of therapy, allowing us to treat glioblastoma in a broader, potentially more effective way.”
The Promise of Cell Therapy for “Incurable” Conditions
This innovative CAR-T treatment offers a beacon of hope in a field that has seen little progress in recent decades. Mass General Brigham emphasized that studies like this one “show the promise of cell therapy for treating incurable conditions,” giving both patients and oncologists new reasons for optimism.
While CAR-T therapy has traditionally been reserved for blood cancers, this breakthrough suggests that its application could be extended to other solid tumors - including those affecting the brain, pancreas, or lungs.
“These results are exciting, but they are also just the beginning,” said Marcela Maus, MD, PhD, director of the Cellular Immunotherapy Program. “They tell us that we are on the right track in pursuing a therapy that has the potential to change the outlook for this intractable disease. We haven’t cured patients yet, but that is our audacious goal.”
A Word of Caution: It’s Still Early Days
As with any early-phase trial, researchers caution that while the results are promising, this is not yet a cure. The study involved only three patients, and the long-term effectiveness and safety of the therapy remain under investigation.
“We report a dramatic and rapid response in these three patients. Our work to date shows signs that we are making progress, but there is more to do,” said Elizabeth Gerstner, MD, a neuro-oncologist and study co-author from Massachusetts General Hospital.
Larger clinical trials are now being planned to determine how widely applicable the treatment is, what side effects may emerge over time, and whether it can be safely scaled up.
The Bigger Picture: Hope on the Horizon
This development comes at a time when global cancer cases are on the rise, and brain cancers remain among the most challenging to treat. According to the World Health Organization, glioblastoma accounts for more than half of all malignant brain tumors in adults, with survival rates stubbornly low despite advances in medical science.
Yet the latest findings from Mass General Brigham demonstrate what’s possible when personalized medicine and cutting-edge immunotherapy intersect. The ability to program a patient’s immune system to selectively destroy cancer cells, even in the brain, represents a profound leap forward.
And it's not just about shrinking tumors.
CAR-T therapy could offer a long-term solution, one where the immune system continues to monitor and fight off cancer cells even after the initial treatment is complete - a concept known as immunological memory.
Looking Ahead: What This Means for Patients
If future trials confirm the success of this hybrid CAR-T treatment, glioblastoma patients may finally have access to a therapy that does more than slow the disease - it might actually reverse it.
For now, the treatment is still experimental and available only through clinical trials. But the team at Mass General Brigham is pushing ahead, driven by what they believe is a historic opportunity.
“Our goal is to make this treatment widely accessible and, ultimately, to cure a disease that has taken too many lives,” said Dr. Maus.
As science continues to evolve, and as trials expand to more patients and hospitals worldwide, it may only be a matter of time before immunotherapy becomes the new standard in treating not just blood cancers, but the most stubborn solid tumors as well.
News in the same category


AI is willing to kill humans to avoid shutdown as chilling new report identifies 'malicious' behaviour

Horrifying simulation details exactly how cancer develops in the body

Elon Musk slammed for posting creepy video of 'most dangerous invention to ever exist'

World’s Rarest Blood Type Discovered—Only One Woman Has It
The woman with Gwada negative blood may not be famous, but her existence has already made an indelible mark on medical science.
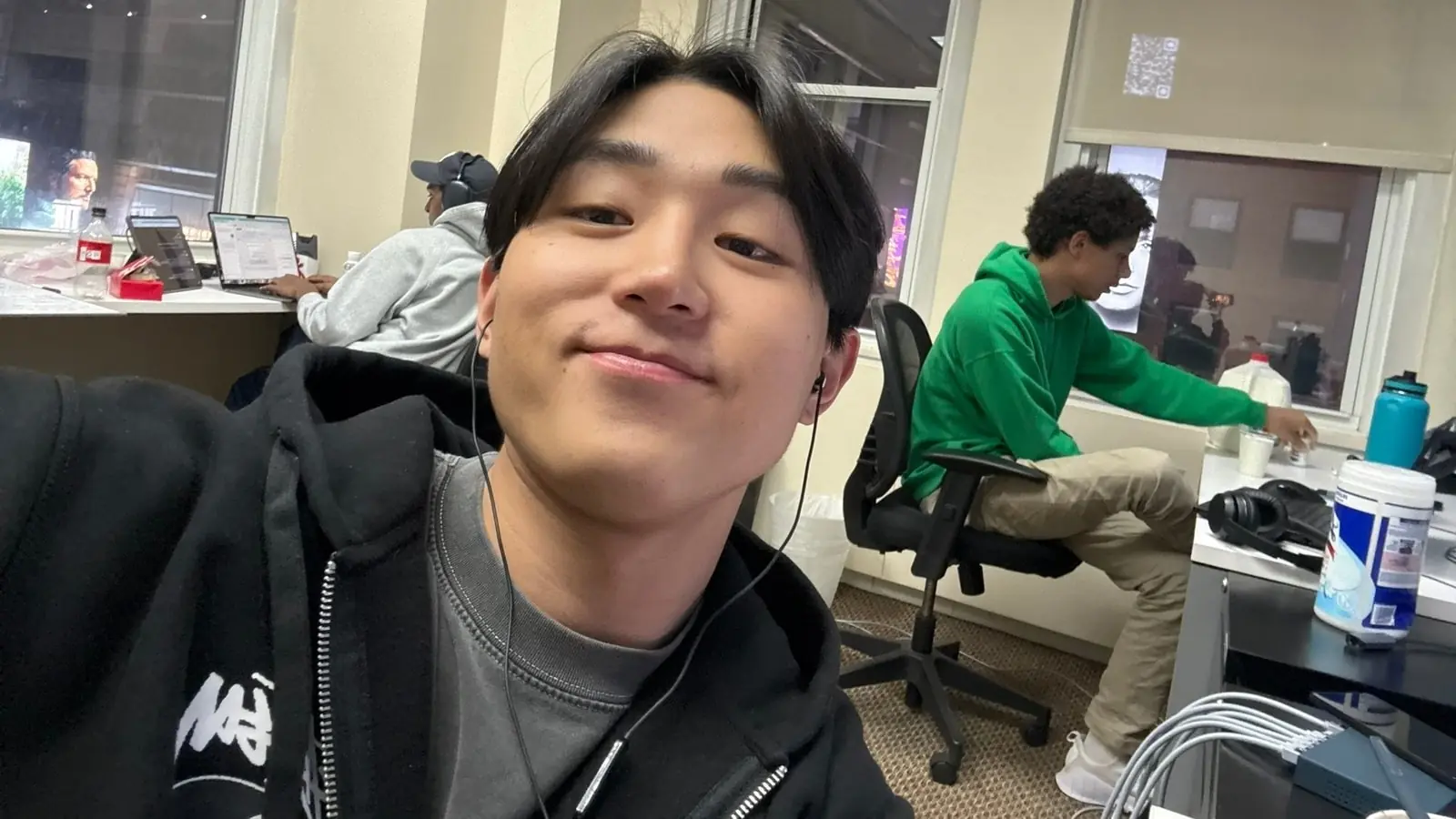
Columbia Student Suspended After Creating AI That Helps You Cheat Your Way to a Six-Figure Job!
Despite being out of school, he remains optimistic about the future. With growing venture capital support and rising user demand, Cluely may be on track to become a key player in the next wave of controversial tech startups.

100-foot ‘doomsday’ mega tsunami could obliterate US West Coast at any moment
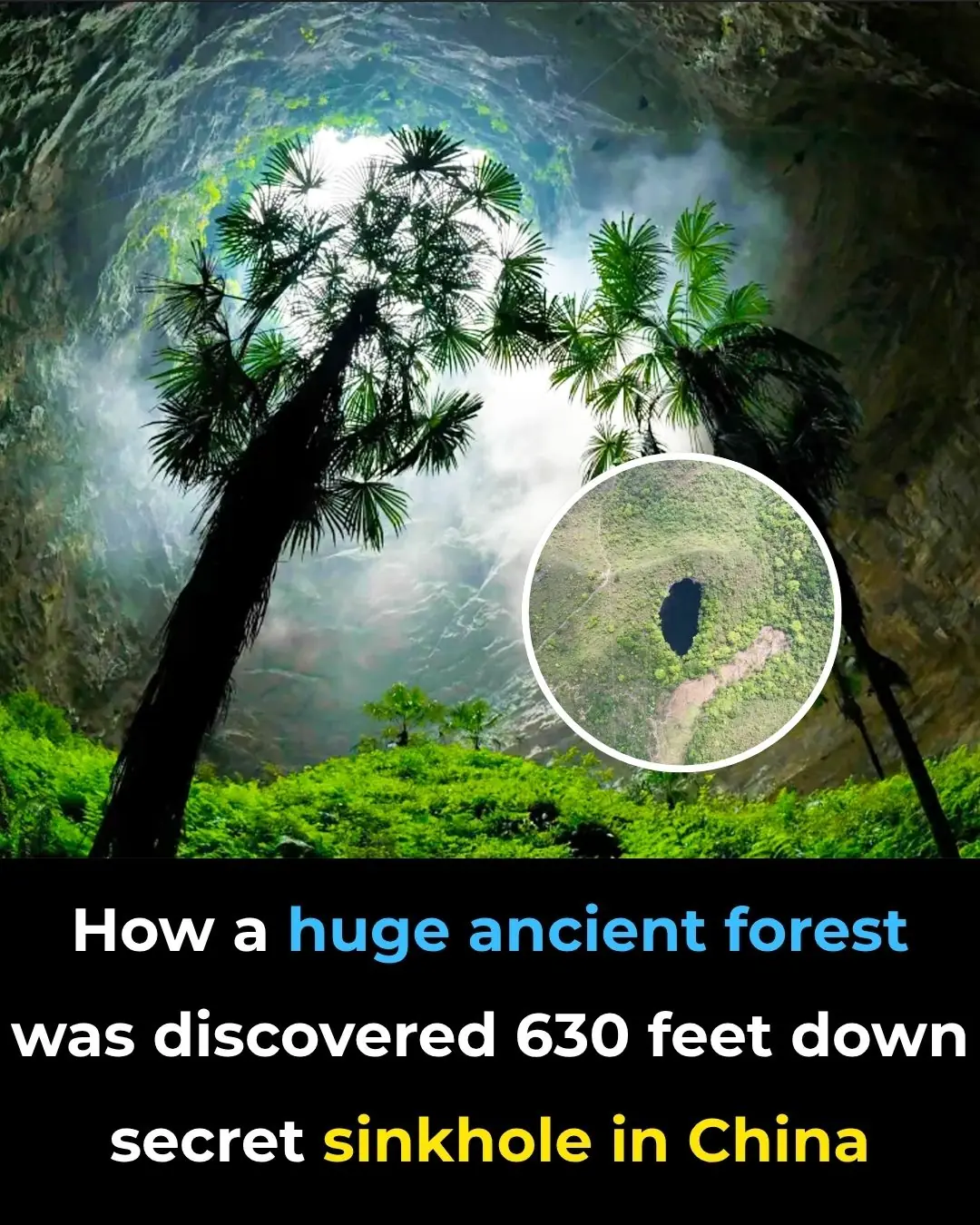
How a huge ancient forest was discovered 630 feet down secret sinkhole in China
100 Million Americans at Risk from Brain-Eating Parasite, Experts Warn
By understanding this parasite, improving detection, and emphasizing prevention, we can mitigate these risks

Woman who "died for 17 minutes" shares unimaginable reality of what she saw when her heart stopped beating
Victoria’s story transcends the ordinary—she experienced clinical death, returned with clarity, and then learned of a rare genetic disease that nearly killed her again. Yet today, she thrives.

Nasa Tracks Plane-Sized Asteroid Speeding Toward Earth At 47,000 Mph

Oscar Mayer Mansion Restored To Gilded Age Glory After $1.5M Renovation
Secret CIA Documents Declare That The Ark Of The Covenant Is Real, And Its Location Is Known

The Mystery Behind The Blood Falls In Antarctica
James Webb Telescope Reveals Surprising Update On An Asteroid That Could Make Everyone On Earth A Billionaire

Archaeologists Think They Discovered The Real Noah’s Ark

Scientists Develop Smart Shoes That Help Blind People Avoid Obstacles. Here’s How They Work
Sh0cking Study: Scientists Find Cocaine in Every Shrimp Sample from National Waters
his research reveals a world where human habits, medications, and vices seep silently into ecosystems, transforming the lives of creatures that never consented to the party.

Meet the Bug You Should Not Kill: The Misunderstood House Centipede
The house centipede might never win a beauty contest, but it deserves far more appreciation than it gets.
News Post

Earth may witness a once-in-5,000-year event on the moon and it's coming sooner than you think

AI is willing to kill humans to avoid shutdown as chilling new report identifies 'malicious' behaviour

Horrifying simulation details exactly how cancer develops in the body

Elon Musk slammed for posting creepy video of 'most dangerous invention to ever exist'

Indiana Boy, 8, Dies Hours After Contracting Rare Brain Infection At School

World-First Gene Therapy Restores Sight to Boy Born Blind

World’s Rarest Blood Type Discovered—Only One Woman Has It
The woman with Gwada negative blood may not be famous, but her existence has already made an indelible mark on medical science.

A Warning About The ‘Worst Thing’ That People Should Never Do When Awakening in the Night
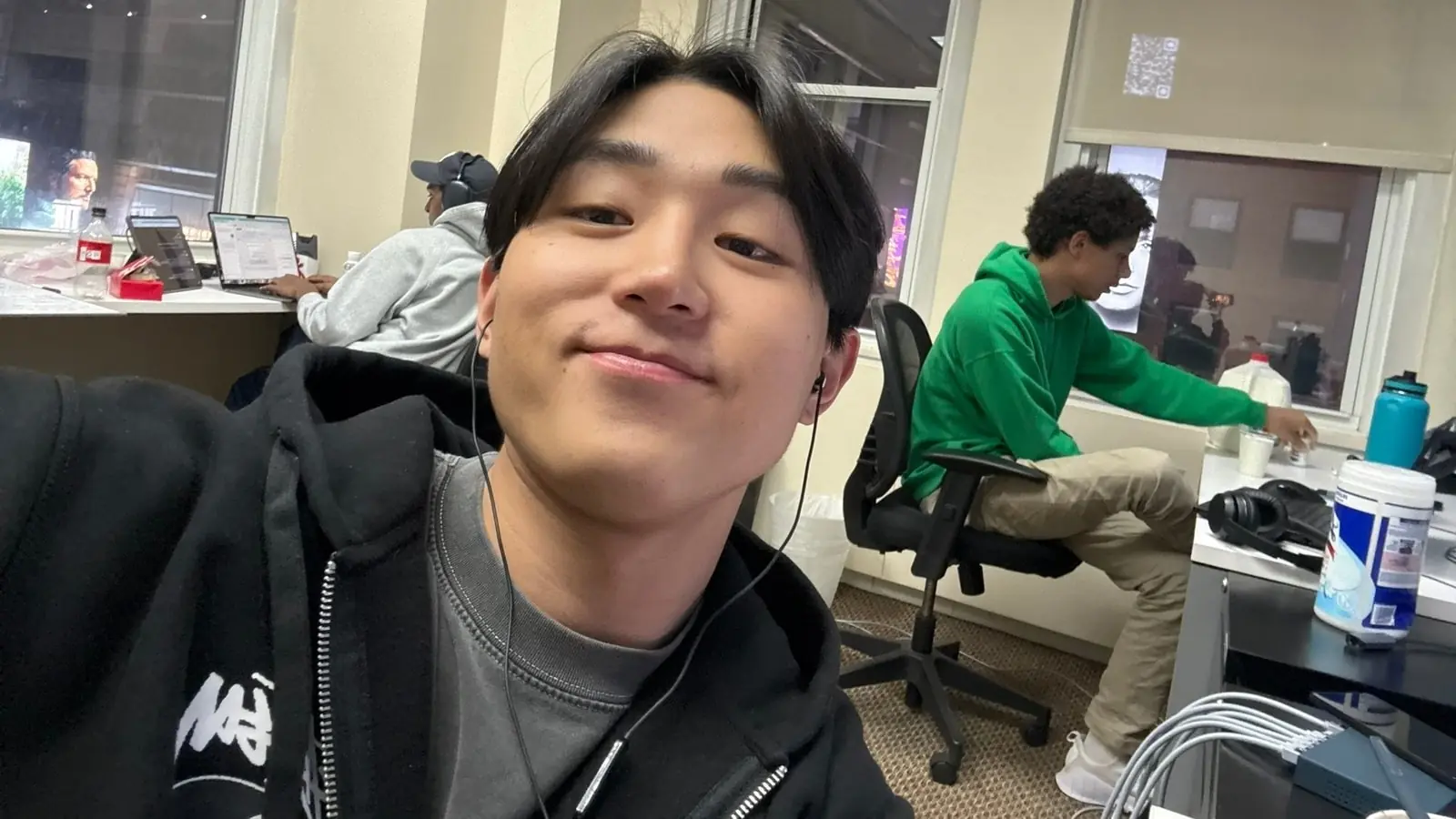
Columbia Student Suspended After Creating AI That Helps You Cheat Your Way to a Six-Figure Job!
Despite being out of school, he remains optimistic about the future. With growing venture capital support and rising user demand, Cluely may be on track to become a key player in the next wave of controversial tech startups.

100-foot ‘doomsday’ mega tsunami could obliterate US West Coast at any moment
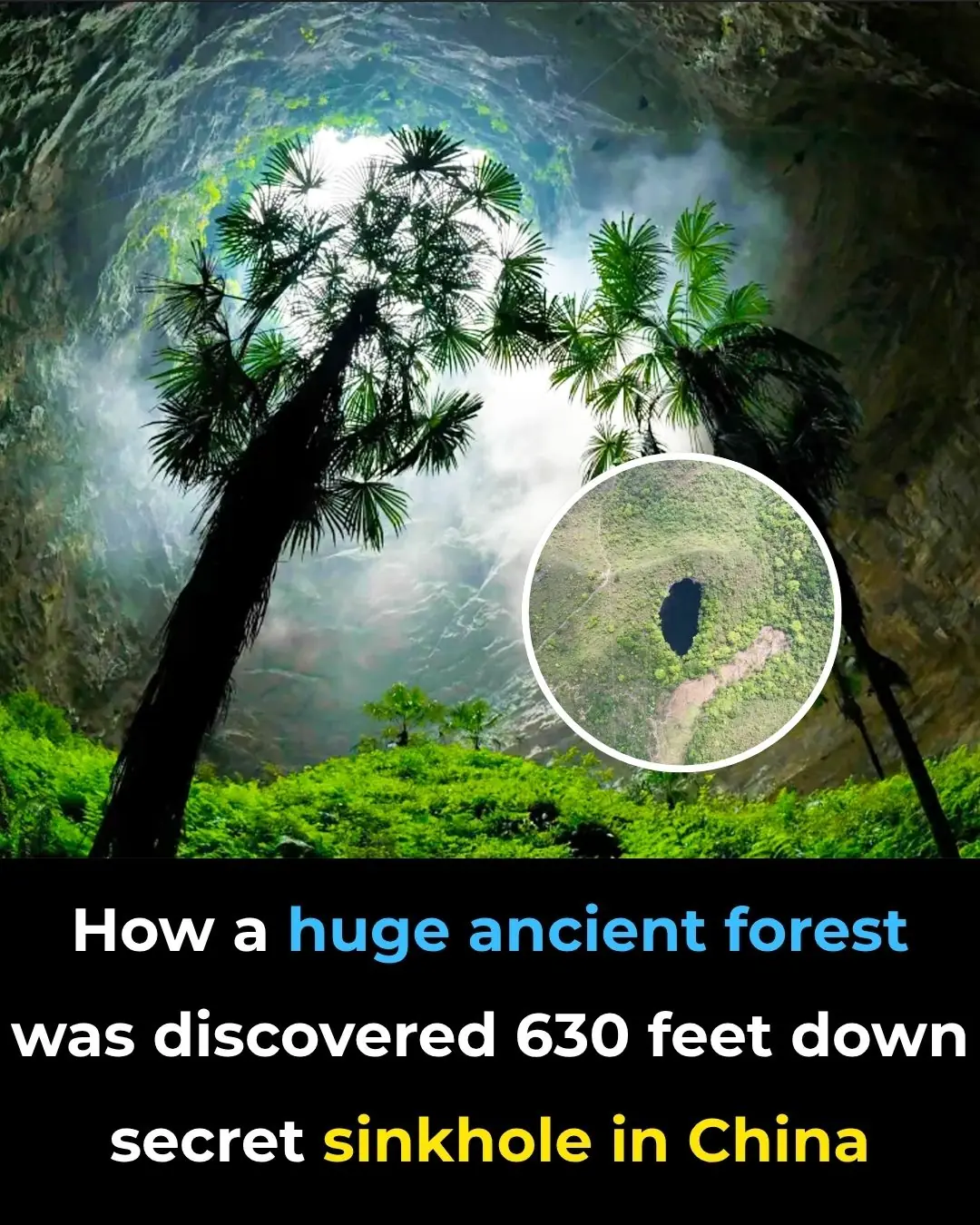
How a huge ancient forest was discovered 630 feet down secret sinkhole in China
100 Million Americans at Risk from Brain-Eating Parasite, Experts Warn
By understanding this parasite, improving detection, and emphasizing prevention, we can mitigate these risks

Woman who "died for 17 minutes" shares unimaginable reality of what she saw when her heart stopped beating
Victoria’s story transcends the ordinary—she experienced clinical death, returned with clarity, and then learned of a rare genetic disease that nearly killed her again. Yet today, she thrives.

A Test of Love and Money: How One Man’s Hidden Life Led to a Surprising Proposal
Nina thought she knew everything about Andrei, but when she discovered his secretive behavior, doubts began to creep in. After a series of expensive surprises and mysterious encounters, Nina’s curiosity led her to uncover the truth about Andrei’s doub

What She Heard When She Came Home Early Left Her Stunned: A Secret Conversation Between Husband and Mother
Diana always felt she had been exceptionally fortunate. Raised in a family of entrepreneurs, she had everything she needed and more.

Boss Crosses the Line: Waitress Forced to Strip in Front of Everyone to Prove She’s Not a Thi3f
Mikhail woke up suddenly, drenched in cold sweat. That same cursed dream again. It had once been rare, but now it was a constant presence in his nights.

I Left Lena, Thinking She Would Always Be the Same – But When I Saw Her Again, I Was Overcome with Envy
After years of frustration and emotional turmoil, Oleg finds himself facing a harsh reality: the woman he once loved has moved on, flourishing without him. When they unexpectedly cross paths again, Oleg is confronted with the woman he never expected to se
I Gave My All to Care for My Sick Mother, But Her Will Left Me With Nothing
I had been there for my mother every step of the way, caring for her through her final days, giving up everything to ensure she wasn’t alone. Yet, when the will was read, I found myself with nothing. The betrayal stung, but the truth behind her decision
I Discovered a Hidden Document in the Trash – My Husband and MIL Made a Huge Deal Behind My Back While I Was Fighting for My Life
When Maria overhears a mysterious conversation between her husband and mother-in-law, she discovers a torn document that leads to an unexpected revelation. Struggling with cancer and fearing betrayal, Maria is about to uncover something that will change e

My Stepmother Kicked Me Out Right After My Father Died – The Next Morning, SUVs Started Appearing at Her Door
When Ellie loses her father, she expects to face grief, not betrayal. Kicked out of her childhood home by a woman who never truly accepted her, Ellie makes one desperate call. But what she gets on the other end isn’t sympathy—it's a revelation. The ne