Regenerative Medicine Milestone: Stem-Cell Trial Restores Motor Function in Paralyzed Patients
A groundbreaking clinical trial in Japan has reported encouraging early results: a man who was paralyzed following a severe spinal cord injury has regained the ability to stand independently—and is now undergoing rehabilitation with the goal of walking—after receiving an experimental stem-cell–based therapy. This development represents one of the most promising advances to date in the field of regenerative medicine for spinal cord injuries, a condition for which treatment options have traditionally been extremely limited.
The study, led by Professor Hideyuki Okano at Keio University School of Medicine in Tokyo, involves injecting neural stem cells derived from induced pluripotent stem cells (iPSCs) directly into the damaged area of the spinal cord. iPSCs are adult cells that have been reprogrammed back into an embryonic-like state, enabling them to differentiate into various cell types, including neural tissue. This technique has attracted substantial attention over the past decade, particularly since its invention earned Shinya Yamanaka the 2012 Nobel Prize in Physiology or Medicine.
(Sources: Nature; Keio University School of Medicine; Nobel Prize official site.)
In the trial’s initial cohort of four participants, two individuals showed significant functional recovery. One patient regained sufficient lower-limb motor control to stand without support—a remarkable milestone given the limited regenerative capacity of the adult spinal cord. Another patient recovered partial movement in both arms and legs, allowing increased independence in daily tasks. The remaining two participants experienced only minimal improvement, though importantly, no severe adverse events were observed during a one-year follow-up period.
(Sources: Nature News, 2024; The Japan Times.)
The procedure involves surgically delivering more than two million iPSC-derived neural stem cells into the injured segment of the spinal cord. To reduce the risk of immune rejection, patients received six months of immunosuppressive therapy following transplantation. The primary focus of this early-phase trial is safety rather than efficacy, and the researchers emphasize that the observed improvements, while encouraging, cannot yet be conclusively attributed to the stem-cell treatment alone. Some degree of natural recovery is known to occur in certain spinal cord injuries, particularly within the first year after trauma.
(Sources: Cell Stem Cell; International Spinal Cord Society.)
Nevertheless, the significance of these findings should not be understated. Conventional treatments for spinal cord injury—such as decompression surgery, physical rehabilitation, and pharmacological interventions—rarely restore lost motor or sensory function once the initial damage has stabilized. The possibility that transplanted neural stem cells may promote regeneration, form new neuronal connections, or modulate inflammation represents a major conceptual shift in what might be achievable for patients with paralysis.
(Sources: Mayo Clinic; National Institutes of Health.)
The use of iPSCs also offers ethical and immunological advantages over embryonic stem cells, as they can be generated from adult tissues and potentially matched to individual patients to reduce immune complications. Japan has been at the forefront of iPSC-based therapies, with national regulatory frameworks that allow carefully supervised but accelerated translation of stem-cell research into clinical trials.
(Sources: RIKEN Center for Developmental Biology; Japan Agency for Medical Research and Development.)
Experts caution that despite the breakthrough, the research is still in its early stages. Larger clinical trials will be required to determine how effective the therapy truly is, how broadly it can be applied to different types of spinal injuries, and whether the improvements will persist over years rather than months. Long-term risks—including abnormal cell growth or delayed immune reactions—must also be carefully monitored.
In summary, while this development marks a major advancement in regenerative medicine and brings genuine hope to individuals living with paralysis, it remains an early but promising step. The patient’s regained ability to stand signals the potential of iPSC-derived neural stem-cell therapy, yet many questions remain regarding durability, safety, and scalability. As further data emerges, the world will be watching closely to see whether this pioneering treatment can fulfill its transformative promise.
News in the same category
A Dual Climate Solution: Solar Panels Over Canals Could Save Billions of Gallons of Water

From Crow to Cleaner: How Feathered Geniuses Are Fighting Litter in Spain

Using Crow Intelligence to Fight Pollution: Inside Sweden’s Corvid Cleaning Project

From Stone to Shelter: Innovative Housing Beneath France’s Historic Bridges

Redefining Public Restrooms in South Korea: Hygiene, Dignity, and Accessibility for All

How Cyclic Sighing Became One of the Most Effective Breathing Techniques for Reducing Anxiety
Hepatitis C Virus Detected in Brain Tissue: A Potential Link to Schizophrenia and Bipolar Disorder

Top 10 Safest Places if World War 3 Broke Out
Scientists Sequence the World’s Oldest RNA from a 40,000-Year-Old Woolly Mammoth

Novel Neural Pathway Identified as Key to Reversing Autism-Related Behaviors

Why seniors should keep their socks on even at home
What Once Seemed Impossible: Lab-Grown Spinal Cord Sparks Hope for Millions
Lab-Grown Spinal Cord Tissue Marks a New Era in Paralysis Treatment
How Hormonal Birth Control May Reshape the Brain: New Neuroscience Insights
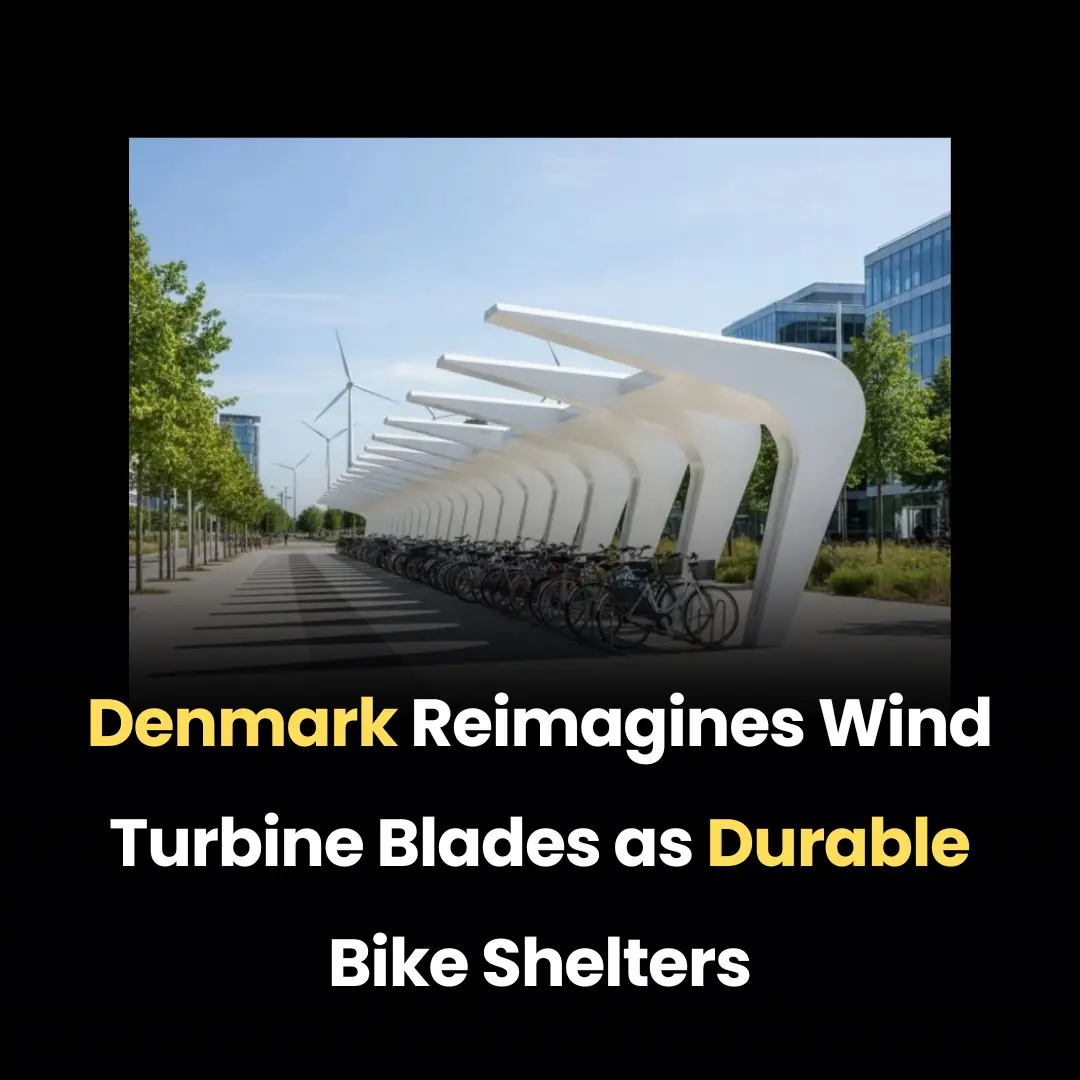
Denmark Reimagines Wind Turbine Blades as Durable Bike Shelters

World-First Recovery Achieved in Terminal Brain Cancer Case

A High School Robotics Team Built What Insurance Refused — And Gave a 2-Year-Old the Gift of Independent Movement

The Man Who Became “Dad” to Millions: How Rob Kenney Turned His Pain Into a Global Mission
News Post

Vaseline Uses and Benefits for Skin, Lips, and Hair

10 simple ways to reduce dust at home that most people overlook
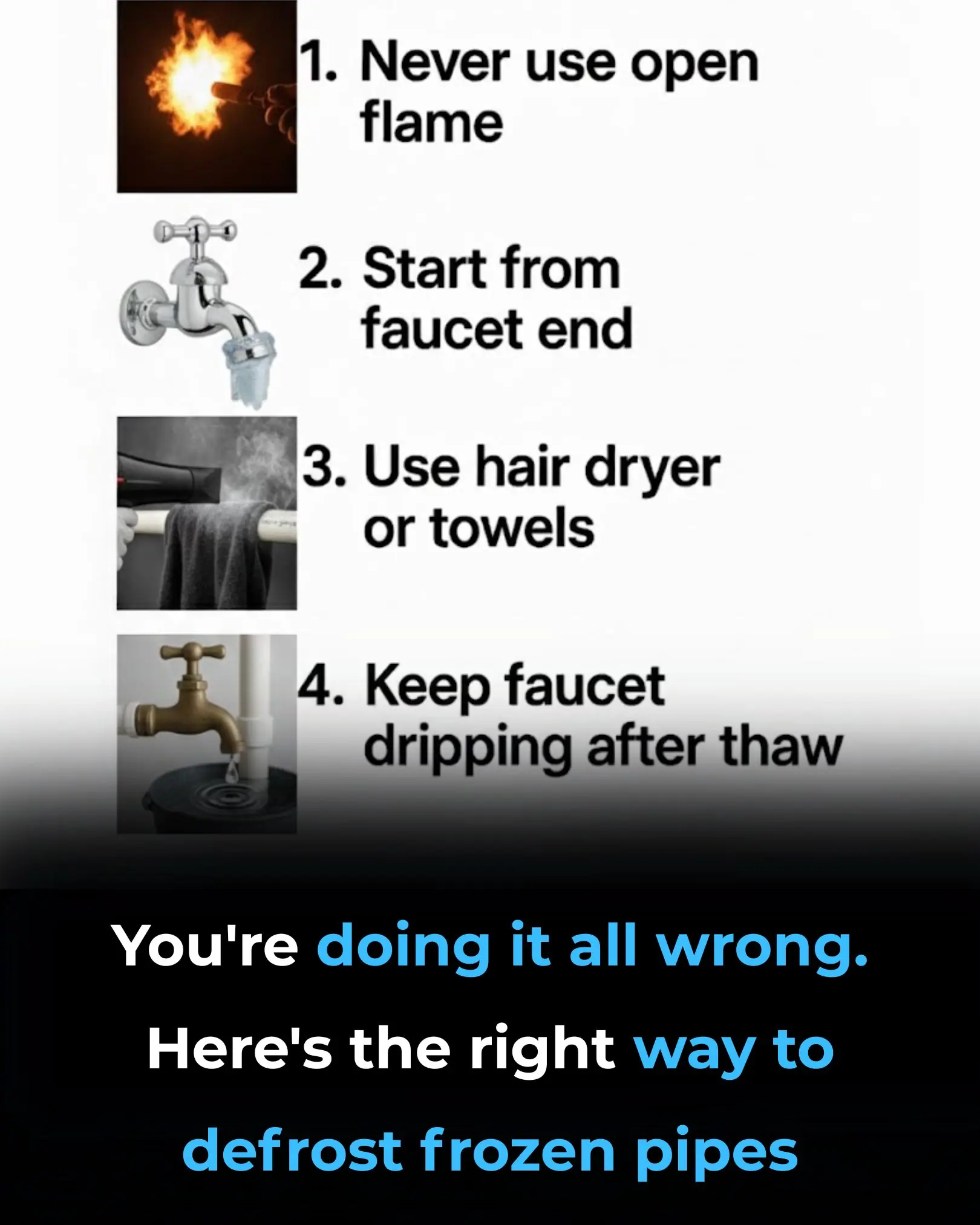
You’re Doing It All Wrong: Here’s the Right Way to Defrost Frozen Pipes

7 Powerful Fruits to Preserve Muscle Strength and Energy After 50

I Didn’t Know!

The #1 FASTEST way to reverse fatty liver naturally

Could the bacteria in your nose be causing Alzheimer’s?

How to treat nerve pain in the foot, toes & legs
The air conditioner only has wind but is not cool. Don't rush to call a repairman and waste money. If you do this, it will be cold.

The more flowers the money tree has, the more luck it attracts: Do this and the money tree flowers will grow 5 times faster.

When boiling duck, don't add ginger and cold water. Add this to remove all the bad smell from the meat and you won't get tired of eating it.

Avocado Seeds: The Overlooked Nutritional Power Inside the Fruit

Bee venom wiped out 100% of aggressive breast cancer cells in just 6 hours
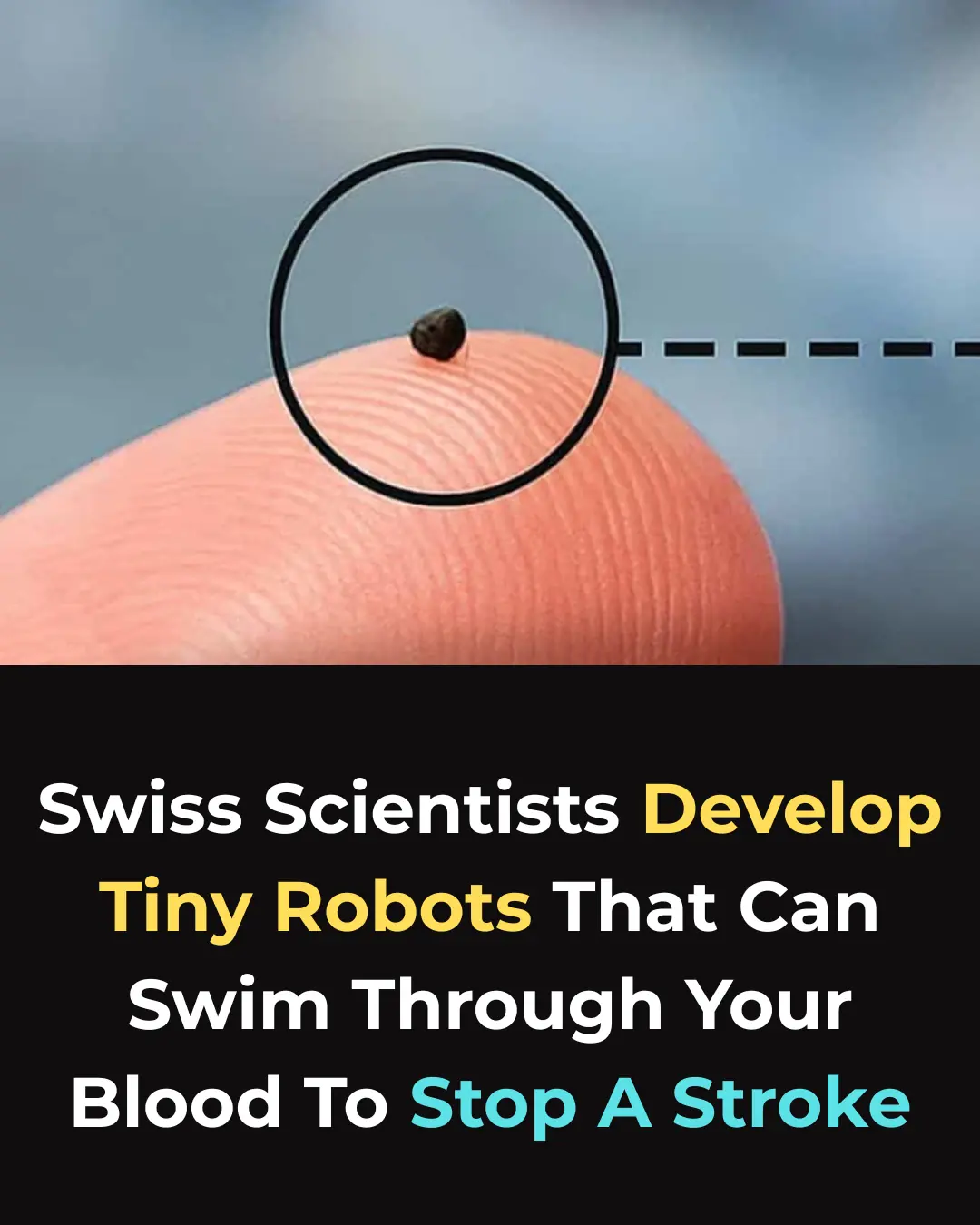
A New Breakthrough: Magnetic Microrobots Designed to Navigate Blood Vessels and Stop Strokes

10 Ways to Lower Uric Acid Naturally
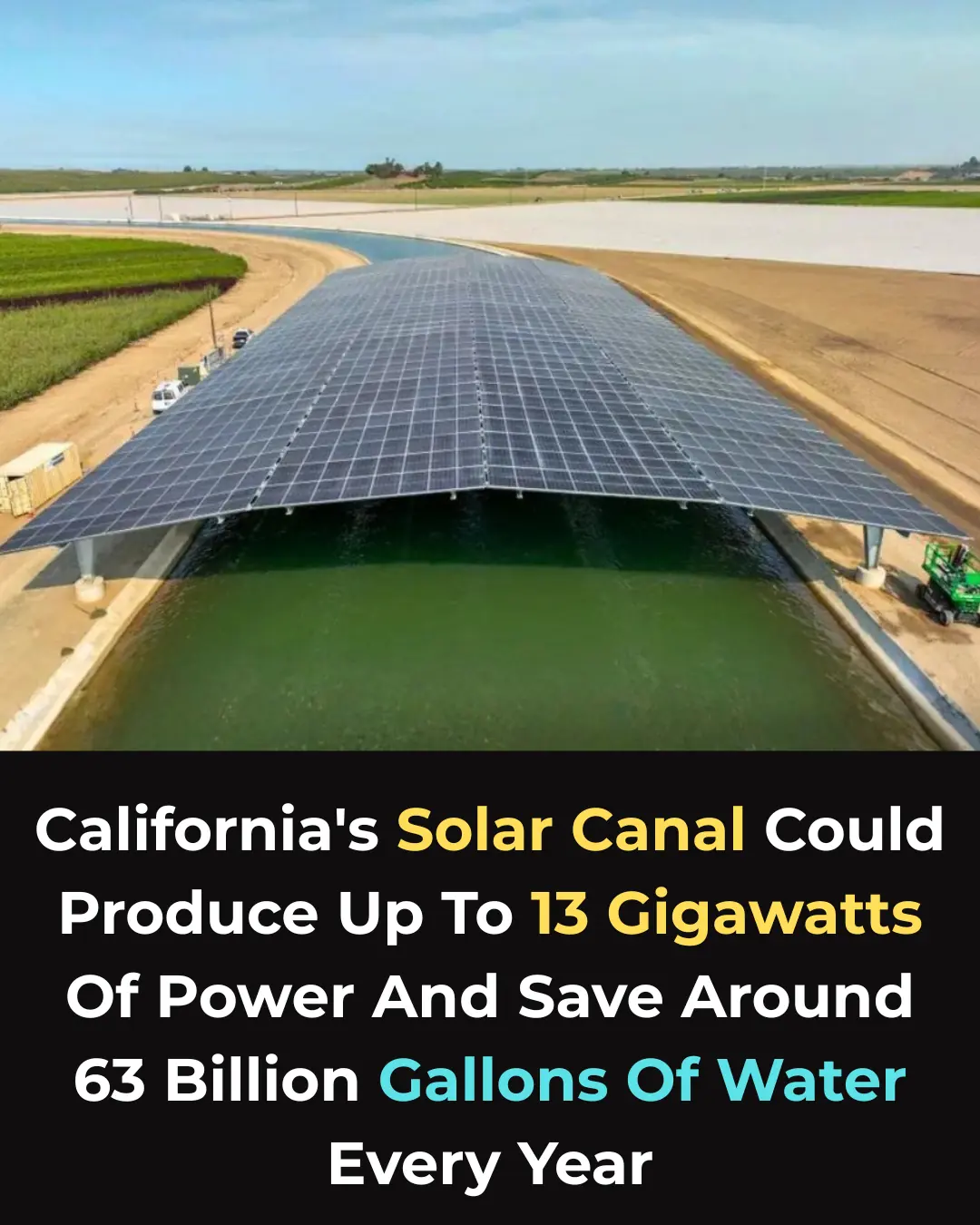
A Dual Climate Solution: Solar Panels Over Canals Could Save Billions of Gallons of Water

From Crow to Cleaner: How Feathered Geniuses Are Fighting Litter in Spain

6 Foods That Can Drain Your Calcium and Weaken Bones
