
Scientists Trigger Cancer Cells to Destroy Themselves From the Inside Out
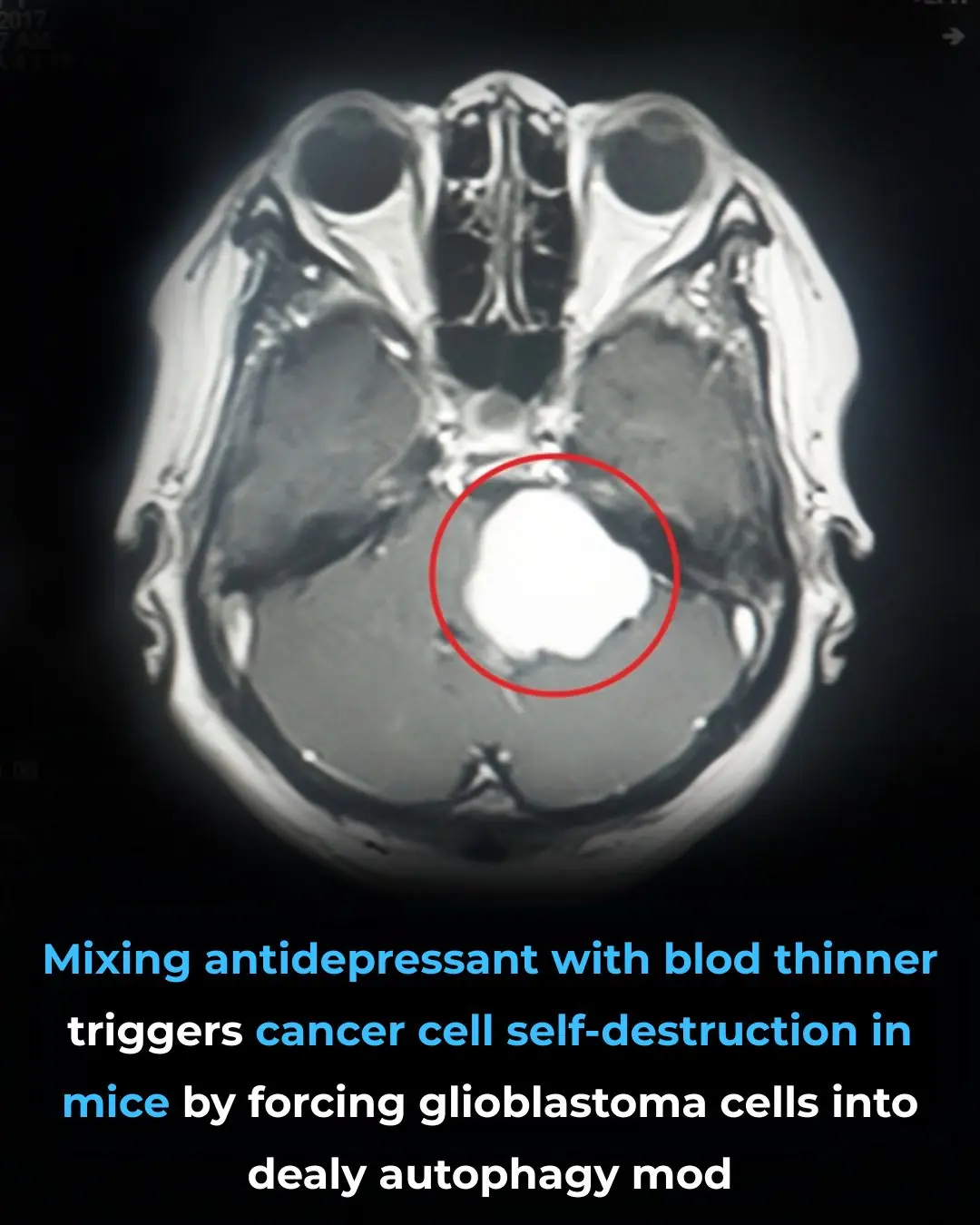
In a breakthrough that has captured the attention of the medical community, researchers have uncovered a surprising new strategy against one of the deadliest forms of brain cancer. By combining two existing medications—neither originally designed to treat cancer—scientists were able to push aggressive tumor cells into a state of fatal self-destruction.
The discovery centers on glioblastoma, an extremely aggressive brain cancer known for its resistance to treatment and poor survival rates. In laboratory experiments using mice, the new drug combination forced cancer cells to activate a biological process so intensely that they effectively consumed themselves from the inside out.
The Challenge of Glioblastoma
Glioblastoma is considered one of the most lethal cancers in modern oncology. Even with surgery, radiation, and chemotherapy, the average survival time remains limited, and recurrence is common. One reason for this resilience is the cancer’s ability to adapt its metabolism and evade cell death.
Traditional treatments aim to poison cancer cells directly or damage their DNA. This new approach, however, takes a fundamentally different path: it convinces cancer cells to activate their own destruction mechanisms.
A Surprising Drug Combination
In the study, researchers combined:
-
A commonly prescribed antidepressant
-
A widely used blood thinner
Individually, these drugs had little effect on tumor survival. But together, they produced a powerful and unexpected result. The glioblastoma cells entered a state of uncontrolled autophagy, a process often described as cellular “self-eating.”
When Autophagy Turns Deadly
Autophagy is normally a healthy and essential function. Cells use it to:
-
Remove damaged components
-
Recycle nutrients
-
Maintain internal balance
Under normal conditions, autophagy protects cells. But when pushed beyond a critical threshold, it becomes lethal.
In this case, the drug combination caused cancer cells to over-activate autophagy, triggering a catastrophic metabolic collapse. Instead of cleaning themselves up, the tumor cells dismantled vital internal structures until they could no longer survive.
Remarkably, surrounding healthy brain cells were largely unaffected, suggesting a level of selectivity that is rare in cancer treatment.
A Metabolic Trap Cancer Couldn’t Escape
Researchers describe the effect as a toxic metabolic trap. Glioblastoma cells, already under extreme metabolic stress, were unable to regulate the runaway autophagy triggered by the drugs. Once initiated, the process became irreversible.
Rather than dying slowly through external damage, the cancer cells effectively activated their own execution program.
Why This Discovery Matters
One of the most promising aspects of this breakthrough is that both drugs are already approved for human use in other medical contexts. This significantly lowers the barrier to clinical testing, as safety profiles, dosage limits, and side effects are already well documented.
If future studies confirm these findings in humans, clinical trials could begin far sooner than with entirely new experimental compounds.
A Shift in Cancer Treatment Thinking
This research reflects a growing shift in oncology: instead of attacking cancer cells head-on, scientists are learning how to exploit the cancer’s own survival mechanisms against it.
By hijacking internal processes like autophagy, metabolism, and stress response pathways, treatments may become:
-
More precise
-
Less damaging to healthy tissue
-
Harder for cancer to resist
Important Limitations and Next Steps
While the results are encouraging, it is crucial to note that these findings are currently based on animal models and laboratory experiments. Human biology is more complex, and not all promising cancer therapies translate successfully to clinical use.
Further research will be needed to:
-
Confirm safety and effectiveness in humans
-
Determine optimal dosing strategies
-
Understand potential long-term effects
-
Identify which patients may benefit most
Hope for a Historically Devastating Disease
Despite these limitations, the implications are profound. Glioblastoma has long been associated with limited treatment options and bleak prognoses. The possibility that a simple, overlooked combination of existing drugs could weaken—or even defeat—this cancer offers renewed hope to patients and researchers alike.
Conclusion
This discovery does not represent a cure—yet. But it signals something equally important: new ways of thinking about cancer. Sometimes, the most powerful solutions are not found in exotic new compounds, but in reimagining how familiar tools can be used.
By forcing cancer cells to destroy themselves from within, scientists may have opened the door to a new kind of warfare against some of the most devastating diseases known to medicine.
News in the same category


These Ideas Are Amazing: 10 Surprising Ways Dryer Sheets Can Make Your Life Easier
My Uncle Swears by This 6-Minute Trick to Stop Ice Buildup Inside Garage Door Seals — Here’s How It Works
My Uncle Swears by This 6-Minute Trick to Stop Ice Buildup Inside Garage Door Seals — Here’s How It Works

Don’t Get Rid of Old Tree Stumps — Here Are 10 Brilliant Ways to Re-Use Them in Your Garden

Scientists Warn: Don’t Strip Moss Off Surfaces—It Absorbs Four Times More CO₂ Than Trees

Study Says That Crows Can Hold A Grudge For Up To 17 Years
What It Means If Your Fingers Turn White When It’s Cold
There are foods that go straight to the belly. Check comments 👇

Most Don’t Know: 12 Brilliant Ways to Use WD-40 Around the House (and What to Avoid)

There’s a Crusty Spot That Keeps Scabbing and Reopening — What Could It Be?

My Nana Taught Me This Hack to Whiten Yellow Pillows in 5 Minutes With Zero Work — Here’s How It Actually Works
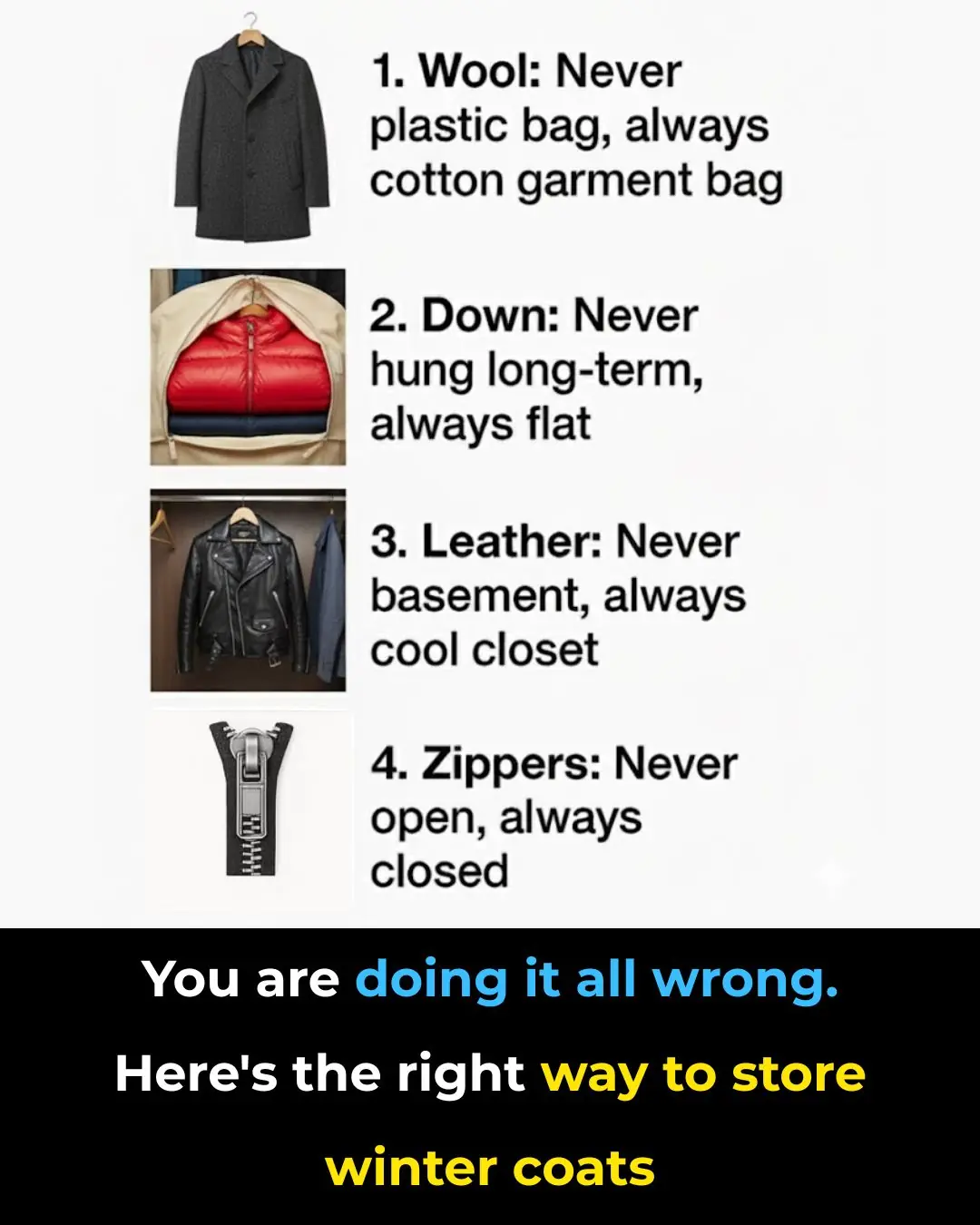
You’re Probably Storing Winter Coats All Wrong — Here’s the Right Way to Do It
A Chocolate Compound May Help the Brain Reclaim Its Youth
Your Outdoor Faucet Froze and Water Is Leaking Indoors — What to Do Immediately Before a Plumber Arrives

Why Christmas Cactus Buds Suddenly Fall Off — And What Usually Causes It

The Easy, Proven Way to Grow Lavender from Cuttings Most Gardeners Don’t Know

Everyone Has Made This Mistake When Using An Air Fryer
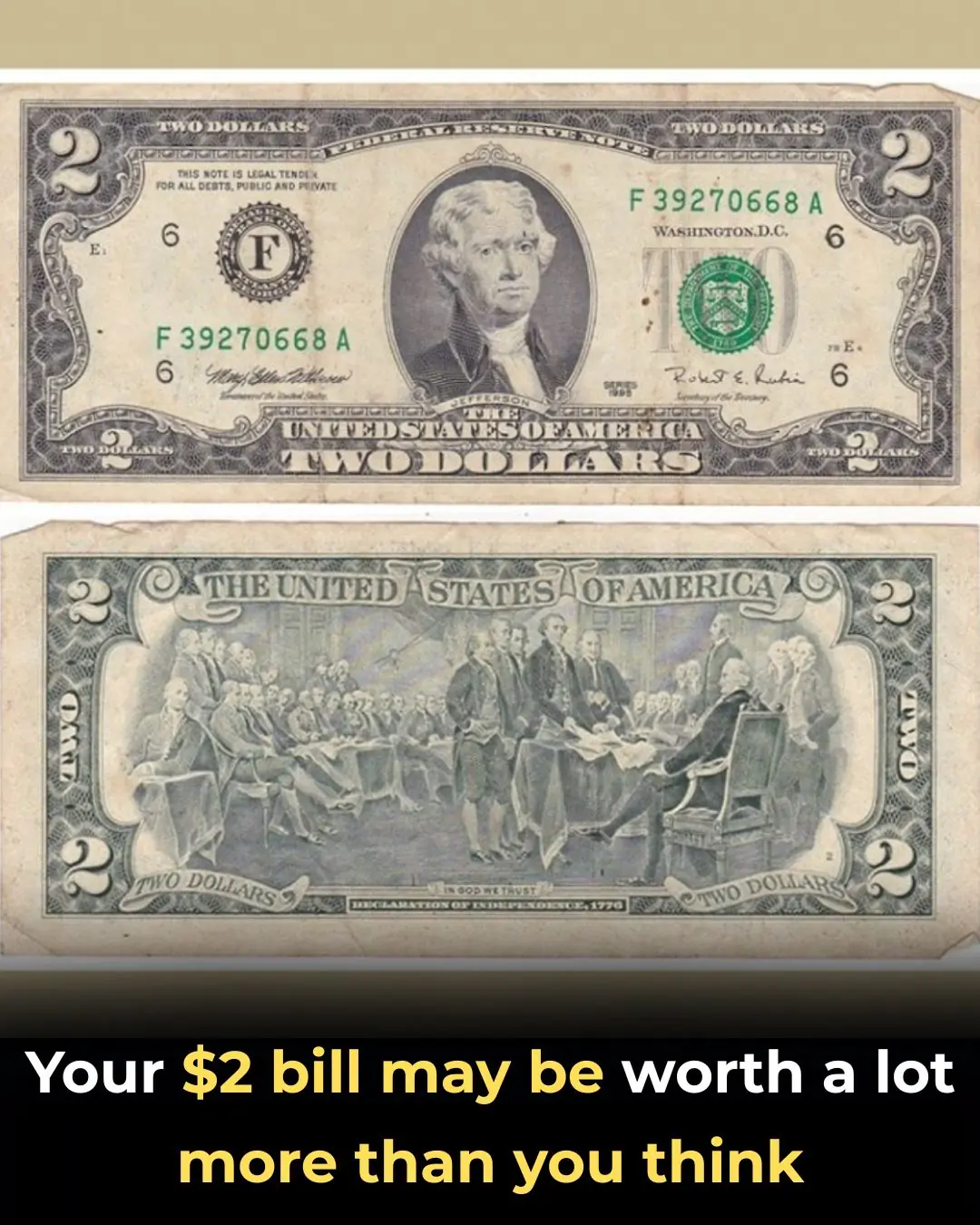
Your $2 Bill May Be Worth a Lot More Than You Think
News Post

25 Remarkable Benefits of Guava Leaves and How to Use Them Safely
Study Finds This Popular Sweetener Damages the Brain’s Protective Barrier

Study Finds a Mother’s Early Bond With Her Baby Can Shape a Child’s Sleep for Years
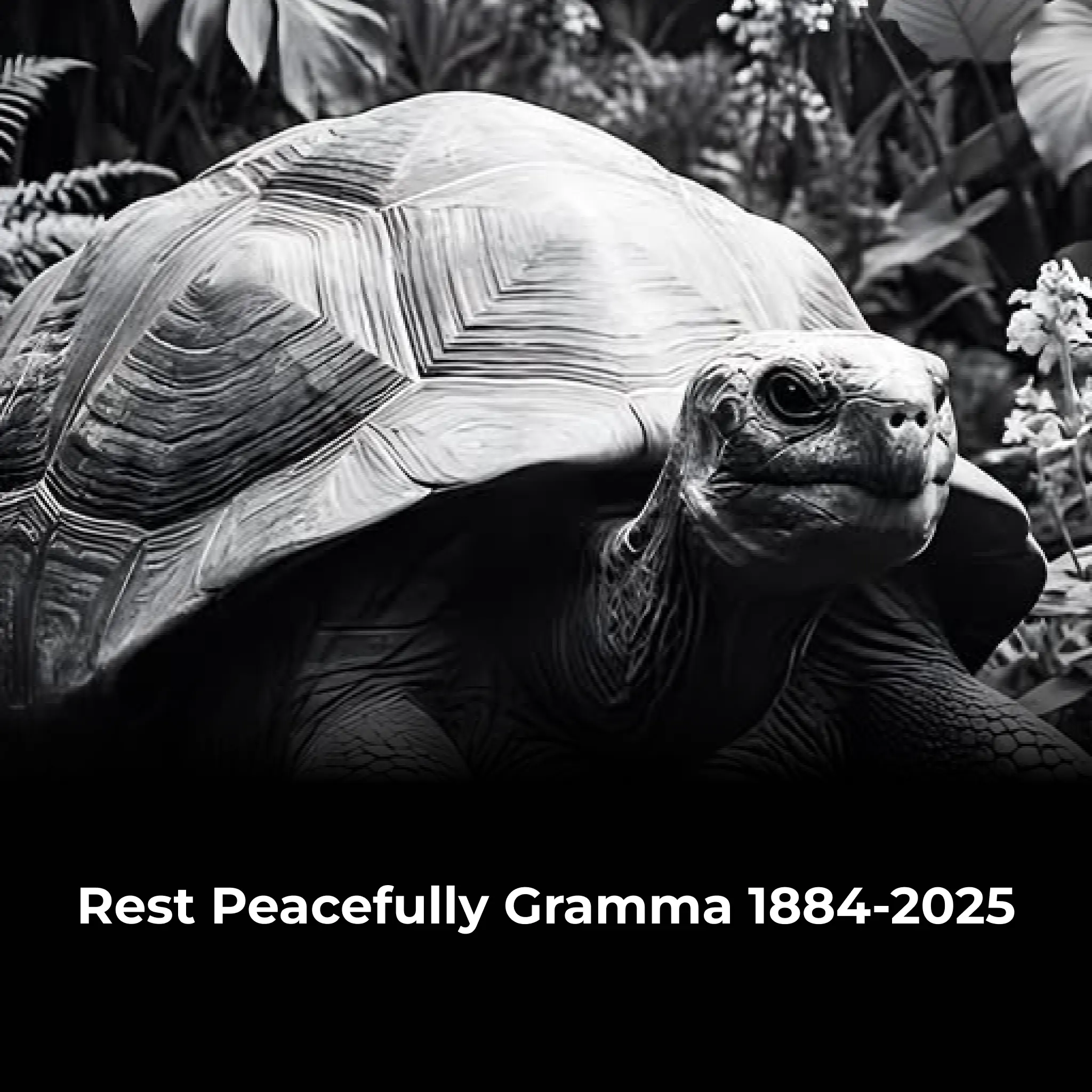
Gramma the Tortoise: A Remarkable Life Spanning Three Centuries

California Surpasses Japan to Become the Fourth-Largest Economy in the World

Why Aging Skin Develops a Distinct Body Odor—and What Science Says Can Help
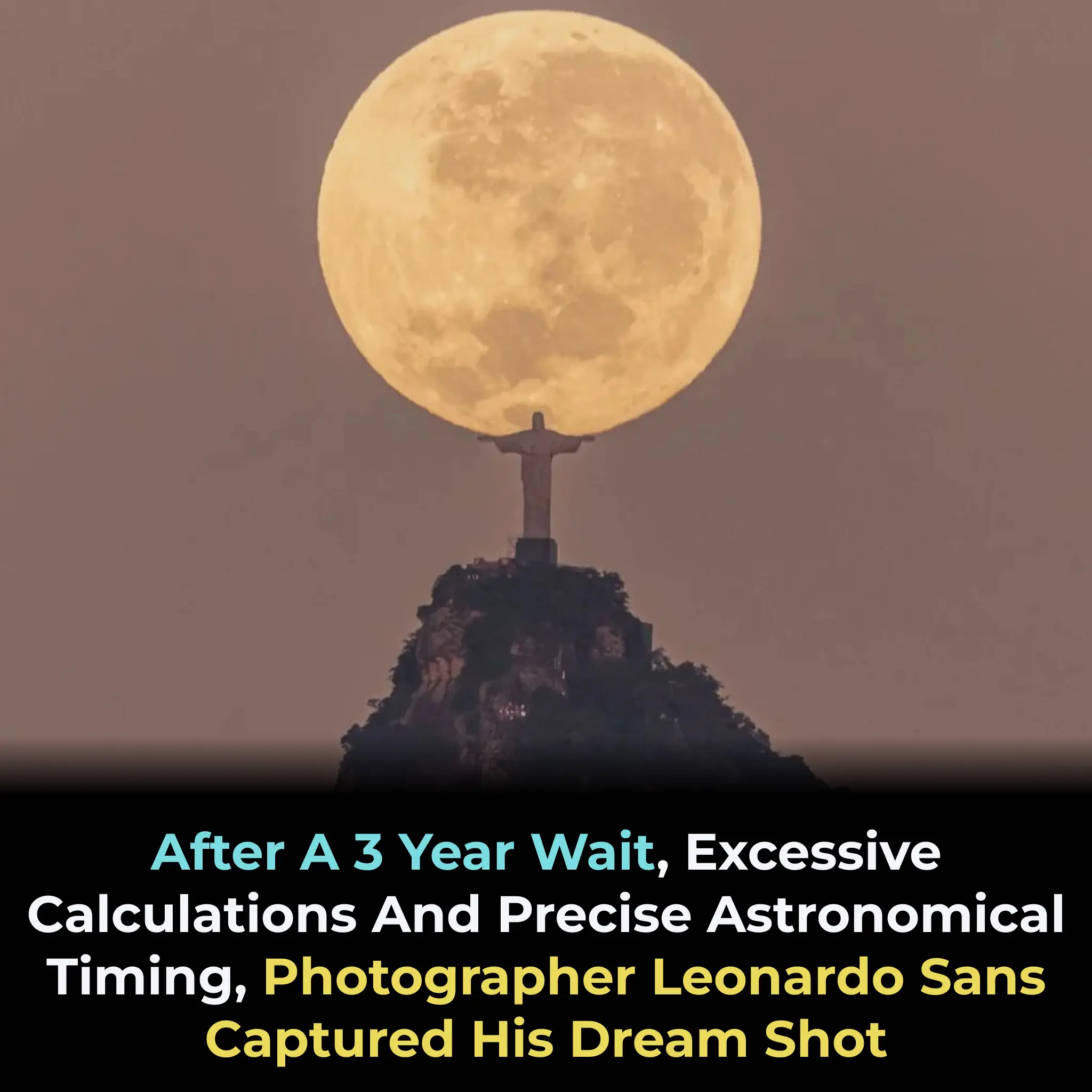
Photographer Captures Dream Shot of Full Moon Over Christ the Redeemer After Three Years of Effort

China Successfully Tests 3D-Printed Micro Turbojet Engine in Landmark Flight Achievement

Swiss Researchers Trial Blood Filtration Device for Alzheimer's Treatment

Bear Takes Over Truckee Diner in Hilarious Culinary Heist

Many people believe they need to walk ten thousand steps daily to stay healthy

The Quieting Skies: A Stark Decline in North America's Bird Population
Does This Drink Really Harm Your Bones? The Truth Behind Soda and Your Health
Oregano: The Small Plant with Big Health Benefits

Sea Otter Takes Over Santa Cruz Surf Scene: A Bold and Unpredictable Presence

Australia's Revolutionary Bionic Eye: A New Era in Restoring Vision

10 Best Collagen Gels For Wrinkle Free Glowing Skin

Why You Might Want to Stop Removing Tomato Suckers: What Gardeners Are Starting to Realize

Banana Blossom: Health Benefits, Recipes, and Traditional Uses
