Shingles Vaccination Associated With Reduced Cardiovascular and Dementia Risk Despite Breakthrough Infections
Herpes zoster, commonly known as shingles, has long been recognized as a painful viral illness caused by reactivation of the varicella-zoster virus. Beyond its well-known dermatologic and neurologic complications, growing evidence suggests that shingles is associated with a significantly increased risk of major cardiovascular events and neurodegenerative conditions such as dementia. New research presented at IDWeek 2025 adds an important dimension to this understanding, demonstrating that vaccination against herpes zoster is associated with a reduced risk of both cardiovascular events and dementia—even among individuals who experience breakthrough infections over a five-year period.
Shingles and Its Broader Health Implications
Shingles occurs when the varicella-zoster virus, which remains dormant in nerve tissue after a primary chickenpox infection, reactivates later in life. The condition primarily affects older adults and individuals with compromised immune systems, including people living with HIV. While shingles is often characterized by a painful, blistering rash, its impact extends well beyond the skin.
Multiple studies have linked herpes zoster infection to systemic inflammation, vascular injury, and immune dysregulation. These processes are believed to contribute to an increased risk of stroke, myocardial infarction, and other major adverse cardiovascular events. Additionally, neuroinflammatory pathways activated during shingles episodes have been implicated in cognitive decline and dementia, raising concerns about the long-term neurological consequences of the infection.
The Role of Vaccination in Reducing Long-Term Risk
Vaccination against herpes zoster has been shown to significantly reduce the incidence and severity of shingles. However, no vaccine is completely protective, and breakthrough infections—cases of shingles occurring despite prior vaccination—can still occur. Until now, it was unclear whether vaccination offered any protective benefit against long-term complications in individuals who experience such breakthrough infections.
The study presented at IDWeek 2025 provides compelling evidence that vaccination may confer benefits beyond infection prevention. Researchers found that vaccinated individuals who developed shingles nonetheless had a lower risk of major cardiovascular events and dementia over a five-year follow-up period compared with unvaccinated individuals who developed shingles.
Key Findings From IDWeek 2025
According to the study, shingles infection was associated with an elevated risk of both cardiovascular disease and dementia, reinforcing previous research linking herpes zoster to systemic and neurological complications. However, among vaccinated individuals who experienced breakthrough shingles infections, the risk of these outcomes was significantly reduced.
The protective association persisted over five years, suggesting that vaccination may attenuate the inflammatory and vascular damage triggered by herpes zoster reactivation. These findings were observed across diverse populations, including older adults and people living with HIV, who are known to have a higher baseline risk for shingles and its complications.
Implications for People Living With HIV
People with HIV face a disproportionately higher risk of herpes zoster due to immune dysfunction, even when viral suppression is achieved with antiretroviral therapy. They also experience higher rates of cardiovascular disease and cognitive impairment compared with the general population.
The study’s findings are particularly relevant for this group, as they suggest that shingles vaccination may offer dual protection—reducing not only the incidence of shingles but also the risk of serious long-term complications. Even in cases where vaccination does not completely prevent infection, the observed reduction in cardiovascular and dementia risk highlights the potential role of vaccination as a broader preventive strategy in this vulnerable population.
Potential Biological Mechanisms
Although the exact mechanisms underlying these protective effects remain under investigation, several hypotheses have been proposed. Vaccination may reduce viral replication and limit the intensity and duration of inflammation during breakthrough infections. This, in turn, could lessen endothelial damage, reduce prothrombotic states, and minimize neuroinflammation—key factors implicated in cardiovascular disease and cognitive decline.
Additionally, immune priming induced by vaccination may lead to a more controlled immune response upon viral reactivation, preventing the exaggerated inflammatory cascades associated with severe systemic complications.
Public Health and Clinical Implications
These findings have important implications for public health policy and clinical practice. They suggest that the benefits of shingles vaccination extend beyond preventing rash and postherpetic neuralgia, encompassing protection against serious cardiovascular and neurological outcomes.
For clinicians, the data reinforce current recommendations to vaccinate eligible adults, particularly older individuals and those with immunocompromising conditions such as HIV. For policymakers, the results support broader implementation of shingles vaccination programs as a cost-effective strategy to reduce long-term disease burden.
Future Research Directions
While the results presented at IDWeek 2025 are promising, further research is needed to confirm these findings in randomized clinical trials and to better understand the biological mechanisms involved. Additional studies may also help determine whether the magnitude of benefit varies by vaccine type, timing of vaccination, or patient characteristics.
Long-term follow-up and real-world data will be essential to refining vaccination guidelines and maximizing the protective benefits for high-risk populations.
Conclusion
Shingles is increasingly recognized as a condition with far-reaching consequences, including an elevated risk of cardiovascular events and dementia. New evidence presented at IDWeek 2025 suggests that vaccination against herpes zoster is associated with a reduced risk of these serious outcomes, even among individuals who experience breakthrough infections over a five-year period.
These findings underscore the importance of shingles vaccination not only as a preventive measure against acute infection but also as a potential tool for reducing long-term cardiovascular and neurological risks—particularly in vulnerable populations such as older adults and people living with HIV.
News in the same category


Why Ages 36–46 Matter: Midlife as a Critical Window for Long-Term Health

Mebendazole as a Repurposed Therapy for Glioblastoma: Evidence from Preclinical Research
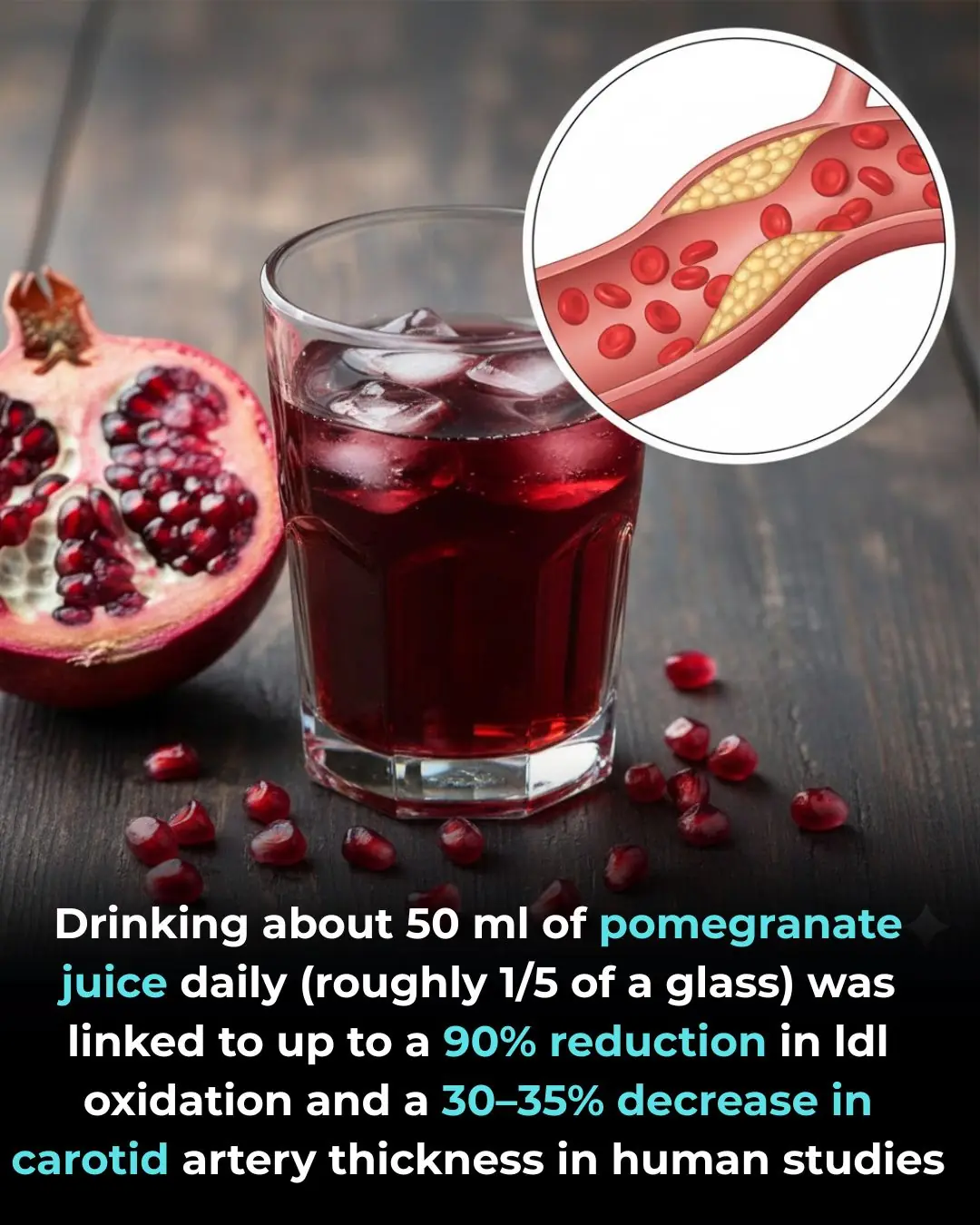
Pomegranate Juice and Cardiovascular Protection: Evidence from Human Clinical Studies

Synergistic Tumor Suppression by Vitamin K2 and Active Vitamin D in Triple-Negative Breast Cancer Cells

Thiamine Tetrahydrofurfuryl Disulfide (TTFD) as a Potential Supportive Intervention in Autism: Evidence from a Pilot Study
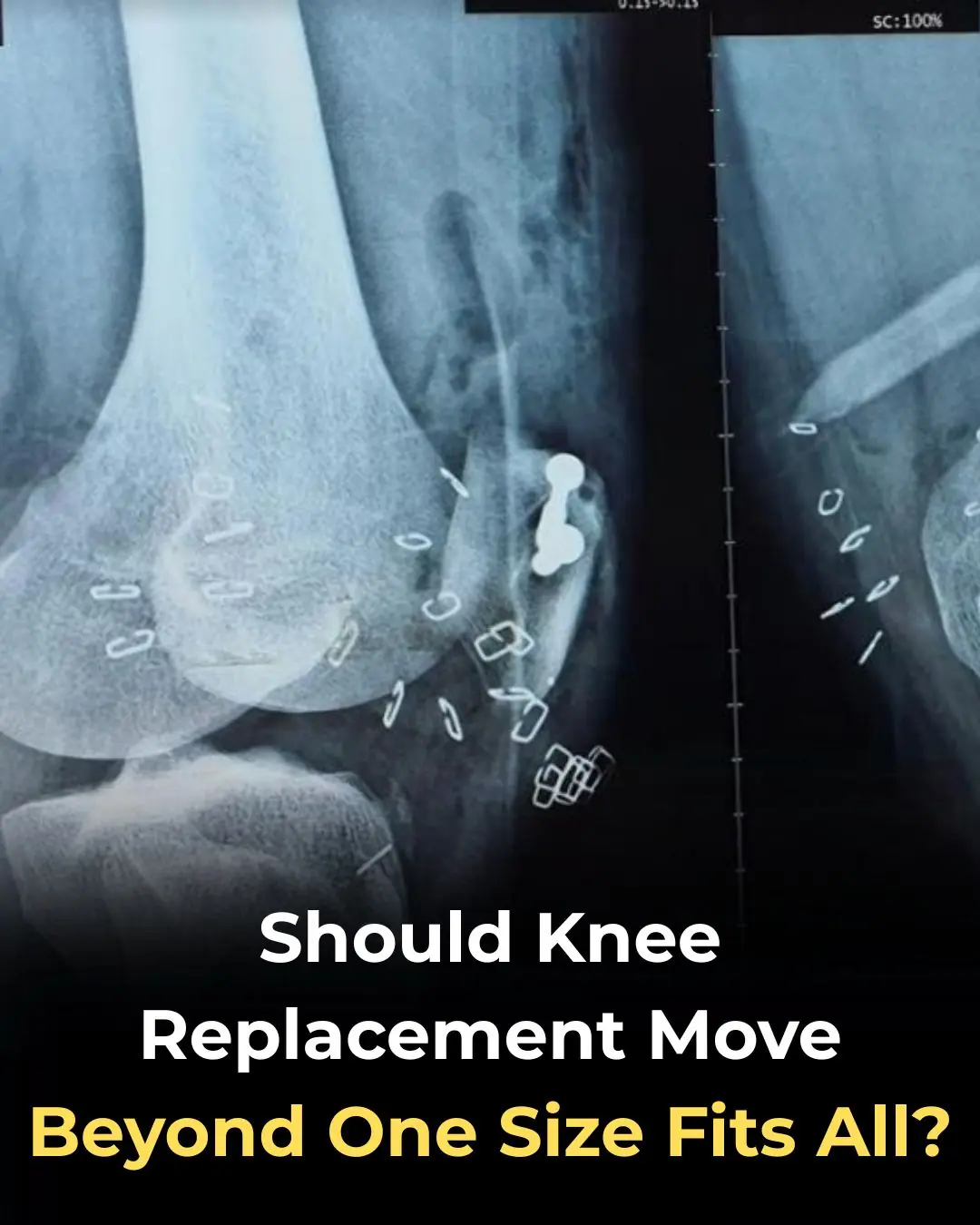
Should Knee Replacement Move Beyond One-Size-Fits-All Alignment?
Early Use of Glucocorticoids Reduces Mortality in Community-Acquired Pneumonia in Low-Resource Settings
8 Early Signs of Diabetes That Many People Overlook

Bad Habits After Washing Clothes That Can Make the Whole Family Sick! Many People Overlook This Detail
How do people who take naps and those who don't? Experts reveal surprising truth
Of particular note, these four unusual pains occurring every morning may be a warning sign of a tumor in the body

Scientifically Proven Health Benefits of Papaya (Fruit) + Uses for the Seeds
10 Habits That Harm Your Heart That You Probably Didn’t Know About

How to Get Rid of Muscle Soreness: Home Remedies That Really Work

Crusty sore on my lip won’t go away. Appointment is impossible to get right now. What is this?

Coffee Consumption, Additives, and Mortality Risk: Evidence from a Large U.S. Cohort Study

Kimchi Consumption and Immune Balance: Evidence from a Controlled Human Trial

Repurposing Itraconazole as an Anticancer Agent: Mechanisms and Clinical Potential
News Post

Optimism as a Psychosocial Predictor of Exceptional Longevity

Why Ages 36–46 Matter: Midlife as a Critical Window for Long-Term Health

Mebendazole as a Repurposed Therapy for Glioblastoma: Evidence from Preclinical Research
Pomegranate Juice and Cardiovascular Protection: Evidence from Human Clinical Studies

Synergistic Tumor Suppression by Vitamin K2 and Active Vitamin D in Triple-Negative Breast Cancer Cells

Thiamine Tetrahydrofurfuryl Disulfide (TTFD) as a Potential Supportive Intervention in Autism: Evidence from a Pilot Study
Should Knee Replacement Move Beyond One-Size-Fits-All Alignment?
Early Use of Glucocorticoids Reduces Mortality in Community-Acquired Pneumonia in Low-Resource Settings

At thirty-seven, I walked into the Grand Westbrook Hotel in downtown Chicago wearing a simple black dress and a wool coat I’d owned for years.

I worked abroad for 5 years to buy a house for my mother – When I returned, meeting my mother was not like I imagined.

THE MORNING AFTER THE WEDDING, MY HUSBAND AND I WERE ALREADY PACKING FOR HONEYMOON WHEN I GOT A CALL FROM THE REGISTRY OFFICE: ‘SORRY, WE CHECKED YOUR DOCUMENTS AGAIN… YOU NEED TO COME IN & SEE THIS IN PERSON. COME ALONE — AND DON’T TELL YOUR HUSB

I quit my career because my husband said, “A real wife stays home.” I did—ten years of silence and sacrifice. Then he filed for divorce. His lawyer smirked, “She has no skills.

“Just the thought of sleeping with that fat pig makes me sick.” I heard my son-in-law say this about my daughter the night before their wedding. He and his friends laughed like it was nothing… But in the end, I was the one who had the last laugh.

I Was Seven Months Pregnant, Carrying Groceries Up Three Flights Of Stairs While My Husband Sat On The Couch Playing Video Games.
Boiling chicken without tap water
8 Early Signs of Diabetes That Many People Overlook

Bad Habits After Washing Clothes That Can Make the Whole Family Sick! Many People Overlook This Detail

Soaking bananas in vinegar: 4 amazing uses recognized by experts, everyone loves it