Thiamine Tetrahydrofurfuryl Disulfide (TTFD) as a Potential Supportive Intervention in Autism: Evidence from a Pilot Study
Autism spectrum disorder (ASD) is a complex neurodevelopmental condition characterized by impairments in social communication, restricted interests, and repetitive behaviors. Although behavioral and educational interventions remain the mainstay of treatment, there is ongoing scientific interest in biological factors that may contribute to ASD symptoms, including abnormalities in energy metabolism, mitochondrial function, and micronutrient utilization. Among these, thiamine (vitamin B1) has attracted attention because of its central role in brain energy metabolism and neurotransmitter synthesis. A small but noteworthy pilot study published in Neuro Endocrinology Letters explored whether improving intracellular thiamine availability could lead to clinical improvements in children with autism.
The study investigated the effects of thiamine tetrahydrofurfuryl disulfide (TTFD), a fat-soluble and highly bioavailable derivative of vitamin B1. Unlike standard water-soluble thiamine, TTFD is designed to cross cell membranes more efficiently and increase intracellular thiamine concentrations, particularly in tissues with high metabolic demand such as the brain. In this NIH-indexed pilot trial, autistic children received TTFD at a dose of 50 mg twice daily for a period of two months.
Clinical outcomes were assessed using the Autism Treatment Evaluation Checklist (ATEC), a standardized tool commonly used to track changes in communication, sociability, sensory awareness, and health-related behaviors. In parallel, researchers measured biochemical markers related to thiamine metabolism to determine whether supplementation produced measurable physiological changes. This dual clinical–biochemical approach strengthened the exploratory nature of the study by linking symptom changes with underlying metabolic shifts.
By the end of the two-month intervention, 8 out of 10 children showed measurable clinical improvement according to ATEC scores. Although the magnitude and domains of improvement varied among participants, the overall trend suggested a positive response in a majority of the cohort. These clinical changes were accompanied by alterations in markers related to thiamine metabolism, indicating that TTFD supplementation was biologically active and successfully influenced thiamine-dependent pathways.
An additional and intriguing observation emerged from baseline assessments. Several children exhibited elevated levels of sulfur-reactive metals, particularly arsenic. The authors proposed that such metal exposure might interfere with thiamine-dependent enzymes or transport mechanisms, creating a functional thiamine deficiency at the cellular level even when dietary intake appears sufficient. In this context, TTFD “mass-loading” could potentially bypass impaired transport or enzymatic inhibition, restoring metabolic function in vulnerable neural pathways. This hypothesis aligns with broader literature suggesting interactions between micronutrient metabolism and environmental toxicants in neurodevelopmental disorders.
Despite these promising signals, the authors were careful to emphasize the limitations of their work. The study involved only ten participants, lacked a placebo-controlled design, and was conducted over a relatively short duration. As such, the findings cannot establish efficacy or support generalized clinical recommendations. Improvements could have been influenced by placebo effects, natural developmental changes, or unmeasured confounding factors. The results should therefore be interpreted as hypothesis-generating rather than confirmatory.
Nevertheless, the study is significant for several reasons. First, it highlights the importance of considering nutrient bioavailability and intracellular metabolism, not merely dietary intake, when evaluating nutritional interventions in ASD. Second, it suggests a potential link between impaired thiamine function and environmental metal exposure, opening new avenues for research into gene–environment–nutrient interactions. Finally, the relatively high response rate observed in this small cohort provides a rationale for larger, well-controlled trials.
In conclusion, the pilot study published in Neuro Endocrinology Letters suggests that supplementation with thiamine tetrahydrofurfuryl disulfide may lead to clinical improvements in some children with autism, possibly by correcting functional impairments in thiamine metabolism (Neuro Endocrinology Letters, NIH-indexed pilot study). While the evidence remains preliminary, it underscores the need for further controlled research to clarify mechanisms, identify responders, and determine whether optimized thiamine delivery could play a supportive role in the management of autism spectrum disorder.
News in the same category


Why Ages 36–46 Matter: Midlife as a Critical Window for Long-Term Health

Mebendazole as a Repurposed Therapy for Glioblastoma: Evidence from Preclinical Research
Pomegranate Juice and Cardiovascular Protection: Evidence from Human Clinical Studies

Synergistic Tumor Suppression by Vitamin K2 and Active Vitamin D in Triple-Negative Breast Cancer Cells
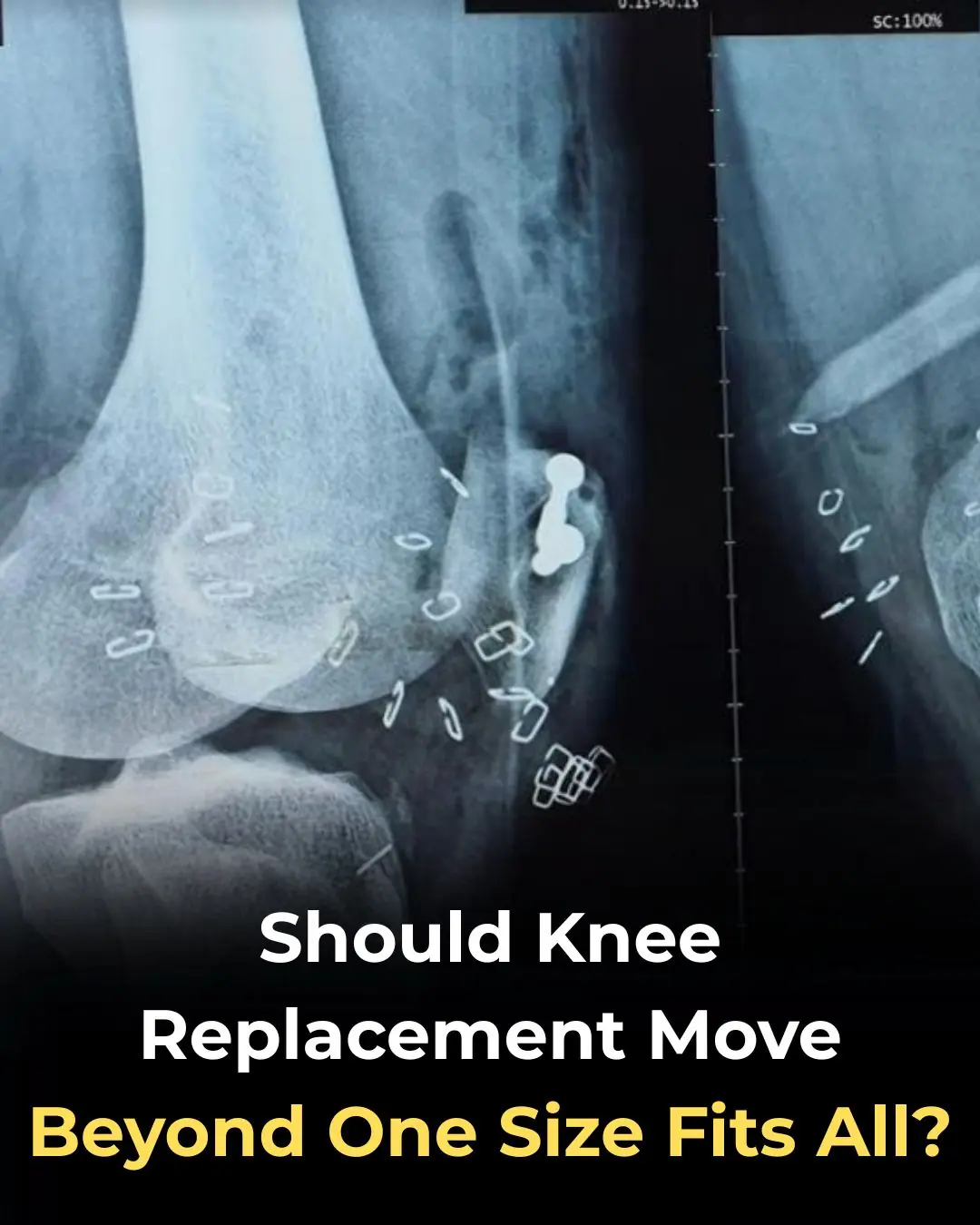
Should Knee Replacement Move Beyond One-Size-Fits-All Alignment?
Shingles Vaccination Associated With Reduced Cardiovascular and Dementia Risk Despite Breakthrough Infections
Early Use of Glucocorticoids Reduces Mortality in Community-Acquired Pneumonia in Low-Resource Settings
8 Early Signs of Diabetes That Many People Overlook

Bad Habits After Washing Clothes That Can Make the Whole Family Sick! Many People Overlook This Detail
How do people who take naps and those who don't? Experts reveal surprising truth
Of particular note, these four unusual pains occurring every morning may be a warning sign of a tumor in the body

Scientifically Proven Health Benefits of Papaya (Fruit) + Uses for the Seeds
10 Habits That Harm Your Heart That You Probably Didn’t Know About

How to Get Rid of Muscle Soreness: Home Remedies That Really Work

Crusty sore on my lip won’t go away. Appointment is impossible to get right now. What is this?

Coffee Consumption, Additives, and Mortality Risk: Evidence from a Large U.S. Cohort Study

Kimchi Consumption and Immune Balance: Evidence from a Controlled Human Trial

Repurposing Itraconazole as an Anticancer Agent: Mechanisms and Clinical Potential
News Post

Optimism as a Psychosocial Predictor of Exceptional Longevity

Why Ages 36–46 Matter: Midlife as a Critical Window for Long-Term Health

Mebendazole as a Repurposed Therapy for Glioblastoma: Evidence from Preclinical Research
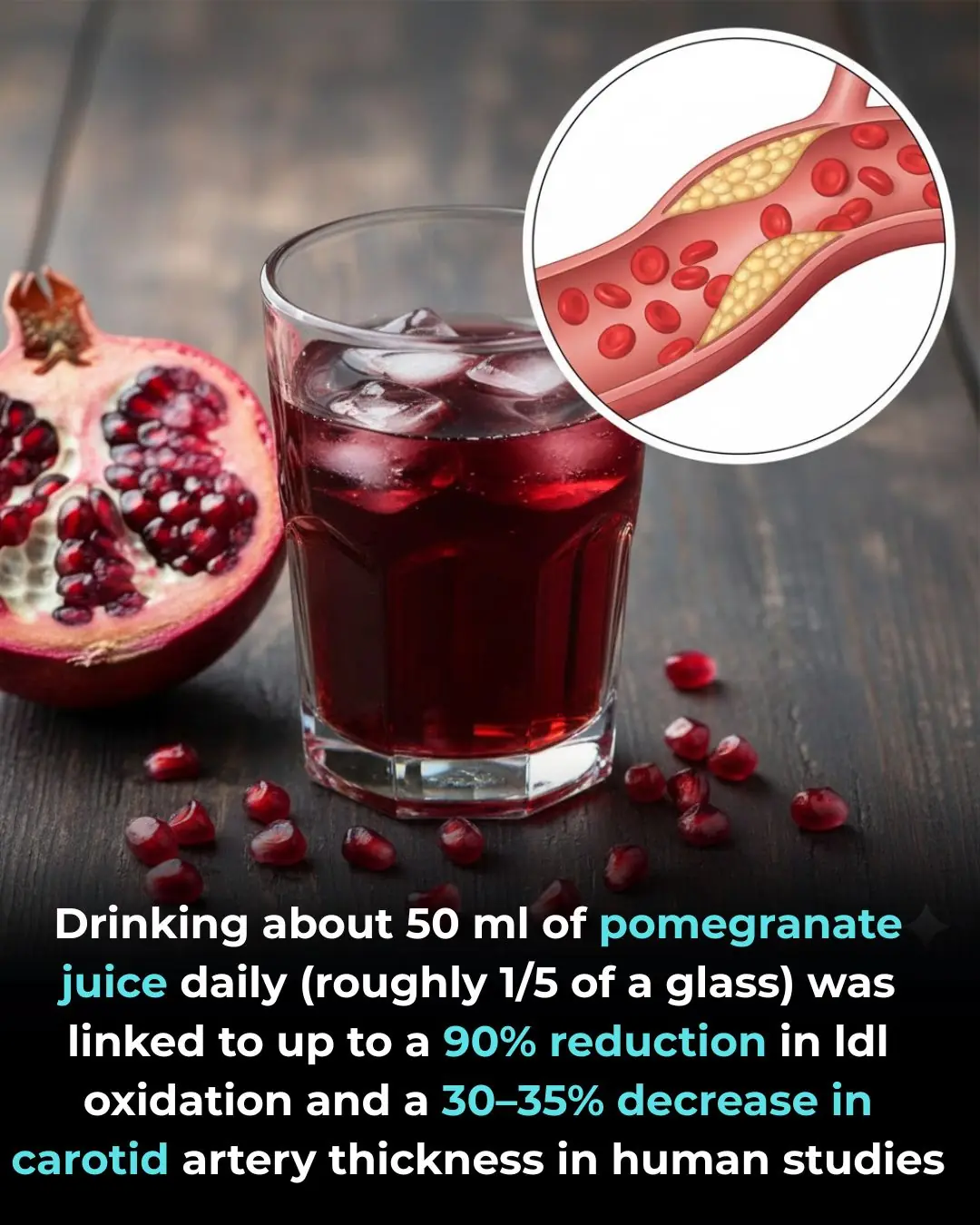
Pomegranate Juice and Cardiovascular Protection: Evidence from Human Clinical Studies

Synergistic Tumor Suppression by Vitamin K2 and Active Vitamin D in Triple-Negative Breast Cancer Cells
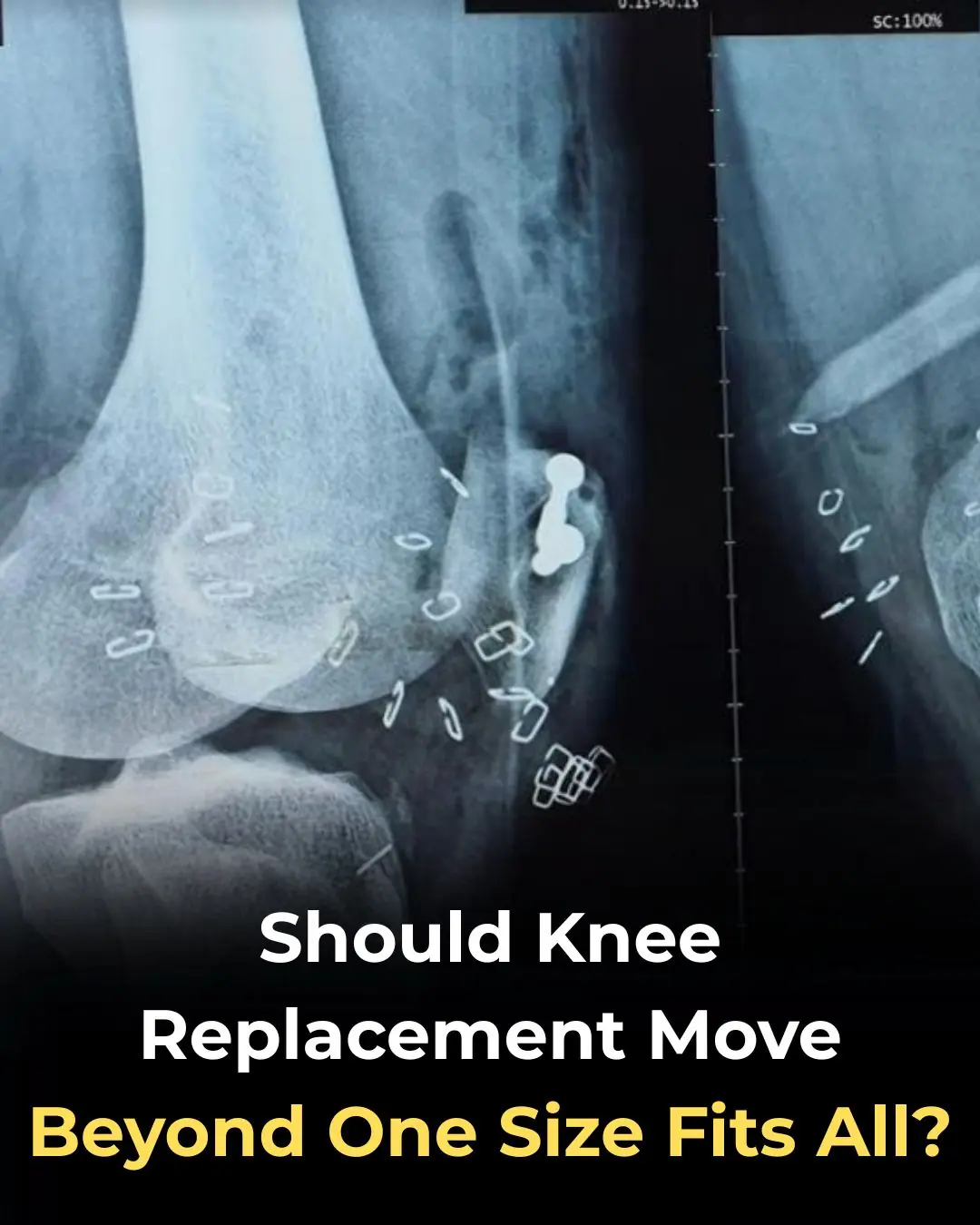
Should Knee Replacement Move Beyond One-Size-Fits-All Alignment?
Shingles Vaccination Associated With Reduced Cardiovascular and Dementia Risk Despite Breakthrough Infections
Early Use of Glucocorticoids Reduces Mortality in Community-Acquired Pneumonia in Low-Resource Settings

At thirty-seven, I walked into the Grand Westbrook Hotel in downtown Chicago wearing a simple black dress and a wool coat I’d owned for years.

I worked abroad for 5 years to buy a house for my mother – When I returned, meeting my mother was not like I imagined.

THE MORNING AFTER THE WEDDING, MY HUSBAND AND I WERE ALREADY PACKING FOR HONEYMOON WHEN I GOT A CALL FROM THE REGISTRY OFFICE: ‘SORRY, WE CHECKED YOUR DOCUMENTS AGAIN… YOU NEED TO COME IN & SEE THIS IN PERSON. COME ALONE — AND DON’T TELL YOUR HUSB

I quit my career because my husband said, “A real wife stays home.” I did—ten years of silence and sacrifice. Then he filed for divorce. His lawyer smirked, “She has no skills.

“Just the thought of sleeping with that fat pig makes me sick.” I heard my son-in-law say this about my daughter the night before their wedding. He and his friends laughed like it was nothing… But in the end, I was the one who had the last laugh.

I Was Seven Months Pregnant, Carrying Groceries Up Three Flights Of Stairs While My Husband Sat On The Couch Playing Video Games.
Boiling chicken without tap water
8 Early Signs of Diabetes That Many People Overlook

Bad Habits After Washing Clothes That Can Make the Whole Family Sick! Many People Overlook This Detail

Soaking bananas in vinegar: 4 amazing uses recognized by experts, everyone loves it