
10 Symptoms of Diabetes That May Show Up In Your Feet

Early Signs of Diabetes in the Feet You Should Never Ignore
Diabetes can affect nearly every part of the body, but the feet are often where the earliest warning signs appear. Because high blood sugar levels gradually damage circulation and nerves, foot issues can develop quietly over time. Recognizing these changes early is key to preventing more serious complications. Below are ten foot symptoms of diabetes to be aware of.
1. Burning or Sharp Pain
Some individuals with diabetes report a burning sensation or stabbing pain in their feet, even while resting. This happens when nerve damage sends faulty pain signals. The discomfort may come and go or worsen at night. If even light pressure or gentle touches feel painful, it could be a sign of advancing neuropathy. Keeping blood sugar under control may help slow this process.
2. Cold Feet Despite Warm Weather
Diabetes can restrict blood vessels, leading to poor circulation. As a result, your feet may feel cold even when the rest of your body is warm. While occasional coldness is normal, persistent chilly feet could signal circulation problems. Wearing warm socks, moving around regularly, and avoiding long periods of sitting can help stimulate blood flow.
3. Numbness or Tingling
Ongoing tingling or numbness in the feet may point to peripheral neuropathy, a common complication of diabetes. Reduced sensation makes it harder to notice cuts, blisters, or injuries, which raises the risk of infection. If you experience this often, check your feet daily to ensure there are no unnoticed wounds.
4. Frequent Foot Cramps
Painful cramps in the feet or lower legs can be another sign of reduced circulation. Muscles require oxygen-rich blood to work properly, and when blood flow is compromised, cramps may occur more often, especially at night. Gentle stretching and regular activity can help, but persistent cramps should be evaluated by a doctor.
5. Slow-Healing Wounds or Sores
A minor cut that lingers for weeks without healing is a major red flag. Elevated blood sugar slows the body’s repair process, leaving wounds prone to infection. Untreated sores may progress into ulcers—open wounds that form due to poor circulation and delayed healing. Regular foot checks and timely wound care can prevent dangerous complications.
6. Changes in Skin Color
Discoloration in the feet, such as dark patches, redness, or a bluish tint, may signal poor blood flow or a skin infection. Inadequate circulation deprives tissues of oxygen, causing visible changes. Noticing these shifts early and consulting a doctor can help prevent further damage.
7. Dry or Cracked Skin
Diabetes often reduces the skin’s ability to retain moisture, leading to dryness, peeling, or cracked heels. Cracks can allow bacteria to enter, creating a risk of infection. Moisturizing daily can help, but avoid applying lotion between the toes since excess moisture there can promote fungal growth.
8. Swelling in the Feet or Ankles
Swelling, or edema, in the feet and ankles may indicate fluid buildup or poor circulation. Diabetes weakens blood vessels, making it harder to move fluids effectively. While mild swelling may improve with elevation, sudden or severe swelling should be evaluated by a healthcare provider, as it could signal a complication.
9. Fungal Infections
People with diabetes are more prone to fungal nail infections. Nails may become yellow, brittle, or thickened. These infections can be difficult to treat and sometimes require prescription medication. Keeping your feet clean, dry, and properly groomed lowers the risk of fungal growth.
10. Foot Deformities
Over time, long-term nerve damage can alter foot structure, leading to deformities such as hammertoes or claw toes. These changes may cause discomfort while walking and increase the chance of pressure sores. Wearing supportive shoes and scheduling regular podiatrist visits can help prevent worsening deformities.
Tips for Protecting Your Feet
Daily care is essential for people with diabetes. Here are some key practices:
-
Inspect feet every day for cuts, blisters, or swelling.
-
Wash and dry feet thoroughly, including between the toes.
-
Moisturize regularly, but not between the toes.
-
Wear comfortable, well-fitting shoes to reduce pressure points.
-
Trim toenails straight across to prevent ingrown nails.
-
Keep blood sugar within a healthy range to protect circulation and nerves.
-
Visit a podiatrist for regular foot examinations.
When to Seek Medical Advice
Ignoring foot symptoms of diabetes can lead to infections, ulcers, and in severe cases, amputation. If you notice any of the signs above, schedule a check-up promptly. With good blood sugar control, daily foot care, and regular monitoring, you can greatly reduce the risk of serious complications.
Protecting your feet begins with awareness and early action. Recognizing changes in your feet may be the first step in taking charge of your health.
News in the same category


10 Healthy Sandwich Dos and Don’ts

Medicinal Health Benefits of Garlic (Raw, Supplement) – Science Based

Why You Should Wash Your Face With Apple Cider Vinegar

If Your Feet Swell It Is a Clear Sign

What Your Feet Are Telling You
6 Health Benefits of Sleeping In a Cold Room and How to Make it Cooler- And Why You May Not Want to Use a Fan
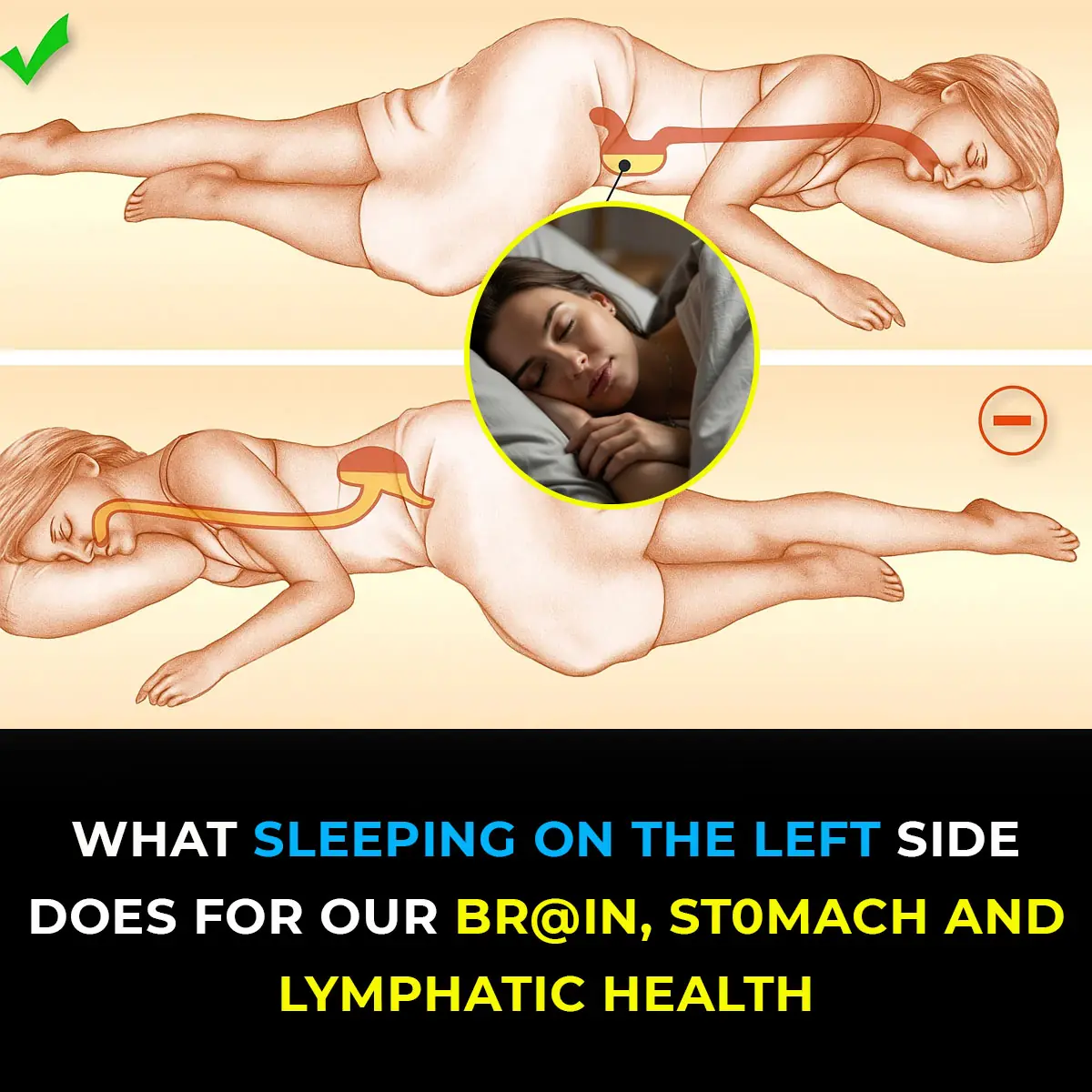
This is what sleeping on the left side does for our brain, stomach & glymphatic health

12 Best Foods To Support Digestive and Gut Health

Study suggests anal cancer is on the rise and reveals who’s most at risk
Wife Complains of a Headache, Sleeps, and Dies Without Husband Knowing: This Type of Headache Requires Immediate Hospitalization!

Shocking Effects of Sleeping Less Than 7 Hours — What Really Happens to Your Body
Getting less than seven hours of sleep might feel harmless, but science shows it can quietly damage your body in ways you don’t expect. From hormonal imbalances to skin problems and even digestive issues, sleep deprivation affects far more than just you

Doctors Explain Why You Should Never Hold Back a Fart
On average, every person passes gas 14 to 23 times per day—it’s a natural part of being human and actually shows that your digestive system is functioning properly.
Scientists Invent Smart Tooth That Grows Into Your Gums And Connects To Nerves Like the Real Thing

Scientists Say This New Stem Cell Treatment Could End Type 1 Diabetes for Good
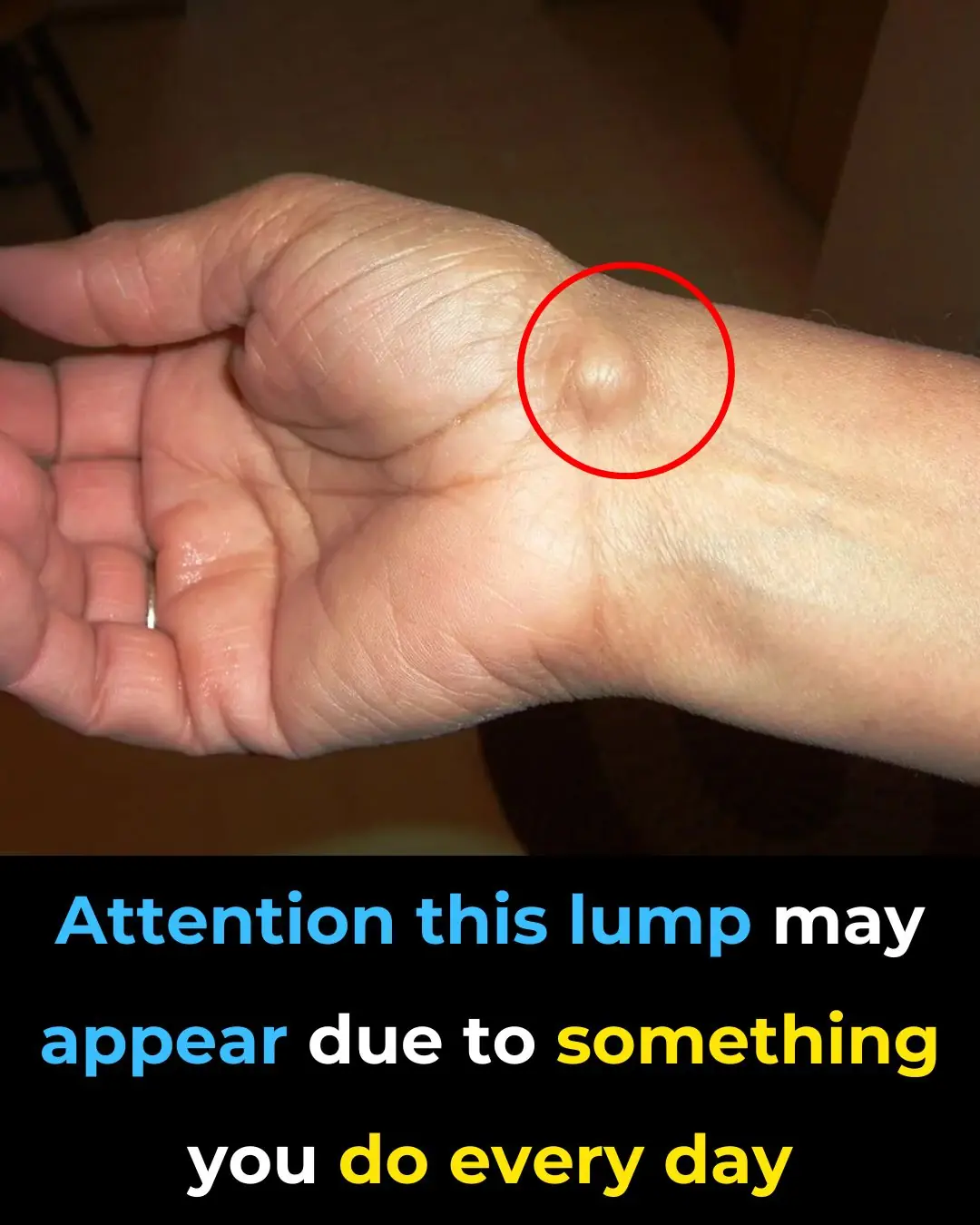
Everyday Habits That Can Cause a This Issue To Your Hands

My Nana’s Homemade Cure for Stubborn Throat Mucus That Works Every Time

Doctors Are Shocked by What Happens When You Eat Chia Seeds First Thing in the Morning
Warning Signs of Poor Blood Circulation That Are Easy to Ignore
News Post

Menopause Symptoms That May Surprise You

10 Healthy Sandwich Dos and Don’ts

Never Ever Say These 4 Things at a Funeral — No Matter the Situation
When it comes to funerals and expressions of sympathy, your words don’t need to be profound or poetic.

🥥 15 Compelling Reasons to Include Coconut Water in Your Daily Routine

🌿 30 Remarkable Benefits of Avocado Leaves

🌿 Natural Collagen Boost: Garlic Remedy for Smoother Skin

✨ Brighten Your Smile Naturally: A Simple DIY Teeth Whitening Remedy
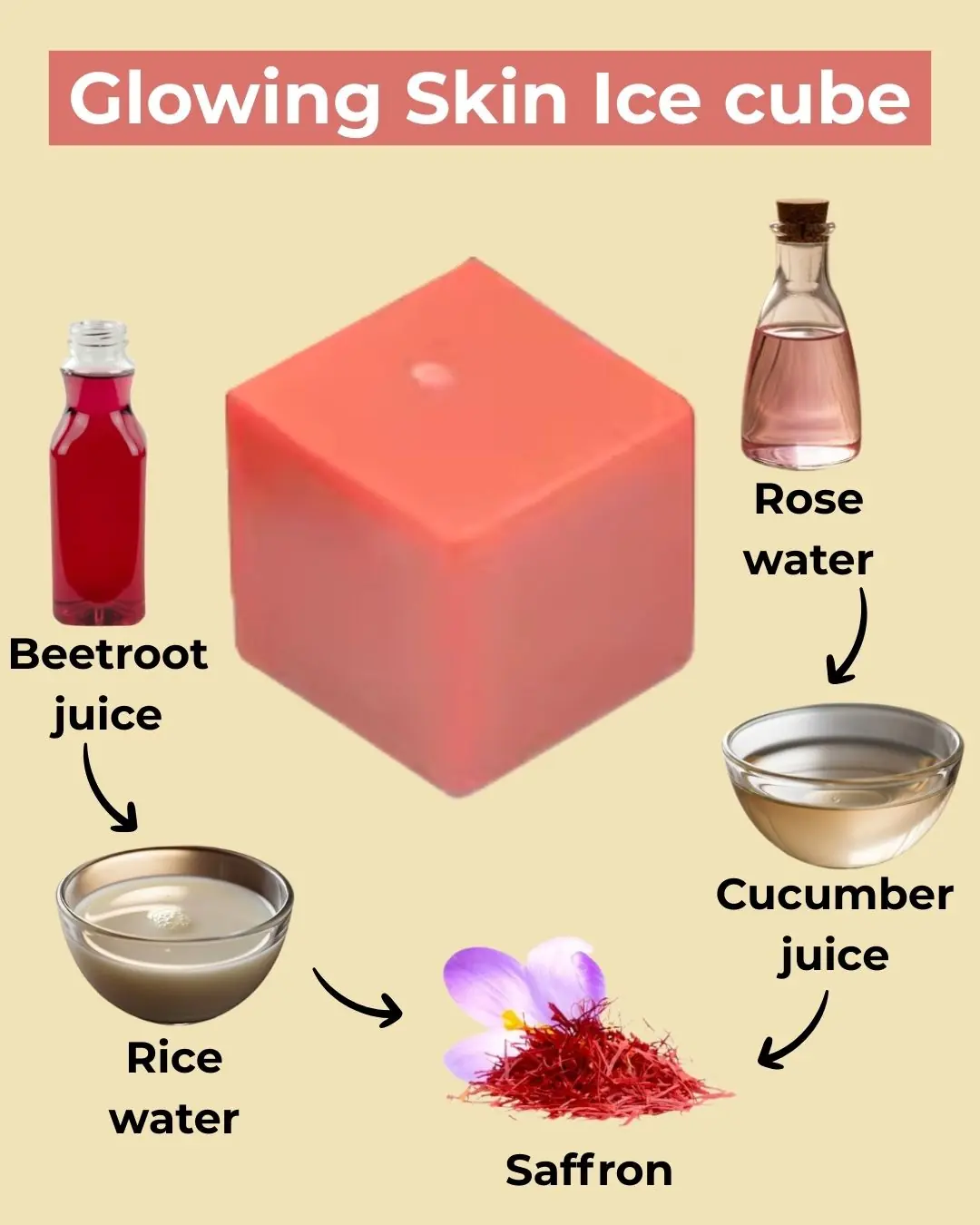
🌟 DIY Collagen Ice Cubes for Radiant Skin

🌿 3 Natural Home Remedies to Remove Skin Tags Safely

Medicinal Health Benefits of Garlic (Raw, Supplement) – Science Based

Why You Should Wash Your Face With Apple Cider Vinegar

If Your Feet Swell It Is a Clear Sign

What Your Feet Are Telling You
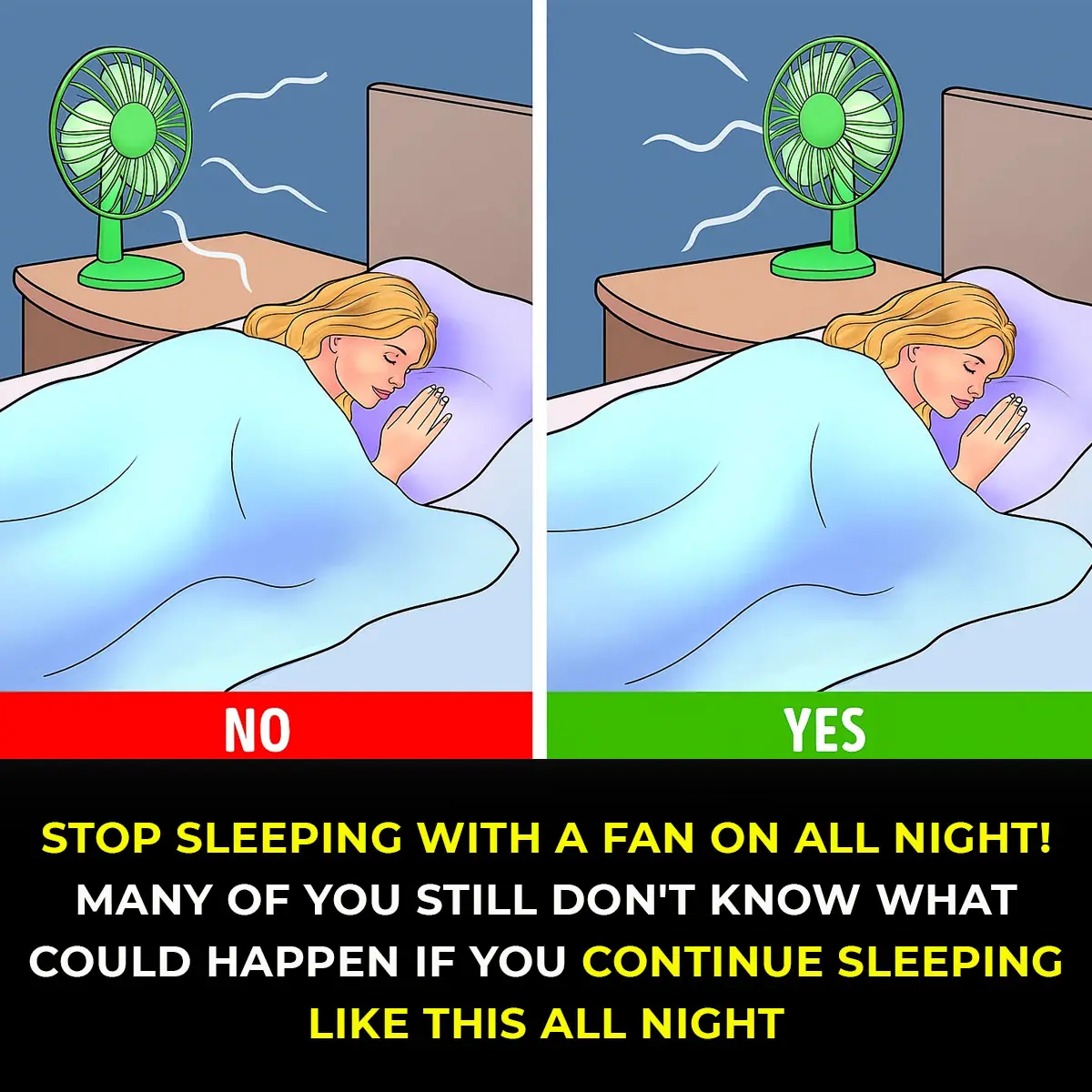
6 Health Benefits of Sleeping In a Cold Room and How to Make it Cooler- And Why You May Not Want to Use a Fan
The Hidden Meaning Behind Leg-crossing — It’s More Than Just Comfort

How To Properly Dispose of Ticks
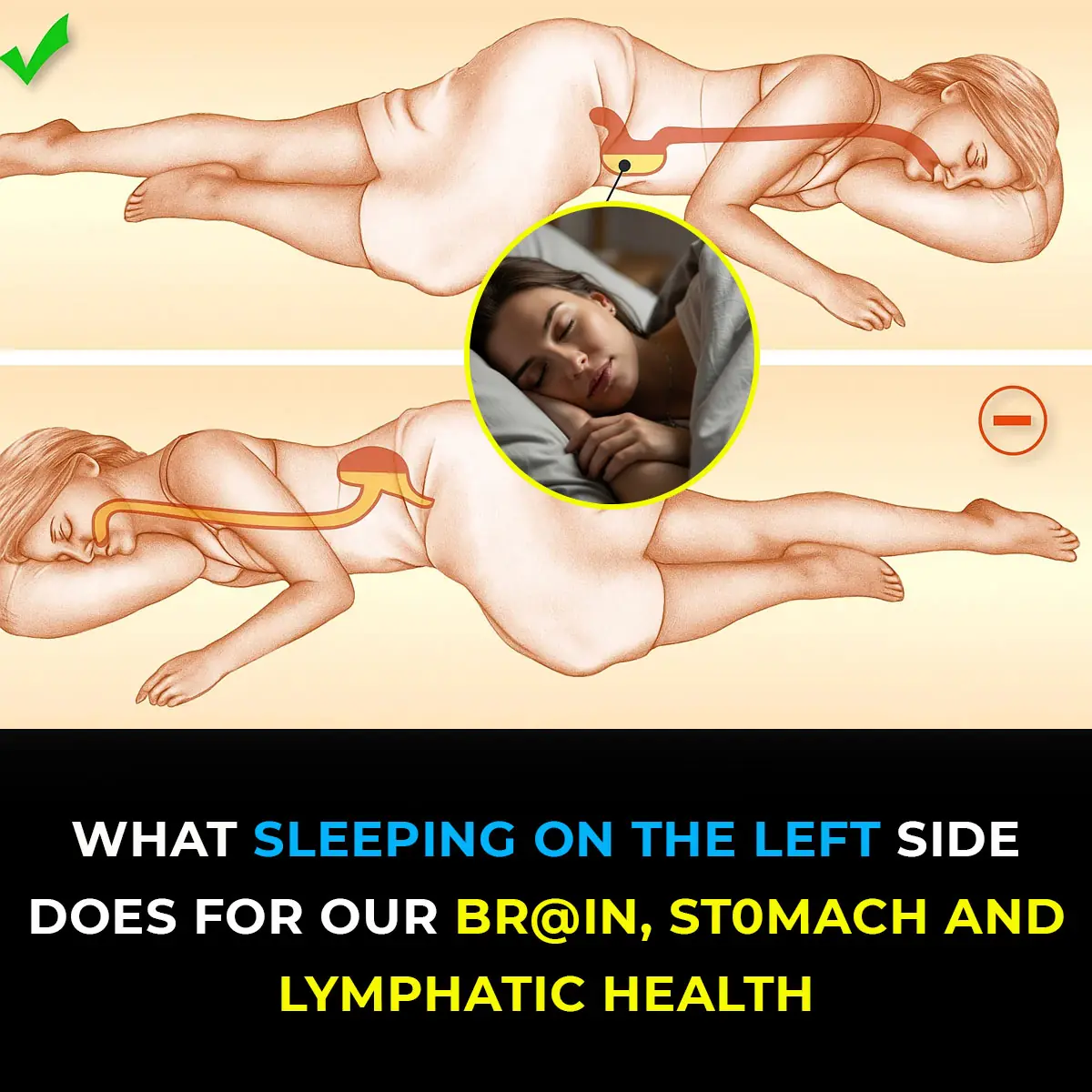
This is what sleeping on the left side does for our brain, stomach & glymphatic health

12 Best Foods To Support Digestive and Gut Health
