
Study suggests anal cancer is on the rise and reveals who’s most at risk

A recent study set to be presented at Digestive Disease Week (DDW) 2025 has drawn attention to a worrying trend: a significant increase in the number of people diagnosed with anal cancer. While this form of cancer is still considered rare, the latest findings suggest that certain groups are experiencing a rapid rise in cases, raising urgent questions about prevention, awareness, and the role of vaccination.
What Is Anal Cancer?
According to the NHS, anal cancer develops in the anus—the opening at the end of the bowel where the digestive tract connects to the outside of the body. Unlike more common cancers such as colorectal or cervical cancer, anal cancer is relatively rare, but its impact can be serious.
The disease can begin in any part of the anal canal. Because symptoms often resemble those of less severe conditions, anal cancer is sometimes overlooked until it has progressed.
Symptoms and Early Warning Signs
Recognizing the signs of anal cancer is crucial, especially since the condition can be misdiagnosed as haemorrhoids or anal fissures. The most frequently reported symptoms include:
-
Bleeding from the rectum or anus
-
Persistent itching or pain around the anus
-
Lumps inside or around the bottom
-
Unusual discharge of mucus
-
Changes in bowel habits, such as difficulty controlling movements
Since these symptoms can mimic other conditions, awareness among both patients and health professionals is essential for earlier detection.
The Study’s Key Findings
The study, conducted between 2017 and 2021, highlights concerning patterns.
“Rates of anal cancer are rising fastest among white and Hispanic women over 65 — groups not traditionally considered high risk,” said lead author Ashley Robinson, MD, a second-year internal medicine resident at Advocate Lutheran General Hospital.
Overall, anal cancer diagnoses increased by:
-
2.9% in women
-
1.6% in men
When broken down further, the highest increase was seen in white women over 65, with cases rising 4.43%. The second most affected group was Hispanic women of the same age range, with an increase of 1.7%.
These findings suggest that shifting demographic factors and gaps in vaccination coverage may be influencing the trend.
HPV and Its Role in Anal Cancer
Most cases of anal cancer are caused by infection with the human papillomavirus (HPV). HPV is one of the most common viruses worldwide and is typically spread through skin-to-skin contact, often during sexual activity.
Dr. Robinson emphasized that vaccination history plays a significant role in today’s rising rates:
“While the exact reasons behind this trend remain unclear, most older women were beyond the recommended age for human papillomavirus vaccination when it first became widely available.”
The Importance of HPV Vaccination
The HPV vaccine has proven highly effective in reducing the risk of HPV infection and related cancers, including anal, cervical, and throat cancers.
In the UK, the vaccine is routinely offered to:
-
Children aged 12 to 13
-
Adults over 25 who missed their earlier vaccination window
Dr. Robinson stressed the urgency of maintaining strong vaccination programs:
“It’s crucial that we promote HPV vaccination as a key tool for preventing anal cancer, while also keeping health care providers informed as screening guidelines evolve. These findings highlight specific patient groups who may benefit from targeted screening for anal HPV and anal cancer.”
Why Are Older Women More Affected?
The sharp rise among women over 65, particularly those who are white or Hispanic, reflects a generational gap. When the HPV vaccine first became widely available, many of today’s older adults had already aged out of the eligibility group. As a result, they carry a higher lifetime risk of HPV-related cancers.
Additionally, natural changes in the immune system with age may make it more difficult to fight off persistent HPV infections, leading to an increased risk of cancer development.
Current Screening Limitations
Unlike cervical cancer, where screening programs such as Pap smears are routine, anal cancer does not yet have a national screening program.
As noted by Cancer Research UK, this is largely because no test has been developed that can reliably detect anal cancer at its earliest stages. This makes prevention and symptom awareness even more critical.
Reducing Your Risk of Anal Cancer
While not all cases can be prevented, several steps may help lower risk:
-
Get Vaccinated
The HPV vaccine is the most effective way to reduce the likelihood of infection. Even if someone missed the vaccine in adolescence, catch-up programs for older adults are available in many countries. -
Practice Safer Sex
Since HPV spreads primarily through sexual contact, using protection and limiting exposure to multiple partners can help reduce risk. -
Quit Smoking
Smoking is known to weaken the immune system and has been linked to higher risks of HPV-related cancers. -
Pay Attention to Symptoms
Unexplained bleeding, pain, or lumps should never be ignored. Seeking medical advice early may help with faster diagnosis and treatment. -
Maintain Regular Health Checkups
Especially for people over 65 or those in identified risk groups, routine checkups and open conversations with healthcare providers are essential.
The Bigger Picture: Prevention Through Awareness
Anal cancer may still be considered rare, but the steady rise in cases—especially among older women—shows that it can no longer be dismissed as a low-risk condition. Awareness campaigns, wider access to HPV vaccination, and updated screening guidelines will be crucial in addressing this growing health issue.
While scientists continue to investigate the exact reasons behind these demographic shifts, one thing remains clear: prevention through vaccination and education is our strongest defense.
Conclusion
The latest study presented at DDW 2025 underscores an important message: anal cancer rates are climbing in groups previously thought to be at lower risk, particularly white and Hispanic women over 65.
With no early screening tests currently available, prevention becomes the key. Expanding HPV vaccination coverage, educating both patients and healthcare providers, and encouraging prompt evaluation of symptoms are critical steps toward reducing the burden of this disease.
By staying informed and proactive, individuals and healthcare systems alike can help ensure that anal cancer is detected earlier, treated more effectively, and—most importantly—prevented whenever possible.
News in the same category


10 Healthy Sandwich Dos and Don’ts

Medicinal Health Benefits of Garlic (Raw, Supplement) – Science Based

Why You Should Wash Your Face With Apple Cider Vinegar

If Your Feet Swell It Is a Clear Sign

What Your Feet Are Telling You
6 Health Benefits of Sleeping In a Cold Room and How to Make it Cooler- And Why You May Not Want to Use a Fan

10 Symptoms of Diabetes That May Show Up In Your Feet
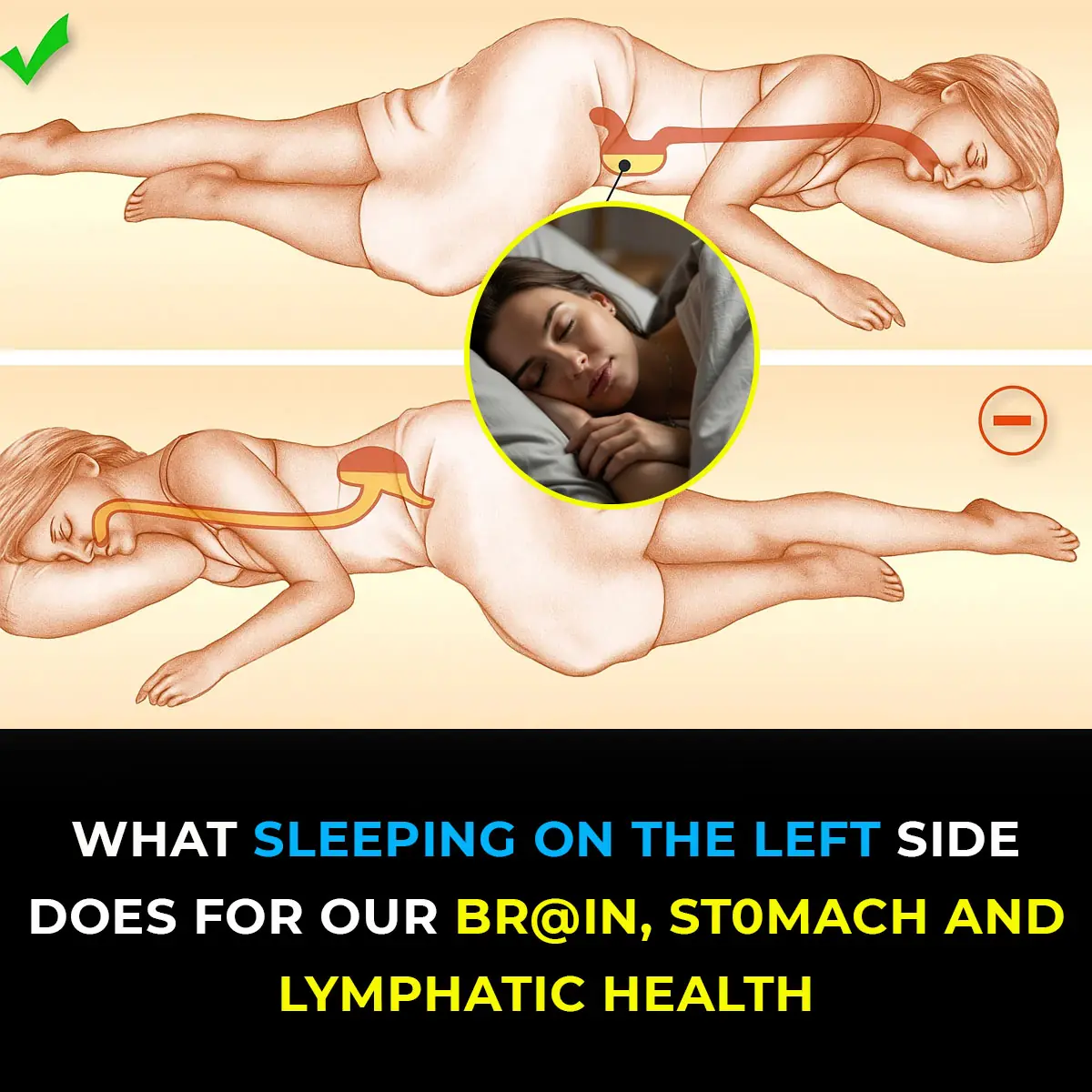
This is what sleeping on the left side does for our brain, stomach & glymphatic health

12 Best Foods To Support Digestive and Gut Health
Wife Complains of a Headache, Sleeps, and Dies Without Husband Knowing: This Type of Headache Requires Immediate Hospitalization!

Shocking Effects of Sleeping Less Than 7 Hours — What Really Happens to Your Body
Getting less than seven hours of sleep might feel harmless, but science shows it can quietly damage your body in ways you don’t expect. From hormonal imbalances to skin problems and even digestive issues, sleep deprivation affects far more than just you

Doctors Explain Why You Should Never Hold Back a Fart
On average, every person passes gas 14 to 23 times per day—it’s a natural part of being human and actually shows that your digestive system is functioning properly.
Scientists Invent Smart Tooth That Grows Into Your Gums And Connects To Nerves Like the Real Thing

Scientists Say This New Stem Cell Treatment Could End Type 1 Diabetes for Good
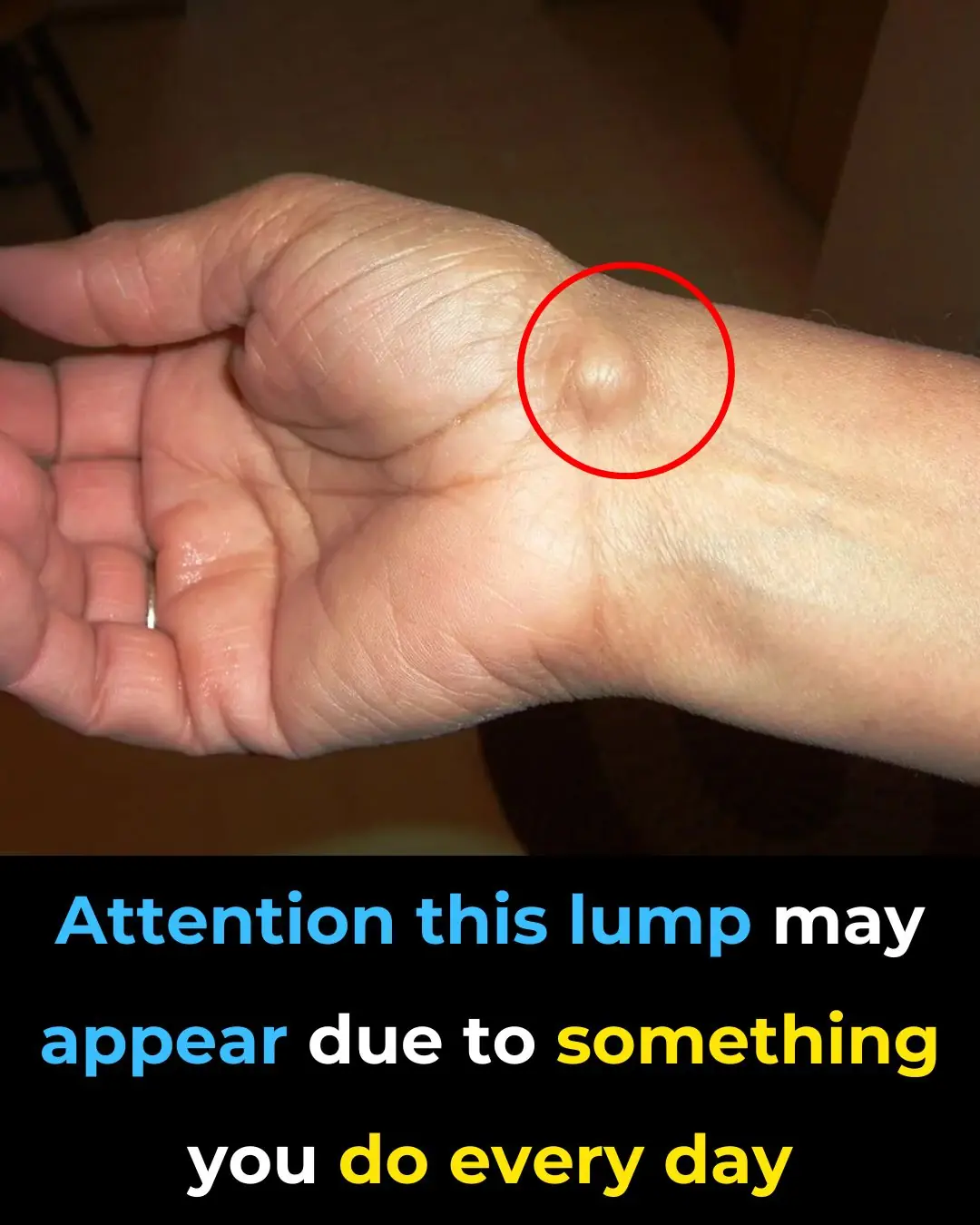
Everyday Habits That Can Cause a This Issue To Your Hands

My Nana’s Homemade Cure for Stubborn Throat Mucus That Works Every Time

Doctors Are Shocked by What Happens When You Eat Chia Seeds First Thing in the Morning
Warning Signs of Poor Blood Circulation That Are Easy to Ignore
News Post

Menopause Symptoms That May Surprise You

10 Healthy Sandwich Dos and Don’ts

Never Ever Say These 4 Things at a Funeral — No Matter the Situation
When it comes to funerals and expressions of sympathy, your words don’t need to be profound or poetic.

🥥 15 Compelling Reasons to Include Coconut Water in Your Daily Routine

🌿 30 Remarkable Benefits of Avocado Leaves

🌿 Natural Collagen Boost: Garlic Remedy for Smoother Skin

✨ Brighten Your Smile Naturally: A Simple DIY Teeth Whitening Remedy
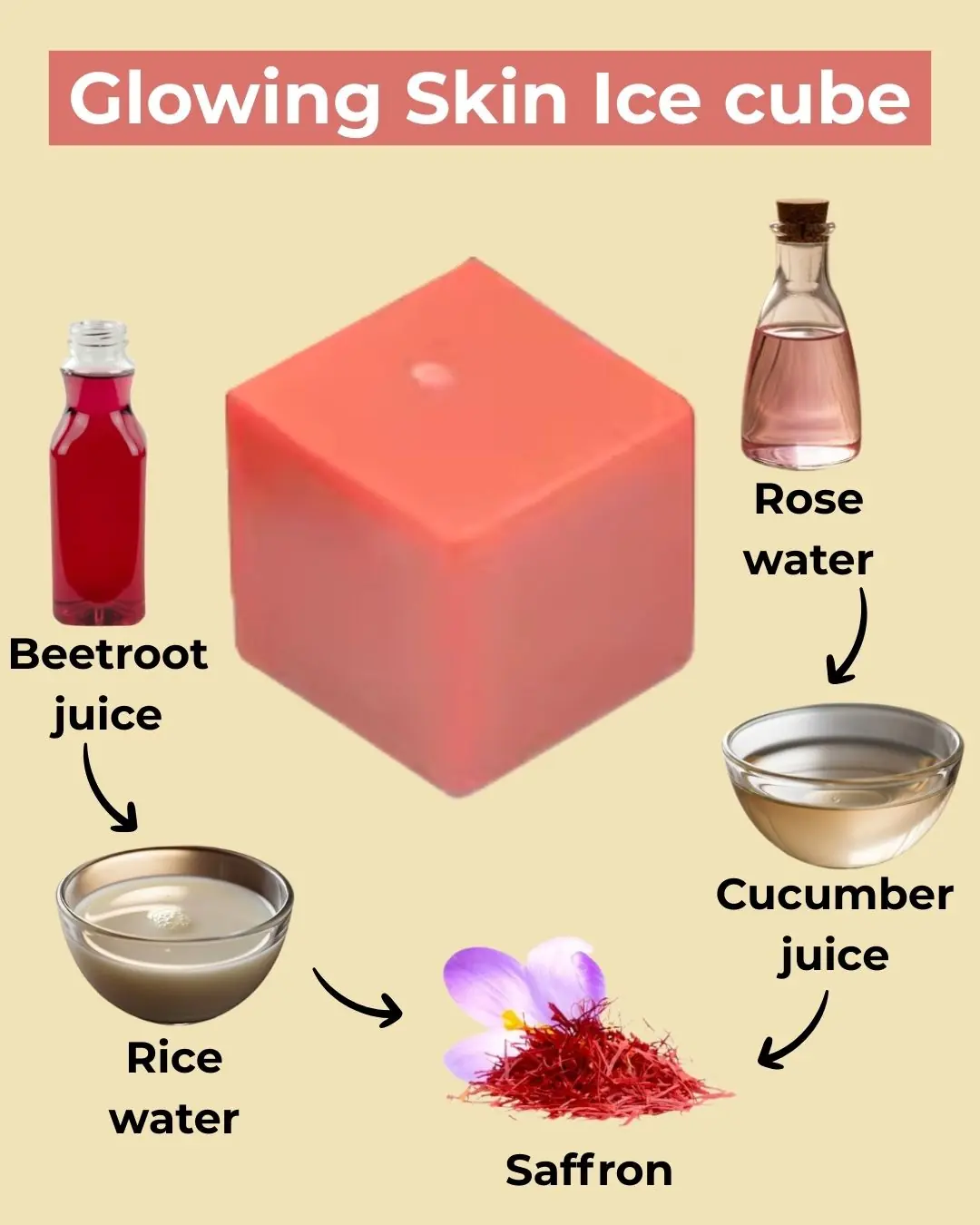
🌟 DIY Collagen Ice Cubes for Radiant Skin

🌿 3 Natural Home Remedies to Remove Skin Tags Safely

Medicinal Health Benefits of Garlic (Raw, Supplement) – Science Based

Why You Should Wash Your Face With Apple Cider Vinegar

If Your Feet Swell It Is a Clear Sign

What Your Feet Are Telling You
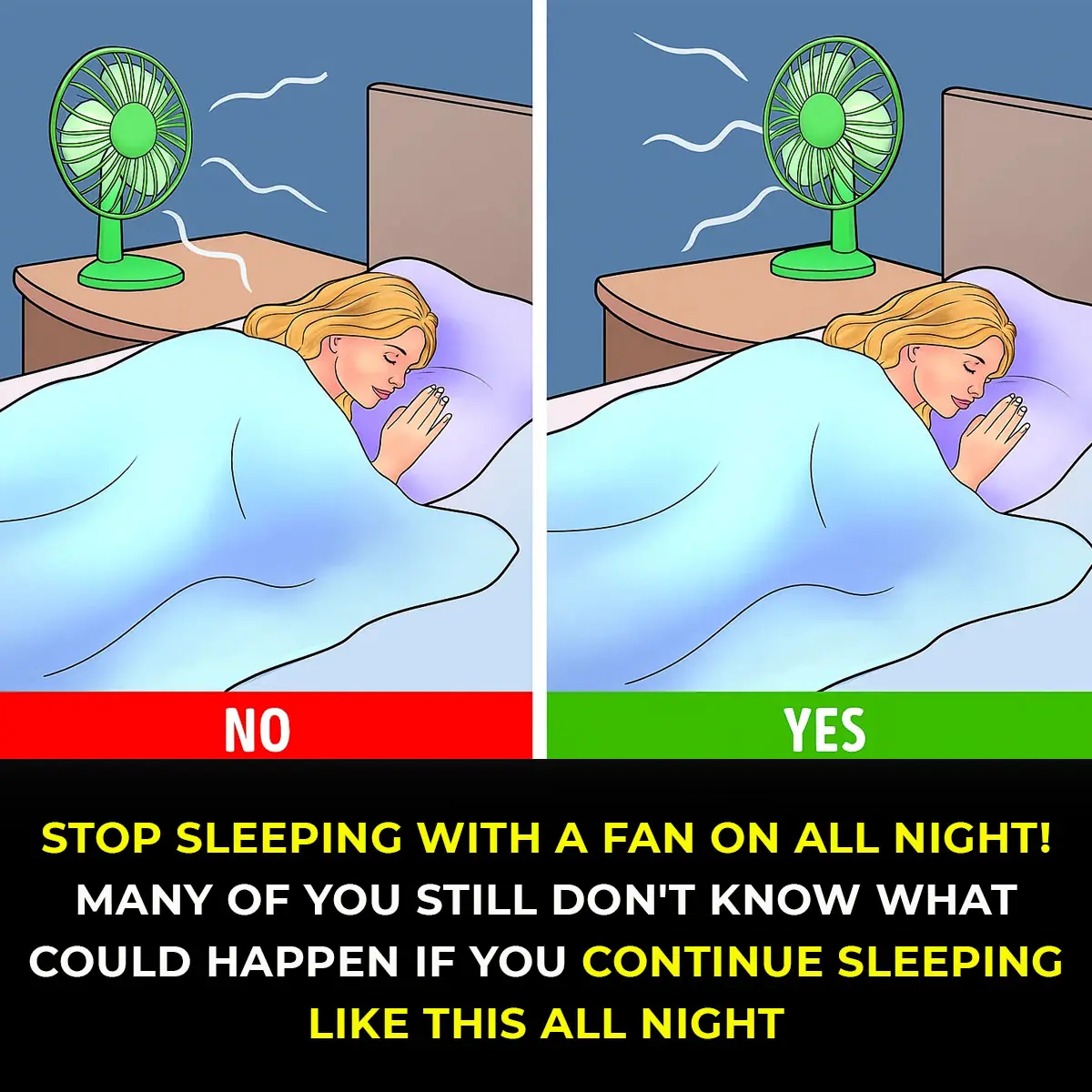
6 Health Benefits of Sleeping In a Cold Room and How to Make it Cooler- And Why You May Not Want to Use a Fan
The Hidden Meaning Behind Leg-crossing — It’s More Than Just Comfort

10 Symptoms of Diabetes That May Show Up In Your Feet

How To Properly Dispose of Ticks
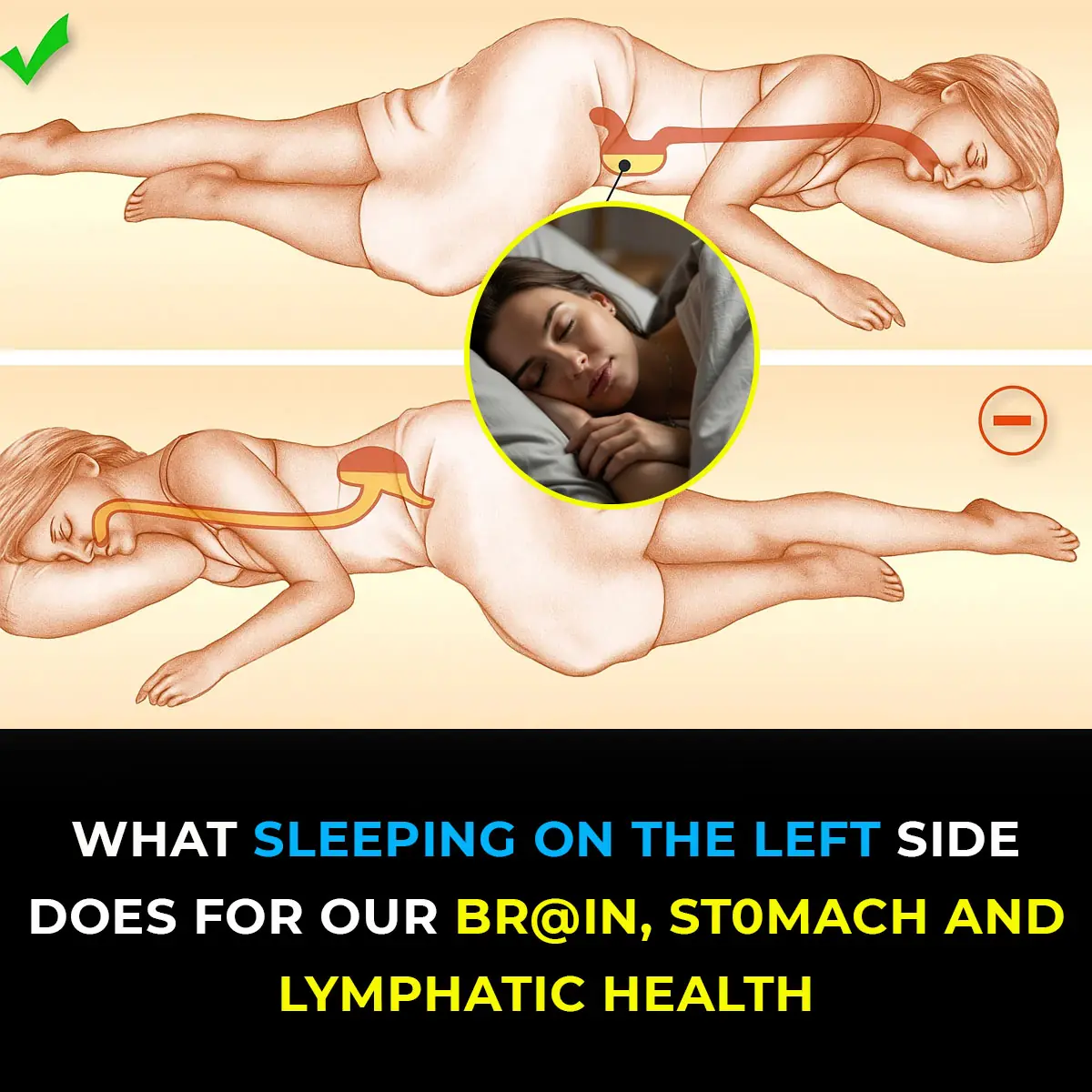
This is what sleeping on the left side does for our brain, stomach & glymphatic health
