
13 Early Warning Signs of Lupus You Need to Know (And What To Do The Moment You See Them)
For many people, lupus feels like a distant, almost unreal illness—something they might hear about but never expect to experience. Yet for an estimated 1.5 million Americans, this autoimmune disease is a daily reality that affects every aspect of their lives. Although lupus currently has no known cure, advances in medicine have provided numerous treatments to help manage symptoms and flare-ups. Strikingly, nine out of ten people diagnosed with lupus are women, and symptoms most often appear between the ages of 15 and 45.
What Is Lupus?
Lupus is an autoimmune disease, meaning the body’s immune system mistakenly attacks its own tissues, perceiving them as harmful invaders. This misguided immune response leads to widespread inflammation and tissue damage, which can affect various organs and systems throughout the body.
The exact cause of lupus remains unclear, but researchers believe it results from a combination of genetic, hormonal, environmental, and immune system factors. Certain medications and hormonal imbalances can also trigger or worsen the disease.
There are several forms of lupus, but the two most common types are:
-
Discoid Lupus Erythematosus (DLE): Primarily affects areas of skin exposed to sunlight, causing red, scaly lesions or discoloration.
-
Systemic Lupus Erythematosus (SLE): The most serious and complex form, which can damage internal organs such as the heart, lungs, kidneys, and brain.
Systemic lupus can lead to inflammation of connective tissues in the joints and muscles, as well as the membranes surrounding vital organs. In severe cases, it may result in kidney failure, heart inflammation, or neurological damage. Because lupus has no definitive cure, patients must focus on managing symptoms, preventing flare-ups, and protecting their organs through consistent medical care and lifestyle adjustments.
Triggers and Treatment Options
Lupus symptoms can worsen in response to certain triggers. Common flare-up triggers include sunlight, infections, and some medications, while stress, extreme temperature changes, and inflammatory foods can make symptoms more severe.
Treatment often involves a combination of anti-inflammatory drugs, immune suppressants, corticosteroids, and even chemotherapy-based medications to reduce immune system overactivity. Patients are typically monitored by a multidisciplinary medical team, including rheumatologists, cardiologists, nephrologists, neurologists, and gastroenterologists, to prevent and manage organ complications.
In addition, many patients are prescribed diuretics, blood pressure medications, anticonvulsants, antibiotics, or bone-strengthening drugs to manage side effects or related conditions.
Some individuals also explore natural or complementary treatments, such as consuming anti-inflammatory foods, taking omega-3 fatty acids (fish oil), and maintaining healthy vitamin D levels from sunlight or supplements. Although these options cannot replace medical treatment, they may help reduce inflammation and improve overall wellbeing.
Common Lupus-Related Complications
Lupus often coexists with or increases the risk of other autoimmune and inflammatory conditions, such as:
-
Rheumatoid arthritis
-
Reactive arthritis
-
Celiac disease
-
Pernicious anemia
-
Vitiligo
-
Scleroderma
-
Psoriasis
-
Inflammatory bowel disease
-
Hashimoto’s thyroiditis
-
Addison’s disease
-
Graves’ disease
-
Sjögren’s syndrome
-
Type 1 diabetes
-
Other immune disorders
What It’s Like to Live with Lupus
“It’s a disability that you cannot describe because the whole thing about lupus is it’s so unpredictable,” said Mallory Dixon, 29, in an interview with Medical Daily. For many patients, lupus feels like living with an unseen enemy—some days are manageable, while others bring extreme fatigue and pain that make even simple tasks impossible.
The unpredictable nature of lupus makes it difficult for doctors to diagnose and treat. Many patients endure years of misdiagnoses because lupus mimics other illnesses such as arthritis, fibromyalgia, or chronic fatigue syndrome. Dixon, for instance, was first diagnosed with rheumatoid arthritis at age 17, but her symptoms continued to worsen in ways her doctors couldn’t explain. At one point, her condition was even dismissed as psychological.
It wasn’t until six years later that she finally received the correct lupus diagnosis. Unfortunately, just two years after that, her disease led to multiple organ failure, requiring resuscitation after she was declared clinically dead. Dixon spent 86 days in the hospital, much of that time in a coma. She required chemotherapy, dialysis, and long-term respiratory support as lupus severely damaged her kidneys.
Despite these challenges, Dixon has turned her experience into advocacy—educating women about lupus so they can recognize symptoms early and seek medical care before serious organ damage occurs. “With early prevention,” she says, “we can keep lupus from spreading to organs like the kidneys or, in some cases, the heart or brain.”
Unfortunately, many lupus patients never receive adequate emotional or medical support, particularly during the early stages of the disease. Because the illness can be invisible, family members, friends, and even healthcare providers sometimes fail to believe the patient’s pain is real. As registered nurse Stothers explains, “Some people look completely normal, yet they feel awful. Doing even the smallest task can be impossible.”
The isolation that accompanies this invisible illness can be devastating. Many sufferers struggle with anxiety and depression, not only from chronic pain and fatigue but also from feeling misunderstood. And because lupus doesn’t always run in families, patients like Dixon often have no known genetic clues to rely on.
Recognizing the Signs of Lupus
If lupus or other autoimmune diseases run in your family—or if you’ve experienced unexplained health problems—it’s important to be aware of potential warning signs, including:
-
Pain or swelling in joints
-
Persistent muscle aches
-
Fevers with no clear cause
-
Red facial rashes (often in a butterfly pattern)
-
Chest pain when breathing deeply
-
Hair loss
-
Pale or purplish fingers or toes (Raynaud’s phenomenon)
-
Sensitivity to sunlight
-
Swelling in legs or around the eyes
-
Mouth ulcers
-
Enlarged lymph nodes
-
Severe fatigue
-
Anemia (low red blood cell count)
-
Headaches, dizziness, or confusion
-
Mood changes, sadness, or depression
-
Seizures
If you notice several of these symptoms, especially alongside a family history of autoimmune disease, consult your doctor for testing. Early diagnosis and ongoing management can make a significant difference in preventing serious complications and improving quality of life.
A Final Thought
Living with lupus requires resilience, patience, and hope. While there may be no cure yet, continuous research is paving the way for better treatments and, ultimately, a deeper understanding of the disease. For now, awareness, empathy, and early intervention remain the most powerful tools in helping lupus patients live full and meaningful lives.
News in the same category


Stroke and Heart Attack Often “Target” These People: 7 Things You Must Do Before It’s Too Late

Doctor Finally Explains the Secret Effect of Eating One Banana a Day

THE NATURAL FIX THAT FINALLY GOT RID OF MY SWOLLEN FEET

10 signs you're not drinking enough water
Drinking Water the Right Way

7 best foods to rebuild your muscle strength after 50

Texas Doctor Reveals A “Miracle Mineral” That Soothes Nerve Pain

Don’t ignore your legs: the surprising early signs of pancreatic cancer

Foods Adding Inches To Your Waistline
This Is What Science Says About Eating a Banana for Breakfast
5 Early Signs of Poor Circulation (and How to Boost Blood Flow)

How Cancer Travels Through the Lymphatic System—and Ways to Keep It Strong
How to Make Alkaline Water to Fight Fatigue, Digestive Issues, and Disease

Your Legs Have a “Second Heart” — And One Simple Move Can Reactivate It Fast

A neurosurgeon says your legs could predict dementia years before memory loss

Simple Homemade Cough Syrup Removes Phlegm From The Lungs
The B vitamin solution: lower blood pressure when medications fail
The #1 habit that’s destroying muscle in older adults—are you doing this?
News Post

Cut up your old jeans instead of junking them. Here are 10 ways to repurpose them

Put raw chicken drumsticks in a slow cooker with these 3 ingredients. You’ll want it every night.

Easy Clove Cultivation: From Seed to Spice

7 Benefits and Uses of Castor Oil
Zachary Levi dishes on being ‘graylisted’ by Hollywood for his beliefs
Inside Gabby Logan’s marriage to husband Kenny Logan – sex-less marriage; affair allegations; wedding day disaster

Concerns for Lisa Snowdon as she admits ‘a few things need investigating’ following scan

Davina McCall reveals she’s been diagnosed with breast cancer in emotional video message

The Amazing 7 Benefits of Cucumber Peels — You’ll Never Throw Them Away Again!

My Nana’s 4-Minute, Zero-Work Hack to Freshen Carpets
Nana’s Timeless Jewelry Cleaning Trick That Actually Works

My nana taught me this hack to relieve joint pain in 5 mins with 0 work. Here’s how it works

10 Foods You Should Never Cook in Aluminum Foil — And Why It Could Be Dangerous

What Does This Little Mark On The Ear Mean
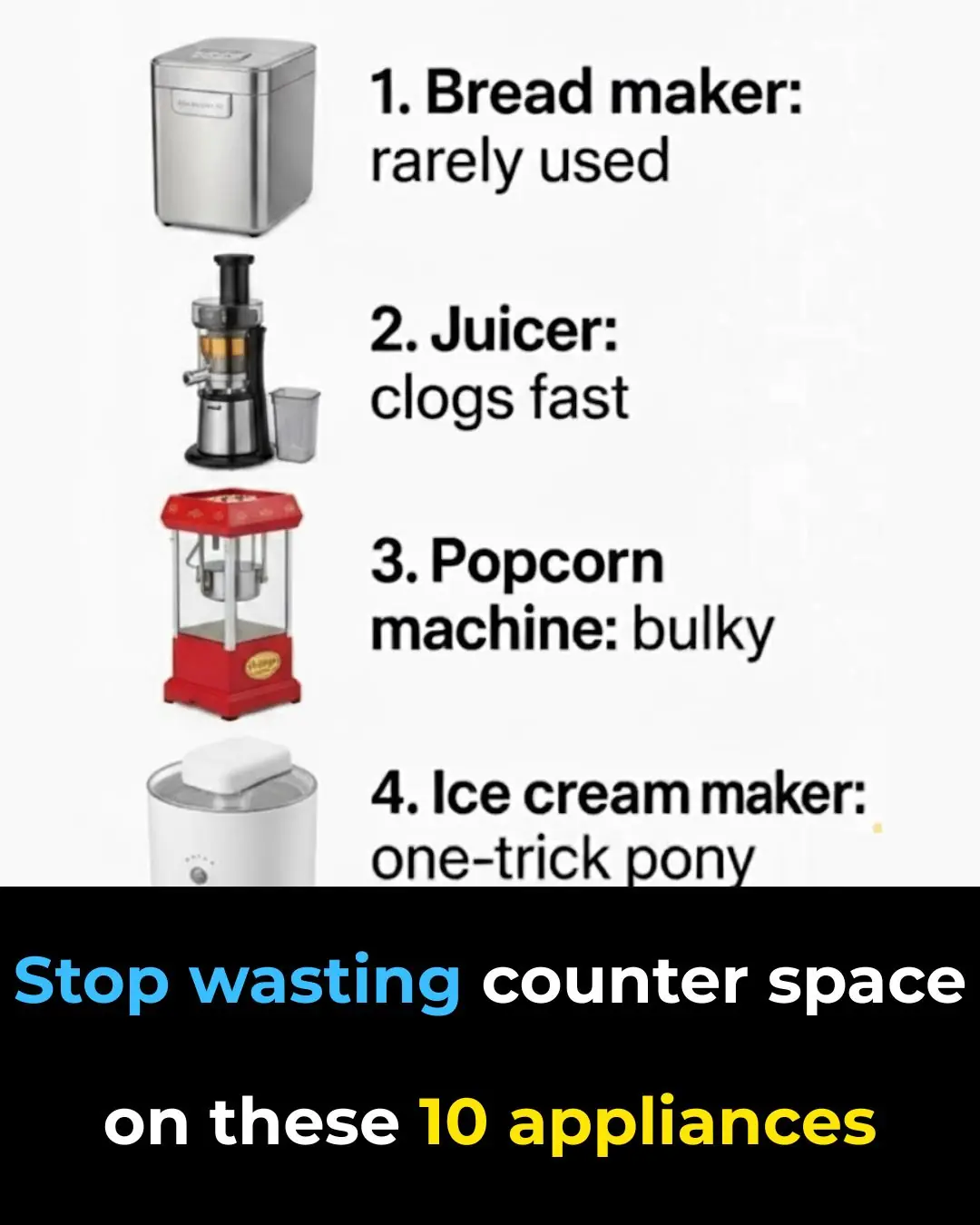
Stop Wasting Counter Space on These 10 Kitchen Appliances
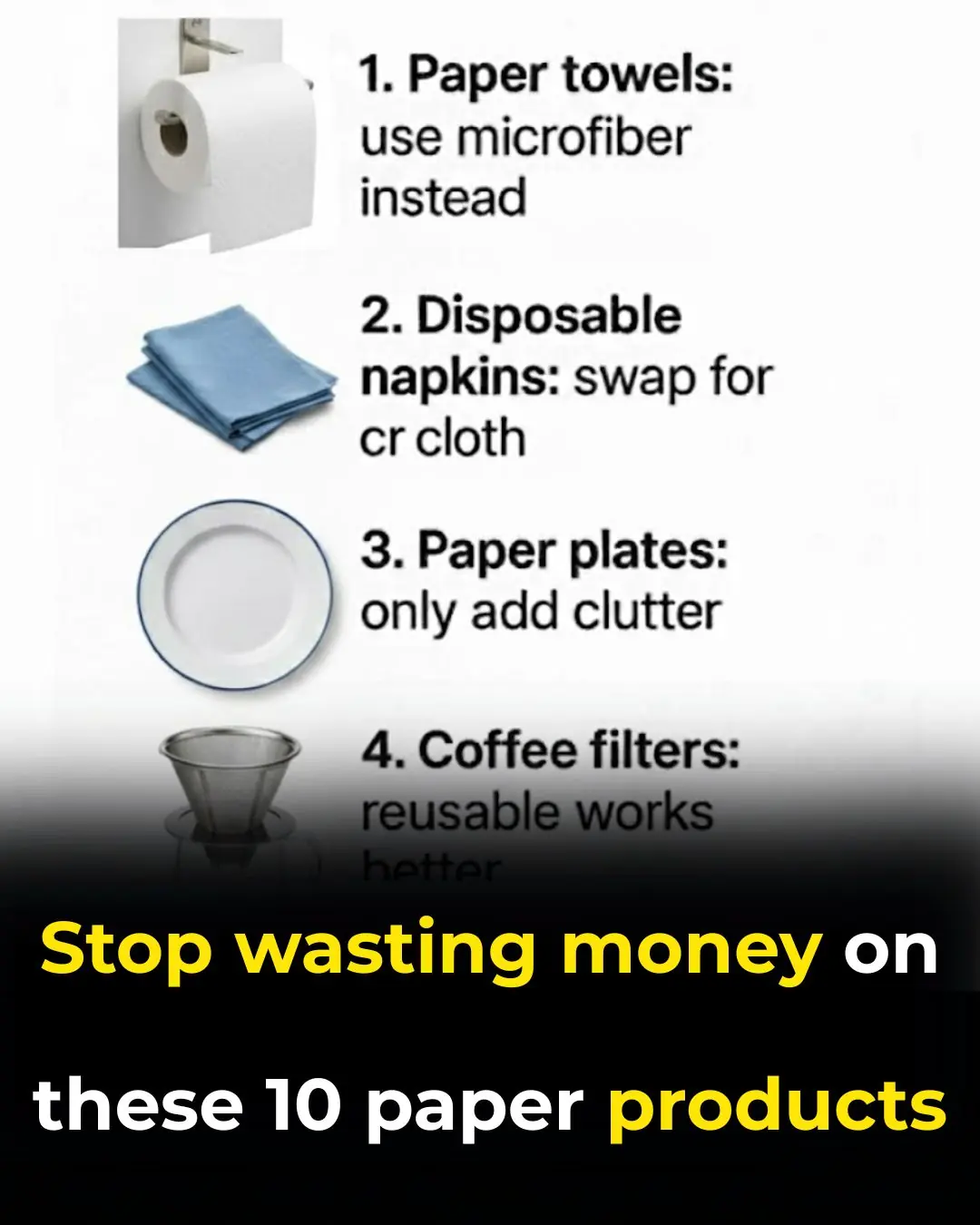
Stop Wasting Money on These 10 Paper Products

Keyless Cars: What Every Driver Needs to Know

1 Minute to “Check Your Kidneys” at Home — See Instantly If They’re Strong or Weak

10 Controversial Winter Watering Tricks That Actually Work
