Bariatric Surgery or GLP-1 Receptor Agonists? Long-Term Effects on Fat Loss and Body Composition

Introduction
Obesity is a chronic, relapsing disease that significantly increases the risk of cardiovascular disease, type 2 diabetes, certain cancers, and reduced quality of life. In recent years, two treatment strategies have emerged as particularly effective for achieving substantial and sustained weight loss: bariatric surgery and pharmacological therapy with glucagon-like peptide-1 (GLP-1) receptor agonists. While both approaches have demonstrated impressive reductions in body weight, growing evidence suggests that the quality of weight loss—specifically changes in fat mass versus fat-free mass—may differ meaningfully between the two.
Recent studies following patients for up to two years indicate that both bariatric surgery and GLP-1 receptor agonists lead to significant reductions in fat mass. However, differences emerge when examining body composition more closely. Notably, individuals undergoing bariatric surgery tend to maintain a higher ratio of fat-free mass to fat mass over time, which may have important metabolic and functional implications.
Understanding Fat Mass and Fat-Free Mass
Weight loss is often discussed as a single number on the scale, but body composition tells a more nuanced story. Fat mass includes all adipose tissue in the body, while fat-free mass encompasses muscle, bone, organs, and body water. Preserving fat-free mass—particularly skeletal muscle—is critical because it supports:
-
Basal metabolic rate
-
Physical strength and mobility
-
Insulin sensitivity
-
Long-term weight maintenance
Excessive loss of fat-free mass during weight reduction can contribute to metabolic slowdown, frailty, and weight regain. Therefore, effective obesity treatment should aim not only to reduce fat mass but also to preserve as much lean tissue as possible.
Bariatric Surgery: Profound and Durable Changes
Bariatric surgery, including procedures such as sleeve gastrectomy and Roux-en-Y gastric bypass, remains the most effective intervention for severe obesity. These procedures promote weight loss through a combination of mechanical restriction, hormonal changes, and altered gut signaling.
Over a two-year follow-up period, patients who undergo bariatric surgery typically experience:
-
Large and rapid reductions in total body weight
-
Significant and sustained decreases in fat mass
-
Some loss of fat-free mass, particularly during the first year
Importantly, despite the reduction in lean mass, surgical patients often maintain a higher fat-free mass–to–fat mass ratio compared with those treated with medication alone. This suggests that the proportion of weight lost as fat is relatively greater after surgery, which may help explain the durable metabolic benefits observed in surgical patients, including long-term diabetes remission and improved cardiovascular outcomes.
GLP-1 Receptor Agonists: A Pharmacologic Breakthrough
GLP-1 receptor agonists, such as semaglutide and tirzepatide, have revolutionized medical obesity treatment. These agents work by:
-
Reducing appetite and food intake
-
Slowing gastric emptying
-
Enhancing insulin secretion and glucose control
Clinical trials and real-world data show that GLP-1 receptor agonists can produce substantial fat loss over two years, approaching levels previously achievable only with surgery in some patients. However, weight loss with GLP-1 therapy is also associated with reductions in fat-free mass.
Unlike bariatric surgery, GLP-1 receptor agonists do not directly alter gastrointestinal anatomy. As a result, changes in muscle mass may be more closely linked to reduced caloric intake and insufficient protein consumption or resistance training during treatment. Over time, this can lead to a lower fat-free mass–to–fat mass ratio, especially if lifestyle interventions are not optimized.
Comparing Long-Term Body Composition Outcomes
When comparing the two interventions over a two-year period, several key differences emerge:
-
Fat mass reduction: Both bariatric surgery and GLP-1 receptor agonists produce significant and sustained fat loss.
-
Fat-free mass loss: Both approaches are associated with some degree of lean mass reduction.
-
Body composition quality: Bariatric surgery patients tend to preserve a higher proportion of fat-free mass relative to fat mass throughout follow-up.
This distinction is clinically important. A higher fat-free mass–to–fat mass ratio is associated with better metabolic health, improved physical function, and potentially lower long-term mortality risk.
Clinical Implications and Patient Selection
Choosing between bariatric surgery and GLP-1 receptor agonist therapy is not a one-size-fits-all decision. Factors influencing treatment choice include:
-
Degree of obesity and presence of comorbidities
-
Patient preference and willingness to undergo surgery
-
Access, cost, and long-term adherence
-
Ability to engage in lifestyle interventions such as resistance training
For some patients, GLP-1 receptor agonists may serve as a bridge to surgery or as a long-term alternative. For others, surgery may offer superior durability and body composition benefits, particularly in individuals with severe obesity or poorly controlled metabolic disease.
Conclusion
Both bariatric surgery and GLP-1 receptor agonists represent powerful tools in the management of obesity, offering sustained fat loss over at least two years of follow-up. While both interventions are associated with reductions in fat-free mass, bariatric surgery appears to preserve a more favorable balance between lean tissue and fat mass over time.
As obesity treatment continues to evolve, future strategies may increasingly focus on combining pharmacotherapy, surgery, nutrition, and resistance exercise to maximize fat loss while preserving muscle. Ultimately, individualized treatment plans that consider not just weight loss, but body composition and long-term metabolic health, will provide the greatest benefit for patients living with obesity.
News in the same category


Sunlight at Work Beats Artificial Light for Glucose Control in Type 2 Diabetes

If You Have Fig Leaves, You Have Gold—and You Didn’t Even Know It

It’s surprising how unclear the link between chicken color and quality still is for many people
🤧 Constant Phlegm in Throat? The Real Causes (and How to Actually Get Rid of It)

Why Daily Showers After 65 May Do More Harm Than Good
Scientists Discover Alarming Substance in Human Blood, Raising Serious Concerns
7 easy ways to quickly unclog your lymph nodes to reduce swelling and flush out toxins

What Really Happens When You Eat a Banana Before Bed

Natural Ways to Relieve Cough and Chest Congestion
People whose mouths feel dry when sleeping at night need to know these 8 reasons

Why Eating More Processed Meat Increases Your Risk for Serious Health Problems
That detail isn’t innocent… and few people know it
Doctor Reveals That Eating Guava Can Cause Powerful Changes in Your Body
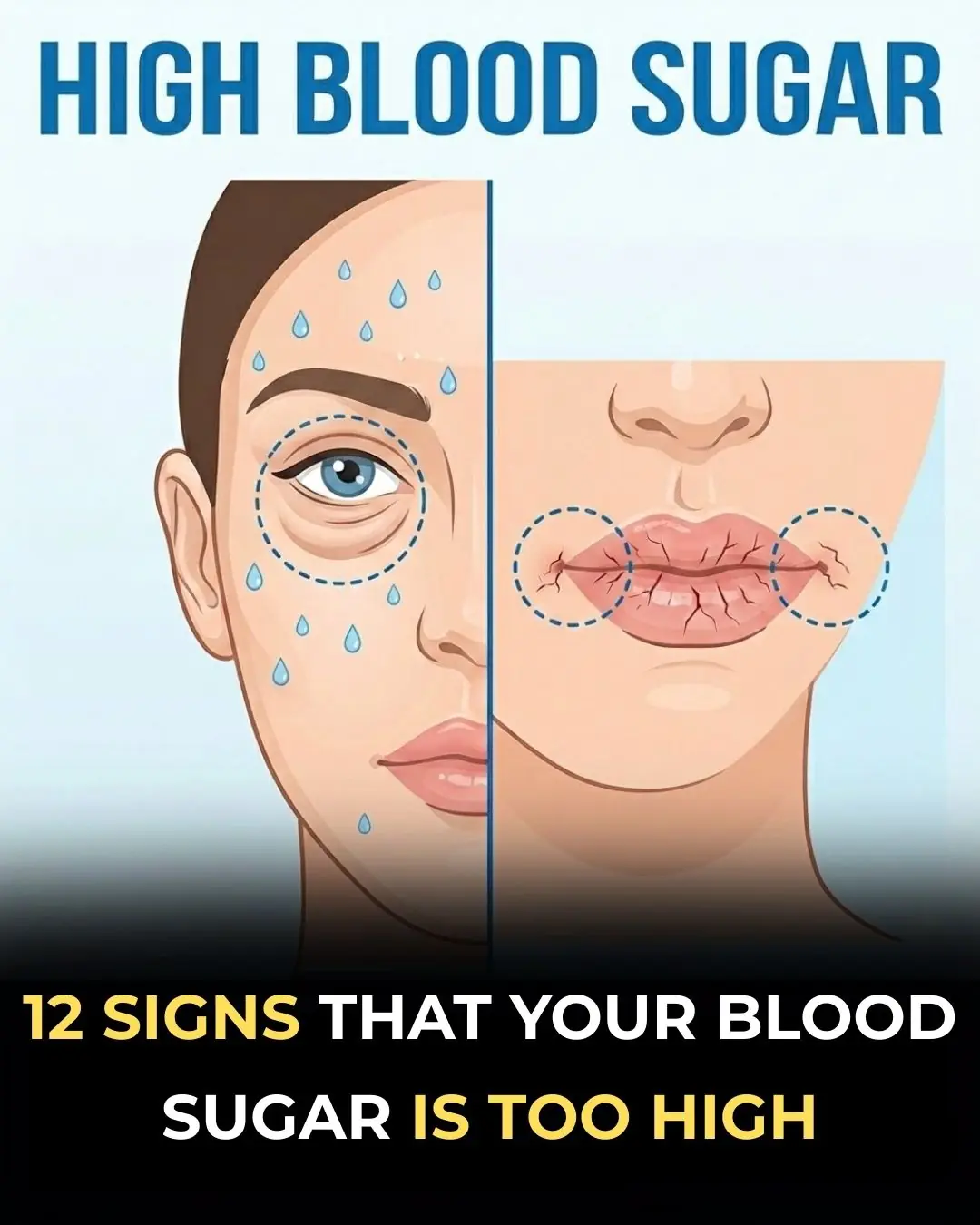
The High-Sugar Alert: Recognizing the 12 Key Symptoms Your Body is Showing You
Boiling Potatoes Without Water: Use This Simple Ingredient for Soft, Sweet, Fluffy Results

Which Fruits Should Cancer Patients Avoid? Dietary Guidance During Cancer Treatment
Visceral Fat Is Increasing: Doctors Recommend 9 Foods to Help Reduce It and Should Be Eaten Regularly
Lung Cancer Warning Signs: If You Often Notice These 4 Symptoms in the Morning, Don’t Ignore Them
News Post

Adding Yoga to Opioid Use Disorder Care May Speed Recovery From Opioid Withdrawal

Sunlight at Work Beats Artificial Light for Glucose Control in Type 2 Diabetes

How to Whiten Laundry Naturally
Harvard Doctor Reveals Foods You Should Avoid to Prevent Inflammation

If You Have Fig Leaves, You Have Gold—and You Didn’t Even Know It

Doctor Warns of Mesotherapy’s Risky Side, Causing Reptile-Like Skin

It’s surprising how unclear the link between chicken color and quality still is for many people
🤧 Constant Phlegm in Throat? The Real Causes (and How to Actually Get Rid of It)

Why Daily Showers After 65 May Do More Harm Than Good
Scientists Discover Alarming Substance in Human Blood, Raising Serious Concerns
7 easy ways to quickly unclog your lymph nodes to reduce swelling and flush out toxins

What Really Happens When You Eat a Banana Before Bed

Natural Ways to Relieve Cough and Chest Congestion
People whose mouths feel dry when sleeping at night need to know these 8 reasons

Why Eating More Processed Meat Increases Your Risk for Serious Health Problems
That detail isn’t innocent… and few people know it
Doctor Reveals That Eating Guava Can Cause Powerful Changes in Your Body
Stephen A. Smith speaks out on ‘NBA Countdown’ exit