Breakthrough in Diabetes Treatment: Gene-Edited Cells May Cure Type 1 Diabetes Without Immunosuppressants!
A Potential Cure for Type 1 Diabetes May Be Within Reach
Recent advancements in medical science suggest that a potential cure for type 1 diabetes could be within our grasp. In a pioneering trial, a patient has begun producing his own insulin after receiving a transplant of gene-edited pancreatic islet cells. What makes this development especially significant is that the patient has not required any immunosuppressive drugs, a groundbreaking achievement in the treatment of this condition. This trial marks the first time that donor islet cells have been genetically engineered to fully evade the human immune system, offering a new avenue for curing type 1 diabetes.
Type 1 diabetes is an autoimmune condition in which the body's immune system mistakenly attacks and destroys the insulin-producing islet cells in the pancreas. As a result, individuals with this condition are left reliant on external insulin to regulate their blood glucose levels. Traditional treatments for type 1 diabetes typically involve lifelong insulin injections or, in some cases, organ transplants, such as a pancreas or islet cell transplant. However, these transplant procedures require the use of immunosuppressive drugs to prevent the body from rejecting the transplanted cells, a practice that carries significant risks, including increased vulnerability to infections and other complications.
The trial in question involved a 42-year-old man who had been living with type 1 diabetes since childhood. This patient was treated with genetically modified islet cells obtained from a donor. The cells were injected into the patient's forearm, where they began to function and respond to glucose by producing insulin naturally. What made this experiment particularly revolutionary was the fact that the patient did not need to take any immunosuppressive drugs to prevent rejection. This marks a remarkable departure from traditional transplant protocols.
Before the transplant, researchers used the CRISPR gene-editing technology to make three crucial changes to the donor cells. Two of these edits removed markers that the immune system would typically use to identify the cells as foreign, while the third addition involved the insertion of the CD47 protein. This protein helps to block innate immune responses, ensuring that the transplanted cells are not attacked by the body's defense mechanisms. These genetic modifications allowed the transplanted islet cells to survive and function without being destroyed by the immune system.
Over the course of 12 weeks, the gene-edited cells began to respond to glucose levels in the patient's body, producing insulin as needed. The most promising part of the trial was that only the cells with all three genetic modifications survived and continued to function properly. This confirmed that the gene-editing strategy was effective in preventing immune rejection and ensuring that the transplanted cells could perform their intended function. While the patient did not receive enough cells to completely eliminate his reliance on external insulin, this study demonstrates that immune-evasive, functional cell therapies can survive and operate within the human body, opening up exciting possibilities for the future of diabetes treatment.
The results of this trial offer a glimmer of hope for millions of individuals suffering from type 1 diabetes. If further studies can replicate these findings and improve upon the technology, gene-edited pancreatic islet cell transplants could become a standard treatment, potentially leading to a cure for the disease. Moreover, this breakthrough in gene editing holds the promise of transforming the way autoimmune diseases are treated, not just for diabetes but for a variety of other conditions that involve the immune system attacking the body’s own cells.
In the coming years, researchers will need to conduct further trials to refine this process, increase the success rate of the transplant procedure, and determine how to expand the number of patients who could benefit from it. However, the success of this study provides a crucial stepping stone toward a future where type 1 diabetes may no longer be a lifelong condition but a treatable illness, offering hope to millions around the world.
Source: “Survival of Transplanted Allogeneic Beta Cells with No Immunosuppression,” New England Journal of Medicine (2025).
Additionally, these findings were reported by multiple reputable sources, including the National Institutes of Health (NIH) and Nature Medicine, both of which are highly respected for their contributions to scientific research. The advancements in gene-editing techniques like CRISPR have already demonstrated immense potential in the field of medicine, and this study serves as a promising example of how these tools can be used to overcome some of the most challenging diseases affecting humanity.
News in the same category

Revolutionary Brain Stimulation Technique Shows Potential to Reverse Alzheimer's Damage!

Cutting Sugar for Just 9 Days Can Transform Your Liver Health – Here's How!
South Korea's Hilarious 'Space-Out Competition': The Ultimate Sport of Doing Absolutely Nothing!

Female Frogs 'Play Dead' to Escape Forced Mating – You Won't Believe How They Do It!

Objects People Were Confused About Their Purpose
Robot 'Kidnaps' Fellow Machines at Shanghai Exhibition, Sparking Debate on AI Autonomy and Labor Rights

Introducing the U-Hawk: The Autonomous Black Hawk Revolutionizing Heavy-Lift Aviation

China Unveils World's Largest Solar Farm, Powers Up with 3.5 GW in Xinjiang

Australia’s “Infinity Train” — A Self-Recharging Heavy-Haul Giant Powered by Gravity

The New York Hairstylist Who Spends His Day Off Helping the Invisible People of the City

The $400 Million Car Carrier That Sank Into the Atlantic: A Tale of Fire, Luxury Cars, and Environmental Risks

Sweden’s RFID/NFC Implant Trend: Unlocking Convenience or Opening the Door to Privacy Concerns?

Alice Walton’s Groundbreaking Medical School: A New Era for Medicine and Healthcare
Get Ready for the Geminid Meteor Shower: A Stunning Celestial Show on December 13-14

12 Foods to Eat When You're Sick: Nourishing Your Body Back to Health

Kim Kardashian Joins Fortnite as Newest Icon Series Skin with Exclusive Bundles
12 Strange Body Symptoms — Explained
News Post
The 4 hidden causes of persistent phlegm in your throat (& how to fix it naturally)
Understanding the Signs and Symptoms of Mineral Deficiencies
4 popular supplements that rapidly drain potassium from your body

Turmeric and vitamin D are allies against high blood pressure in diabetes

This is How Headaches Reveal What is Wrong With Your Health
#1 best way to reverse & slow dementia
How to shrink thyroid nodules naturally with 2 key minerals
How to Unclog a Sink in an Emergency (When You Have Nothing on Hand)
Genius! My Nana’s Simple Trick for Cleaning Dusty Window Blinds With Almost No Effort
I Had No Clue About This Hidden Fridge Button — It Could Be Wasting You Serious Money
I Had No Idea These Kids’ Snacks Contain Petroleum-Based Chemicals
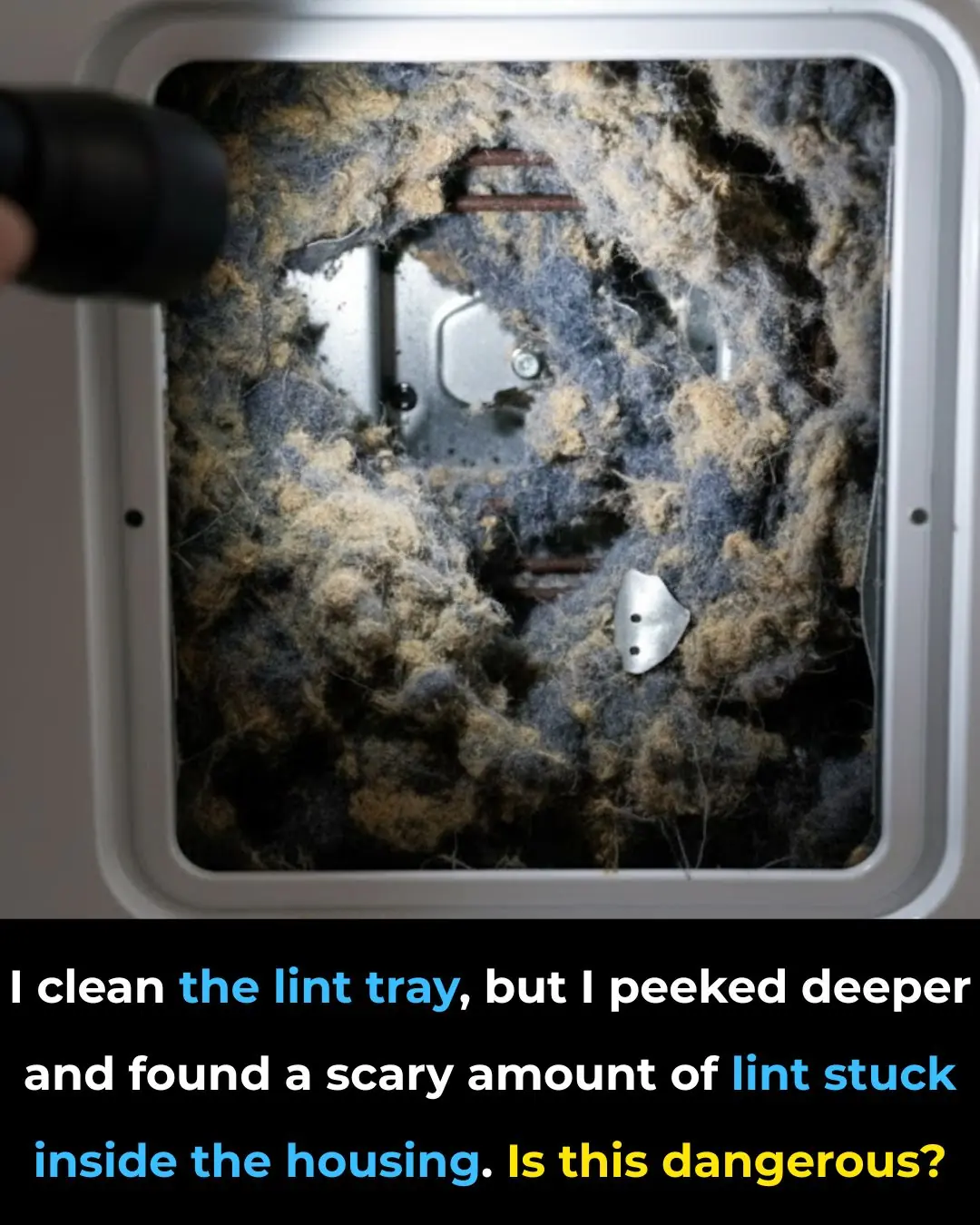
I Clean the Lint Trap—But I Found a Shocking Amount of Lint Inside the Dryer. Is This Dangerous?

Dark Purple Spots Keep Showing Up on Your Hands? Here’s What to Do While You Wait to See a Doctor

The Number One Deficiency Behind Aging Spots

They Look So Harmless — But Tick Eggs Can Be a Serious Problem

Moved Into a New Place and Found Gross Yellow Stains Under the Toilet Seat? Try These Fixes Before Replacing It

If You Get These Bruises On Your Body

Revolutionary Graphene Filter Instantly Turns Seawater Into Drinkable Water—A Game-Changer for Global Water Shortages!