
How Helicobacter pylori Revolutionized the Understanding of Stomach Ulcers
In the early 1980s, Dr. Barry Marshall fundamentally changed the medical community’s understanding of stomach ulcers, overturning decades of deeply rooted assumptions. At that time, peptic ulcers were widely believed to be caused by stress, spicy foods, smoking, or unhealthy lifestyle habits. As a result, treatment often focused on long-term symptom management, dietary restrictions, or even invasive surgery, rather than addressing an underlying cause.
Working alongside pathologist Dr. Robin Warren in Australia, Marshall began to suspect that a previously overlooked bacterium—later identified as Helicobacter pylori—played a central role in chronic gastritis and peptic ulcer disease. Their hypothesis directly challenged conventional medical wisdom, and many experts initially dismissed the idea that bacteria could survive in the acidic environment of the human stomach.
In 1984, faced with widespread skepticism and limited acceptance of their research, Marshall took an extraordinary and controversial step to prove his theory. He deliberately ingested a culture of live H. pylori bacteria. Within days, he developed symptoms of acute gastritis, including nausea and stomach inflammation. After confirming the presence of the bacteria in his stomach, Marshall treated himself with antibiotics and recovered fully. This dramatic self-experiment provided compelling evidence that ulcers were the result of a bacterial infection rather than purely lifestyle-related factors—and that they could be effectively cured with antibiotic therapy instead of surgery.
Although the medical establishment was slow to accept these findings, continued research eventually confirmed the link between H. pylori and peptic ulcer disease. Over time, Marshall and Warren’s work revolutionized gastrointestinal medicine, leading to standardized antibiotic treatments that dramatically reduced ulcer recurrence rates. Their discovery also had profound implications for cancer prevention, as H. pylori infection is now recognized as a major risk factor for gastric cancer.
In recognition of their groundbreaking contribution to medical science, Dr. Barry Marshall and Dr. Robin Warren were awarded the Nobel Prize in Physiology or Medicine in 2005. Their work is now considered a classic example of how scientific persistence and evidence-based research can transform clinical practice and improve global health outcomes.
Today, Dr. Barry Marshall continues to contribute to research on H. pylori and infectious diseases, while his legacy inspires generations of scientists and healthcare professionals. His discovery has improved the lives of millions of patients worldwide and stands as a powerful reminder that challenging established beliefs is often essential for scientific progress.
Beyond its immediate clinical impact, the discovery of Helicobacter pylori reshaped how scientists understand chronic diseases more broadly. Marshall’s work helped establish that long-standing inflammatory conditions could have infectious origins, opening new directions for research in gastroenterology, immunology, and microbiology. This paradigm shift encouraged scientists to reexamine other diseases once thought to be driven solely by genetics or lifestyle factors.
The global adoption of H. pylori eradication therapy has had measurable public health benefits. Studies show that treating the infection not only heals ulcers but also lowers the long-term risk of complications such as gastrointestinal bleeding and gastric malignancies. In regions with high prevalence of H. pylori, especially in parts of Asia, Africa, and Latin America, antibiotic-based treatment strategies have become an essential component of preventive healthcare.
Marshall’s story is also frequently cited as a powerful example of scientific courage and ethical debate. While self-experimentation is no longer encouraged under modern research standards, his actions highlighted the importance of rigorous evidence when confronting entrenched medical beliefs. His willingness to challenge authority underscored the need for openness to new ideas, even when they disrupt long-standing practices.
Today, the legacy of Dr. Barry Marshall extends far beyond ulcer treatment. His research continues to influence medical education, clinical guidelines, and global health policy. The recognition of H. pylori as a major pathogen has improved diagnostic methods, refined antibiotic use, and contributed to a deeper understanding of how microbes interact with the human body over time.
Ultimately, Marshall’s discovery serves as a reminder that medical progress often begins with questioning what is assumed to be true. By following scientific evidence rather than convention, he transformed patient care worldwide and demonstrated how persistence, curiosity, and integrity can lead to breakthroughs that save millions of lives.
News in the same category


Redefining Diabetes Treatment

If your partner says goodbye with a kiss on the forehead, be very careful: this is what it really means

Here’s what the letter ‘M’ and the crescent moon on the palm of your hand truly signify

New Research Raises Brain Health Concerns About a Common Sweetener

🌟 Breakthrough in Cancer Treatment: Targeted Light Therapy
HHS to Reexamine Cell Phone and 5G Radiation Risks Following Direction From RFK Jr

Injectable Gel for Nerve Regeneration: A Breakthrough in Healing
Processed Meats and Cancer Risk: What You Need to Know
Microplastics in Human Testicles: A Wake-Up Call for Reproductive Health
A Geologist Explains What Makes Greenland So Incredibly Special

They Successfully Cured HIV in a 60-Year-Old German Man Using a Stem Cell Transplant; He Has Been Disease-Free for 6 Years
A study shows that oxytocin, the ‘love hormone,’ can help regenerate the heart after injury.
Renewable Energy Boom Drives Down Electricity Prices in Australia

Male humpback whale crossed 3 oceans for sex, inadvertently breaking distance record for species
Lithium deposit valued at $1.5 trillion has been discovered in the U.S.
The Babylonians discovered the Pythagorean Theorem 1,000 years before Pythagoras

Scientists Just Started Testing a Universal Cancer Vaccine on Humans
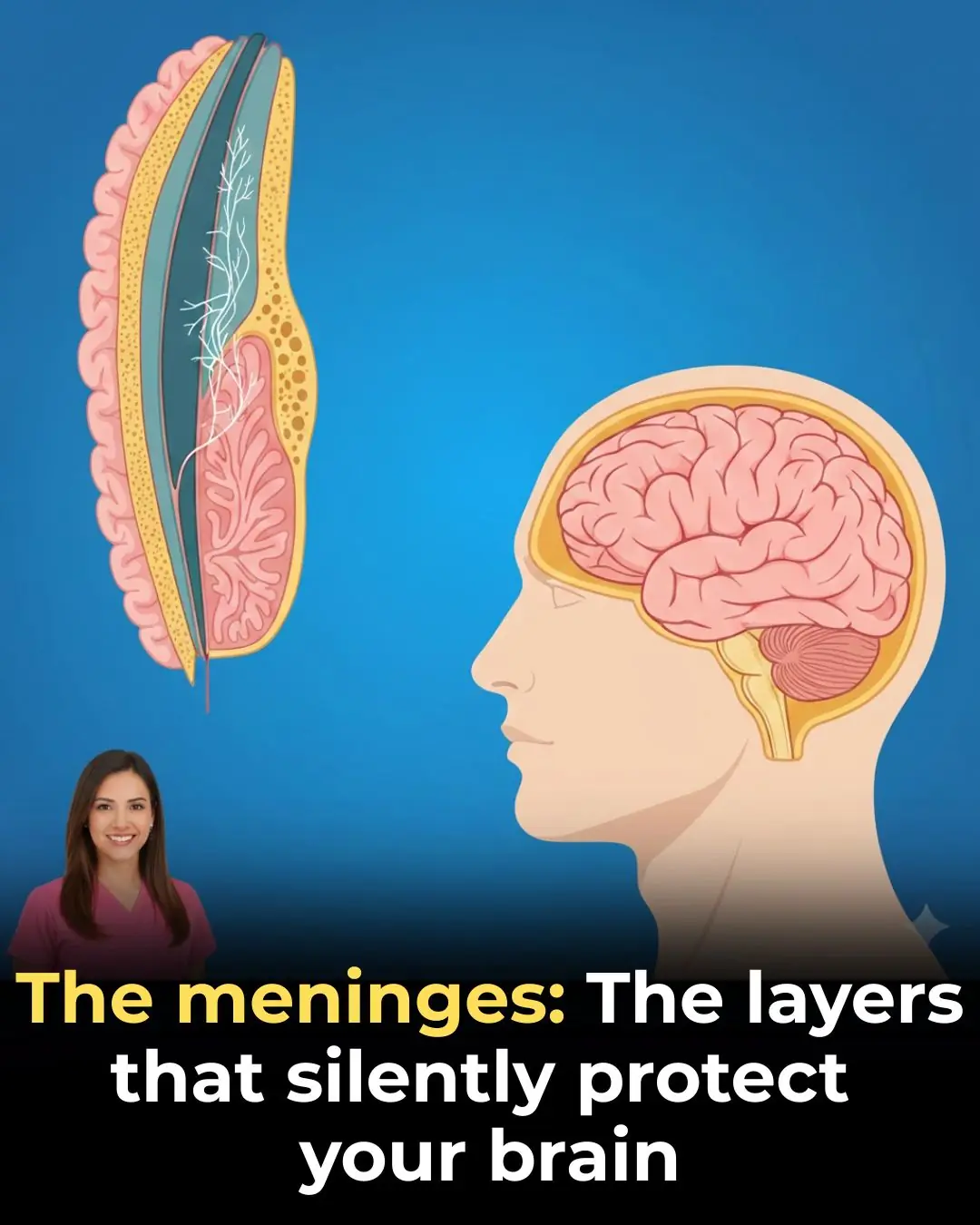
🧠 The Meninges: The Silent Layers That Protect Your Brain
News Post

Nanobot Technology: A New Frontier in Cardiovascular Disease Treatment

Redefining Diabetes Treatment

If your partner says goodbye with a kiss on the forehead, be very careful: this is what it really means

7 habits that make you look ugly...
If you're a woman with chin whiskers, pay attention. Here's what it means

Here’s what the letter ‘M’ and the crescent moon on the palm of your hand truly signify

🏠 8 Household Items That Could Be Affecting Your Health (And How to Check Them Safely at Home)

Why Some People Put Water Bottles Outside Their Homes
If your cat comes near your face while you sleep, this is happening in your life
10 Benefits of Drinking Rosemary Tea on an Empty Stomach

Red Bumps That Look Like Goosebumps
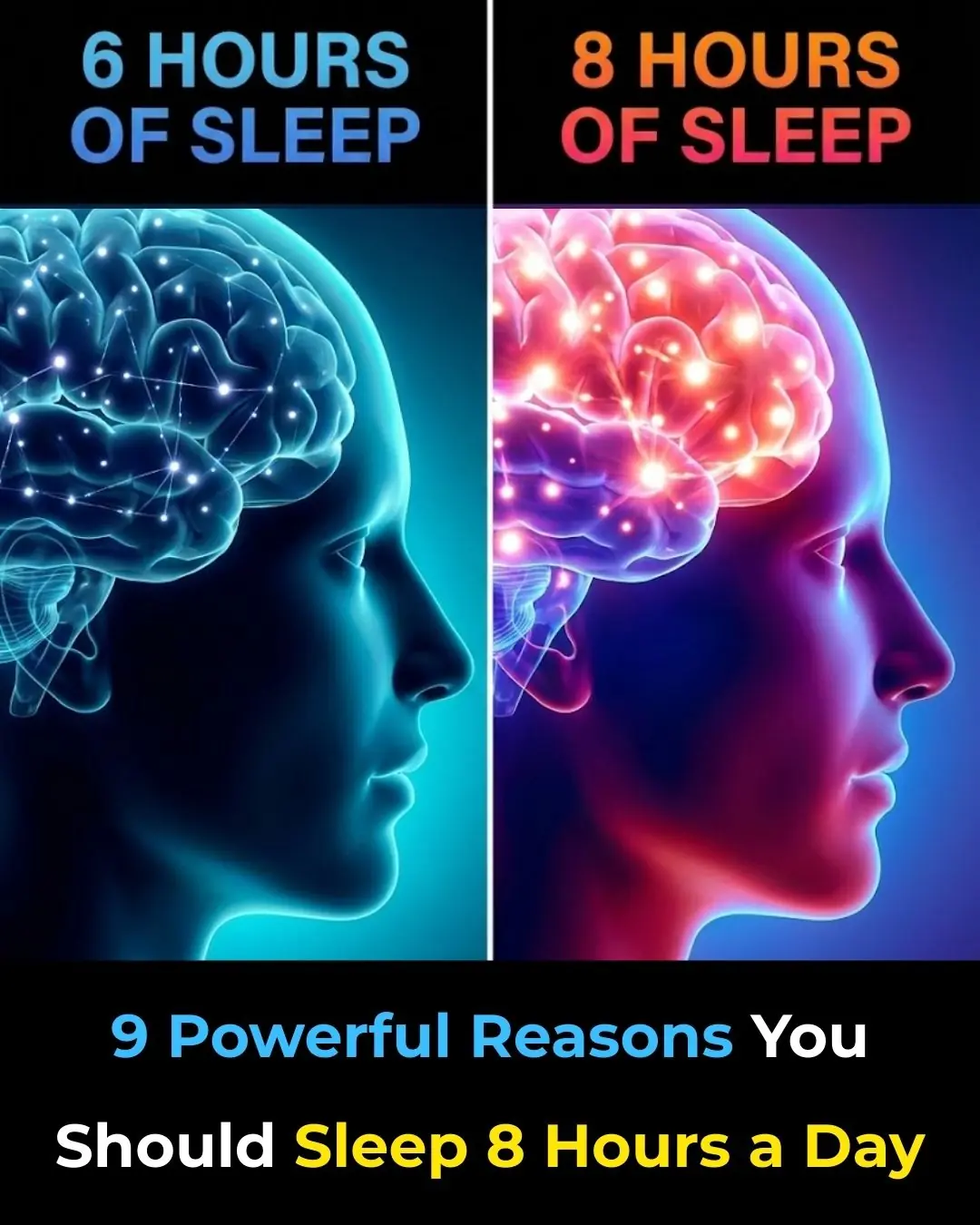
Reasons You Should Sleep 8 Hours a Day

Thrown into the Snow for Being “Infertile,” a Woman Finds Unexpected Hope in a Widowed CEO

The Blind Billionaire’s Unexpected Dinner Guest: How One Little Girl Changed Everything

A Brutal Betrayal: How a CEO Husband’s Cruelty Led to a Stunning Revenge

The Cold Revenge of Sofía: A Woman’s Unforgiving Response to Betrayal

A Father's Regret: The Truth That Shattered My Heart After Ten Years
A Heart-Wrenching Discovery: A Mother's Unbelievable Recognition of Her Daughter's Tattoo

Lola's Courageous Fight After Snake Bite: A Story of Bravery and Resilience
