This new development is part of a broader shift in how scientists approach neurological diseases. Instead of focusing solely on halting degeneration, researchers are increasingly exploring neuroregeneration - ways to repair or replace damaged cells and re
In a discovery that could revolutionize the future of neurodegenerative disease treatment, scientists have unveiled a promising new drug that may not only halt the progression of Parkinson’s disease, but actually reverse its damaging effects on the brain - potentially restoring lost neural function and “bringing the brain back to life.”
The study, recently published in the prestigious journal Science Signaling, offers compelling evidence that this treatment could go far beyond symptom management, opening the door to a form of regenerative therapy once considered science fiction.
As the brain is the body's command center, disorders affecting it - particularly progressive ones like Parkinson’s - have long confounded doctors and researchers. Despite rapid advancements in other areas of medicine, cognitive and neurological diseases remain among the most difficult to treat. Parkinson’s disease alone affects over 10 million people worldwide, causing symptoms such as tremors, muscle stiffness, balance issues, and cognitive decline.
But this newly explored therapy could change that.
The Drug Behind the Discovery: MLi-2
At the heart of this groundbreaking research is MLi-2, a drug designed to inhibit the activity of a key enzyme in the brain known as LRRK2 (leucine-rich repeat kinase 2). Mutations in the LRRK2 gene are known to be one of the most common genetic causes of Parkinson’s disease, responsible for up to 25% of hereditary cases and a significant number of sporadic cases.
The research team, led by scientists from Stanford University, genetically engineered mice to overexpress the LRRK2 enzyme, mimicking the brain conditions observed in Parkinson’s patients. Over a period of three months, these mice were treated with the drug MLi-2 - and the results stunned the team.
Not only did MLi-2 successfully halt the damaging effects caused by overactive LRRK2, but it also triggered regeneration in already damaged areas of the brain. This unexpected phenomenon suggests that neurons weren’t just being protected from further damage - they were actively repairing themselves.

“These findings suggest that it might be possible to improve, not just stabilize, the condition of patients with Parkinson's disease,” said study co-author Dr. Suzanne Pfeffer, the Emma Pfeiffer Merner Professor in Medical Sciences at Stanford.
“We're so excited about these findings,” she continued. “They suggest this approach has great promise to help patients in terms of restoring neuronal activity in this brain circuit. There are multiple LRRK2 inhibitor clinical trials underway, and our hope is that these findings in mice will hold true for patients in the future.”
How Does MLi-2 Work?
To understand the significance of this discovery, it’s important to grasp how the LRRK2 enzyme contributes to Parkinson’s.
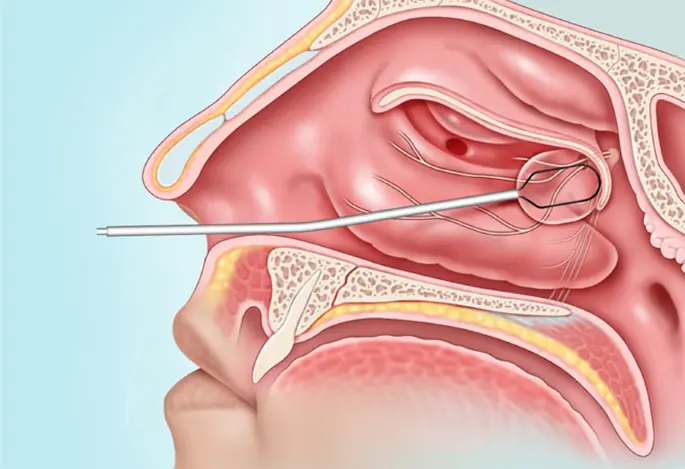
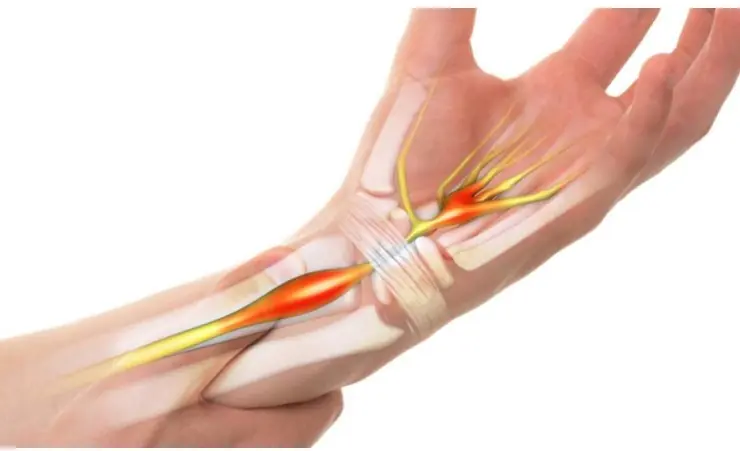
LRRK2 affects a critical part of brain cell structure called the primary cilium - a tiny, antenna-like projection on the surface of cells that plays a vital role in signaling between neurons. When LRRK2 is overactive, it damages or destroys these cilia, disrupting communication in brain circuits and contributing to the loss of dopamine-producing neurons - a hallmark of Parkinson’s disease.
This disruption is particularly devastating when it interferes with the brain’s ability to respond to a neuroprotective signal known as Sonic Hedgehog. This signal - despite its whimsical name - is crucial in maintaining the health of striatal neurons, which are responsible for motor control and are highly vulnerable in Parkinson’s patients.
When these neurons lose their primary cilia due to LRRK2 overactivity, they no longer respond effectively to Sonic Hedgehog, leading to cascading neuronal death.
MLi-2, however, not only inhibited LRRK2 but also promoted the regrowth of primary cilia, restoring intercellular communication and rejuvenating the brain’s capacity to heal itself.
Reversing the Clock on Neurodegeneration
While most treatments for Parkinson’s today focus on symptom relief - such as dopamine replacement therapy - MLi-2 represents a paradigm shift. Instead of just slowing down deterioration, it may actually reverse it, allowing the brain to repair past damage.
In the treated mice, previously lost neural connections began to reform. This regenerative effect opens the door to a future where Parkinson’s may not be a lifelong, progressively worsening condition, but a treatable - and possibly reversible - illness.
Even more encouraging is the timing of these effects. The signs of Parkinson’s can begin more than a decade before the hallmark tremors appear, making early detection and treatment incredibly valuable. If MLi-2 proves effective in humans, it could offer doctors a window to intervene before significant brain damage occurs, especially in high-risk patients with known LRRK2 mutations.
Clinical Trials and Future Outlook
While this study was conducted in mice, human trials are already underway for LRRK2 inhibitors, including MLi-2 and related compounds. These trials will help determine whether the benefits seen in mice - including brain regeneration - translate to human patients, and whether the drug is safe for long-term use.
“Our hope is that these findings in mice will hold true for patients in the future,” said Dr. Pfeffer. Her optimism is shared by many in the neuroscience community, who view this as one of the most promising leads in Parkinson’s research in years.
The drug's development could also open avenues for treating other neurological conditions involving cilia dysfunction and neuroinflammation, such as certain types of dementia and even some psychiatric disorders.
However, experts caution that while the results are exciting, it is still early days. Larger and longer human studies will be required to confirm efficacy, determine appropriate dosages, and monitor potential side effects.
Implications Beyond Parkinson’s
The implications of MLi-2 stretch beyond just one disease. Because primary cilia are vital in numerous cellular processes - from brain development to immune response - the ability to regrow and restore cilia may have far-reaching applications.
For instance, Alzheimer’s disease, Huntington’s disease, and certain forms of brain injury could all theoretically benefit from similar regenerative approaches. The restoration of neuronal connectivity and signal transmission might help rejuvenate brain circuits damaged by trauma or chronic disease.
Furthermore, the LRRK2 pathway is also being investigated in relation to inflammatory responses, suggesting that inhibitors like MLi-2 could one day be part of a broader toolkit for managing both neurological and systemic conditions.

A New Frontier in Neurodegenerative Medicine
This new development is part of a broader shift in how scientists approach neurological diseases. Instead of focusing solely on halting degeneration, researchers are increasingly exploring neuroregeneration - ways to repair or replace damaged cells and restore lost brain function.
While it may take years before a drug like MLi-2 is widely available, the trajectory is clear: the future of Parkinson’s treatment lies not just in slowing the disease, but in reversing it.
“We are finally entering an era where regenerative medicine is no longer a distant dream, but a tangible possibility,” commented Dr. Pfeffer. “This is the beginning of something truly transformative for patients and their families.”