
This Could Be Why Lung Cancer Is Rising in People Who Never Smoked
Lung Cancer in Non-Smokers: The Hidden Risks You Should Not Ignore
Lung cancer has long been considered a smoker’s disease. However, growing evidence tells a very different and concerning story. Today, up to 20% of newly diagnosed lung cancer cases occur in people who have never smoked. This trend is particularly evident among women and younger adults, with adenocarcinoma now identified as the most common subtype in non-smokers.
If tobacco is not the cause, what is silently damaging the lungs of people who have never lit a cigarette?
Current research points to a complex interaction of environmental exposure, genetic susceptibility, and lifestyle-related inflammation. Understanding these hidden risks — and acting early — can dramatically improve outcomes, shifting diagnosis from late-stage disease to early, treatable cancer.
Air Pollution: A Constant and Invisible Threat
Air pollution is one of the strongest non-smoking risk factors for lung cancer. Fine particulate matter, especially PM2.5 and PM10, originates from vehicle exhaust, industrial emissions, construction dust, and wildfires. These microscopic particles penetrate deep into the lungs and lodge in the alveoli.
Once inside lung tissue, they trigger chronic inflammation, oxidative stress, and DNA damage. Over time, this cellular injury can lead to malignant transformation. Importantly, exposure often occurs without obvious symptoms, meaning damage accumulates silently for years.
People living or working near busy roads, industrial zones, or dense urban centers face significantly higher daily exposure.
How to Reduce Pollution Exposure
-
Ventilate your home during early mornings or late evenings when traffic is lower
-
Use a HEPA air purifier indoors, especially in bedrooms
-
Choose walking or jogging routes away from major roads
-
Avoid outdoor exercise during pollution alerts or wildfire smoke events
Radon: A Little-Known but Serious Household Risk
Radon is a naturally occurring radioactive gas released from soil and certain rock types, particularly granite. It can enter homes through cracks in floors, walls, or foundations and accumulate in basements or ground-level rooms.
Radon is the second leading cause of lung cancer overall and the leading cause among non-smokers. It is colorless, odorless, and tasteless, making it impossible to detect without testing. When inhaled over long periods, radon releases radioactive particles that damage lung cell DNA.
How to Detect and Reduce Radon Exposure
-
Use an at-home radon testing kit or hire a certified radon inspector
-
If levels exceed 200 Bq/m³ (or 4 pCi/L), install mitigation systems such as sub-slab ventilation
-
Seal visible foundation cracks and improve airflow
-
Maintain regular cross-ventilation, especially in lower levels of the home
Genetics: When Lifestyle Isn’t the Primary Cause
In many non-smokers, lung cancer is driven by specific genetic mutations rather than environmental exposure alone. Mutations such as EGFR, ALK, KRAS, and ROS1 are particularly common in non-smoking women and individuals of Asian descent.
The encouraging news is that advances in targeted therapy have dramatically improved survival and quality of life for patients with these mutations, even in advanced-stage disease.
When Genetic Testing Should Be Considered
-
A family history of lung cancer diagnosed before age 60
-
Personal history of cancers associated with these mutations
-
Diagnosis of lung cancer in a lifelong non-smoker
-
Belonging to a higher-prevalence group, such as Asian non-smokers
Inflammatory Lifestyle: Diet, Inactivity, and Excess Weight
Lifestyle factors play a critical but often overlooked role. Diets low in fruits and vegetables reduce antioxidant intake, limiting the body’s ability to neutralize free radicals. At the same time, physical inactivity and excess body weight promote chronic systemic inflammation.
This inflammatory environment weakens immune surveillance and reduces the body’s capacity to repair damaged cells, increasing vulnerability to cancer development — even in people with no smoking history and relatively healthy lungs.
Simple Lifestyle Changes That Matter
-
Consume at least five servings of colorful fruits and vegetables daily
-
Engage in 30 minutes of moderate physical activity most days of the week
-
Maintain a healthy BMI to reduce inflammatory markers
-
Stay well-hydrated to support metabolic and detoxification processes
Rethinking Lung Cancer Screening
Low-dose CT scans are proven to detect lung cancer at early stages, but current screening guidelines primarily focus on heavy smokers. As lung cancer rates rise among non-smokers, many experts now argue that screening criteria should expand.
Individuals with prolonged exposure to air pollution, high household radon levels, or strong family history may benefit from earlier assessment — even without a smoking history.
How to Talk to Your Doctor
Prepare specific information:
-
Years spent living in high-pollution environments
-
Radon test results from your home
-
Family history of lung or related cancers
-
Persistent symptoms such as chronic cough, chest discomfort, or unexplained fatigue
Ask for a personalized risk assessment rather than relying solely on smoking history.
Frequently Asked Questions
I don’t smoke but live in a large city. Should I be concerned?
Yes. Long-term exposure to urban air pollution significantly increases lung cancer risk, particularly with frequent traffic exposure.
Is radon testing expensive?
No. Affordable test kits are widely available and represent a small investment compared to the potential health risks.
Does exercise really reduce lung cancer risk in non-smokers?
Yes. Regular physical activity improves lung capacity, lowers inflammation, and enhances cellular repair mechanisms.
Who should consider EGFR or ALK genetic testing?
Non-smokers with early-onset disease, strong family history, or belonging to high-prevalence populations should discuss testing with a specialist.
Conclusion
The increasing incidence of lung cancer among people who have never smoked proves that cigarettes are not the only threat to lung health. Invisible air pollutants, hidden household gases, genetic factors, and chronic inflammation all contribute to risk.
Testing for radon, reducing pollution exposure, maintaining an anti-inflammatory lifestyle, and advocating for personalized screening form a powerful strategy to protect your lungs — even if you have never touched a cigarette.
Early awareness is no longer optional.
It is essential.
News in the same category


The Surprising Health Benefits of Boiled Eggs

🚨 Recurrent Yeast Infections? STOP Doing These Things Immediately!
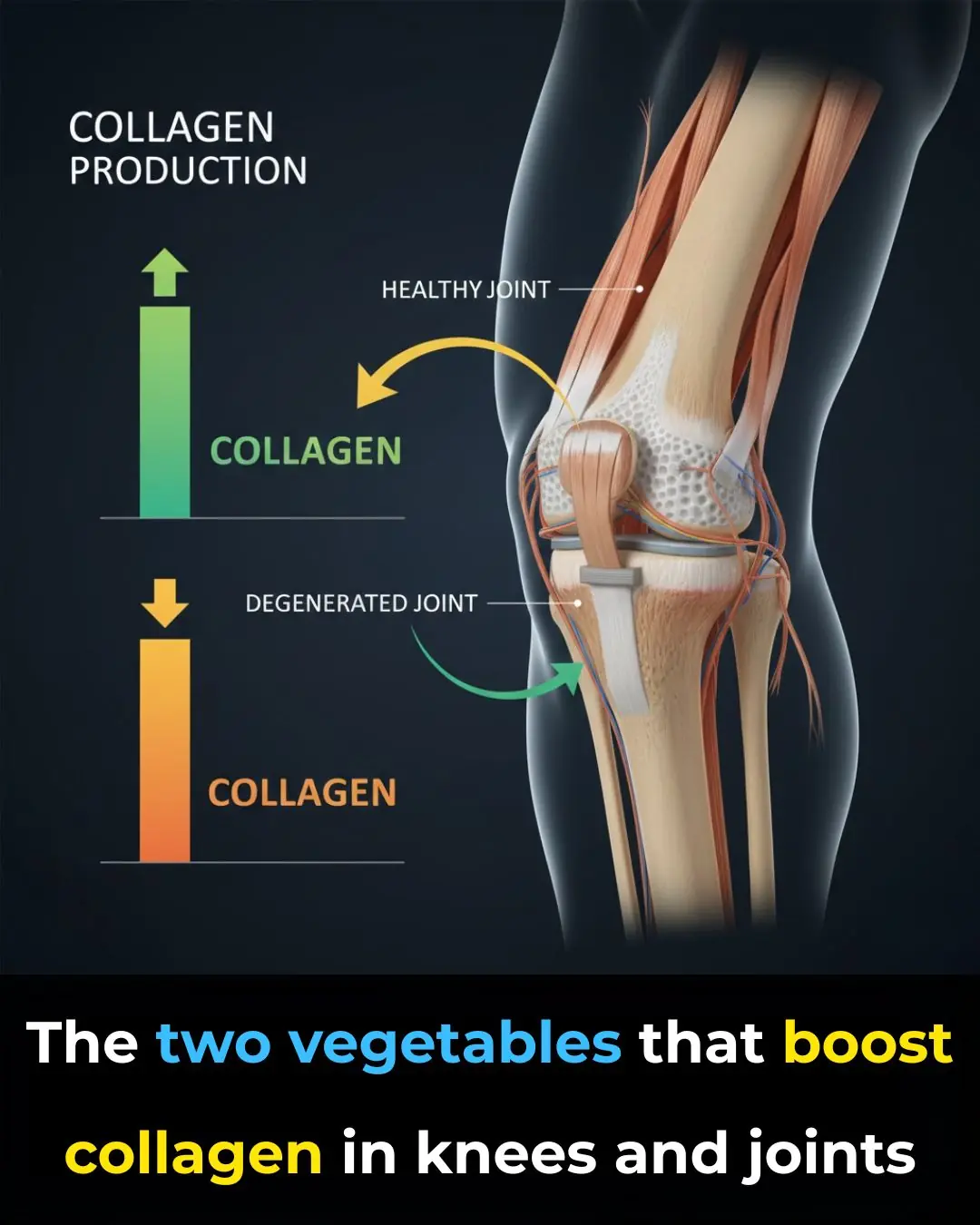
Doctors Are Amazed: Two Vegetables That Boost Collagen in the Knees and Relieve Joint Pain
One Powerful Leaf That Supports Blood Sugar, Blood Pressure, Pain Relief, Cholesterol & Circulation

Discover the Natural Benefits of Air Plant Leaf for Daily Eye Care

Step-by-Step Guide to Making a Homemade Baking Soda Cream for Skin Care

The Forgotten Leaf That Might Support Your Defenses (No Magical Promises)

The Nighttime Bite That May Help Wake Up Your Circulation

Natural Energy Booster: Ginger and Tomato for Long Day Vitality
15 autoimmune warning signs your doctor keeps dismissing as stress or aging

Why You Keep Waking Up With a Dry Mouth
🦴 Hip Pain: What Does It Mean? Common Causes & When to Seek Help

You see Lipton tea, cloves, and ginger?

Boiling Garlic in Milk and Drinking It Once: Why So Many People Are Trying This Old Remedy
🌿 What Rosemary Can Actually Do
Early Symptoms of Ovarian Cancer
When your head itches:... Please know this

🥚 What Causes the Green Ring Around Hard-Boiled Eggs?
News Post

10 Ways to Kill a Toothache In a Minute

A Pregnant Woman Warned a Stranger to Run

The Surprising Health Benefits of Boiled Eggs

🚨 Recurrent Yeast Infections? STOP Doing These Things Immediately!
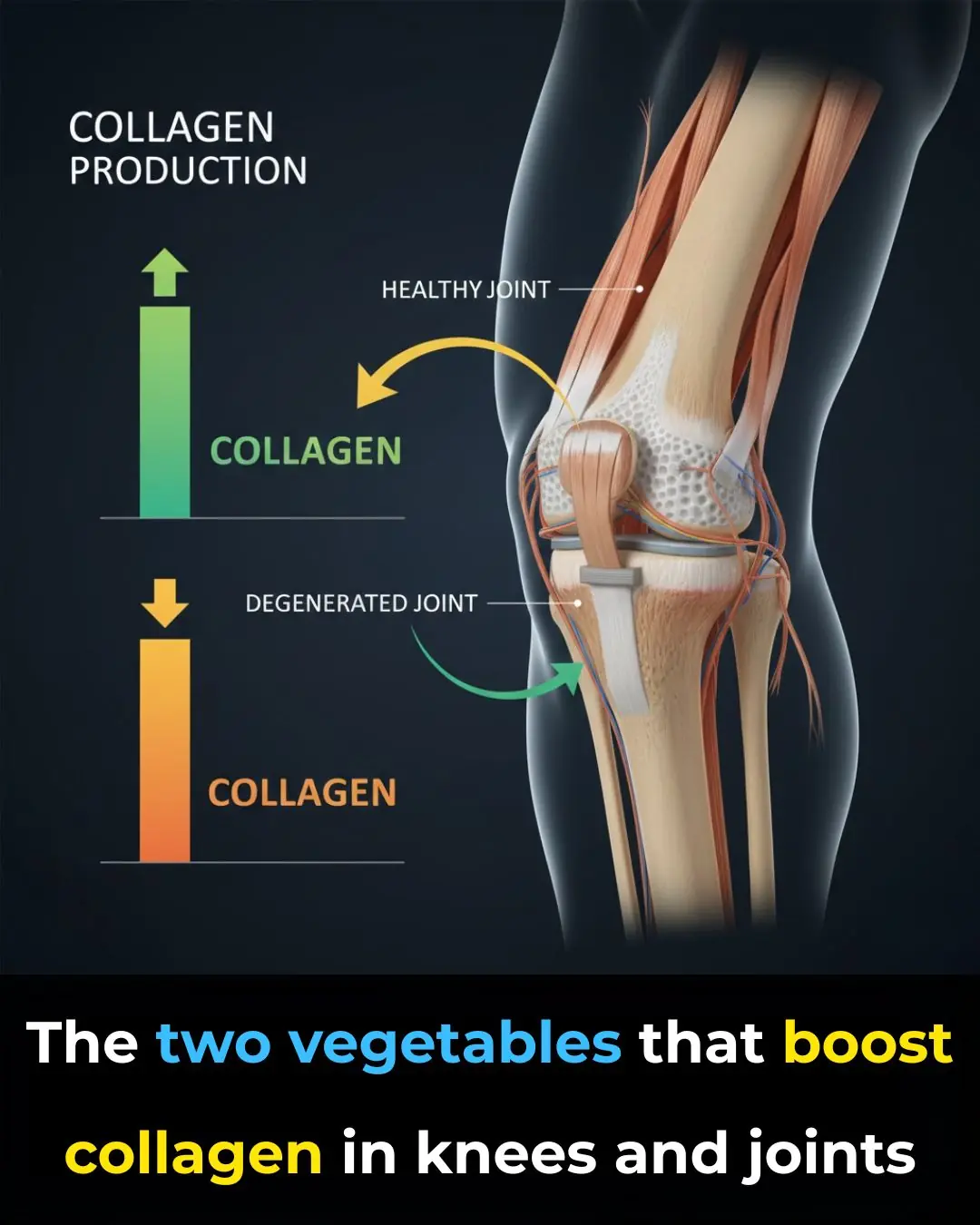
Doctors Are Amazed: Two Vegetables That Boost Collagen in the Knees and Relieve Joint Pain
One Powerful Leaf That Supports Blood Sugar, Blood Pressure, Pain Relief, Cholesterol & Circulation

Discover the Natural Benefits of Air Plant Leaf for Daily Eye Care

Step-by-Step Guide to Making a Homemade Baking Soda Cream for Skin Care

The Forgotten Leaf That Might Support Your Defenses (No Magical Promises)

The Nighttime Bite That May Help Wake Up Your Circulation
The Boy Who Ended the Robbery

Natural Energy Booster: Ginger and Tomato for Long Day Vitality

This Grocery Store Moment Changed Two Lives Forever
15 autoimmune warning signs your doctor keeps dismissing as stress or aging
They Laughed at His Age – Until His Past Caught Up With Them

Why You Keep Waking Up With a Dry Mouth
🦴 Hip Pain: What Does It Mean? Common Causes & When to Seek Help

You see Lipton tea, cloves, and ginger?
