12 Common Foot Problems and How to Manage Them
The Human Foot: Tough, Complex—and Easily Overworked
Each human foot contains 26 bones, 33 joints, and 100+ muscles, ligaments, and tendons. These fibrous tissues hold the moving parts together, and the soles also pack more sweat glands than any other body area.
From an evolutionary standpoint, the foot is remarkable: it bears hundreds of tons of cumulative force every day as you walk, run, and pivot. The American Academy of Orthopaedic Surgeons (AAOS) estimates that every mile you walk loads up to 60 tons of pressure on each foot. Your toes, heel, arch, and forefoot coordinate like a small machine to move you efficiently.
That workload also makes feet especially vulnerable. According to podiatrist Saylee Tulpule, DPM (Maryland and Washington, D.C.), many common problems—hammertoes, blisters, bunions, corns and calluses, claw and mallet toes, ingrown toenails, toenail fungus, and athlete’s foot—stem from neglect, poor footwear, or simple wear and tear.
Good shoes matter. “Because our body weight rests on our feet, it’s essential to choose durable footwear with support and cushioning,” says Tulpule. Just as important: don’t ignore foot pain. It can flag broader health issues. Gout often begins in the foot, and diabetes may present with numbness, burning, coldness, or thin skin on the feet—possible signs of vascular or nerve problems that merit medical evaluation.
Below are common foot issues, how to recognize them, and what helps.
1) Athlete’s Foot (Tinea Pedis)

What it is: A contagious fungal infection that thrives in warm, moist, dark environments (think sweaty socks and tight shoes). It often affects between the toes and the soles.
Symptoms: Itchy, burning, peeling or scaly rash; color can look red, purple, gray, or white depending on skin tone. A mild odor may occur.
Self-care & prevention
-
Keep feet clean and dry; change socks and shoes regularly.
-
Avoid going barefoot in locker rooms, pools, and communal showers.
-
Prefer synthetic or wool-blend socks that wick moisture; minimize cotton.
-
Use OTC antifungal creams, sprays, or powders; disinfect shoes with antifungal sprays.
When to see a doctor: If symptoms persist 3–4 weeks despite treatment, or if you have diabetes/immunosuppression.
2) Blisters

Cause: Friction between skin and footwear.
What to do
-
Wear properly fitted shoes and moisture-wicking socks to prevent.
-
Do not pop a blister intentionally. Cover with a bandage and let it deflate naturally.
-
If it opens, apply OTC antibiotic ointment, re-cover, and reduce friction.
See a clinician: If you have diabetes, poor circulation, signs of infection (pus, spreading redness), or persistent pain.
3) Bunions (Hallux Valgus)

What it is: A bony prominence at the base of the big toe; the toe drifts toward the others.
Contributors: Genetics, arthritis, past trauma, and tight/narrow shoes or high heels.
Care
-
Rest, ice, OTC pain relievers.
-
Wide toe-box shoes, pads/orthotics, and range-of-motion exercises.
-
Surgery may be recommended if conservative measures fail to relieve pain or restore function.
4) Corns and Calluses

Cause: Repeated rubbing/pressure—often from ill-fitting shoes.
Where they form
-
Corns: tops/sides of toes or between toes.
-
Calluses: weight-bearing areas—heels, balls of feet, and toe edges.
Home care
-
Soak in warm water, then gently reduce thickened skin with a pumice stone/emery board.
-
Moisturize to soften; avoid over-trimming (risk of bleeding/infection).
Professional care: If painful, recurrent, or if you have diabetes/neuropathy, see a podiatrist for padding, offloading, or debridement.
5) Plantar Fasciitis

What it is: Inflammation or microtearing of the plantar fascia, the band connecting heel to forefoot. Classic symptom: stabbing heel pain, often worse on first steps in the morning.
Risks: Overuse (runners), prolonged standing, limited ankle mobility, tight calves, unsupportive shoes, or higher body weight.
Relief
-
Ice, short-term NSAIDs (if appropriate), rest.
-
Supportive shoes/insoles; night splints to gently stretch fascia/calf.
-
Physical therapy for calf/plantar fascia stretches and loading exercises.
Prognosis: Most improve without surgery; <10% need operative care.
6) Hammertoes

What it is: The middle joint of the toe bends upward, making the toe look like a hammer (usually the 2nd–4th toes).
Causes: Tight shoes, structural imbalance, congenital factors, diabetes, or neuromuscular disease.
Management
-
Early: roomy footwear, pads/orthotics, toe-stretching.
-
Advanced/fixed deformity: surgical correction may be necessary.
-
Watch for corns/calluses where the toe rubs the shoe.
7) Mallet Toes

What it is: Downward bend at the joint nearest the tip of the toe—often the second toe.
Causes: Tight shoes, injuries, arthritis.
Treatment: Shoe inserts, larger toe box, stretch/strengthen toe muscles; surgery if rigid or painful despite conservative care.
8) Claw Toes

What it is: The toe base joint extends upward, while the middle and end joints flex downward, creating a claw-like shape.
Causes: Tight footwear or nerve damage (e.g., from diabetes) weakening intrinsic foot muscles.
Care: Roomy shoes, protective padding, exercises; surgery if fixed and painful.
9) Gout

What it is: Uric acid crystals deposit in joints, commonly first the big-toe joint, causing abrupt redness, heat, swelling, and severe pain.
Prevention & management
-
Limit red meat, certain seafood, alcohol (especially beer); maintain healthy weight.
-
During flares: hydration, rest; see your clinician about anti-inflammatories and longer-term urate-lowering therapy if attacks recur.
-
Treat the disease, not just the pain—untreated gout can affect other joints and restrict motion.
10) Ingrown Toenails

Prevention: Cut nails straight across, not too short; avoid shoes that squeeze the toes.
Home care: Soak in warm water 15–20 minutes a few times daily; gently place cotton/dental floss under the edge to lift it as it grows.
Medical care: If signs of infection, severe pain, recurrent cases, or if you have diabetes/poor circulation, see a clinician; partial nail removal and topical antibiotics may be advised.
11) Toenail Fungus (Onychomycosis)

How it starts: Nail-skin junction gets disrupted (pedicures, tight shoes, repetitive impact from running/hiking). Fungi love the warm, moist shoe environment.
What you’ll see: Thickened, brittle, discolored, or distorted nails; it can spread to other nails.
Treatment: Topical antifungals, oral antifungals, or combination; persistent cases may need nail removal plus antifungals. Recurrence is common; prevention (dry feet, shoe disinfection, protective footwear in communal areas) is key.
12) Hallux Rigidus (Stiff Big Toe)

What it is: The most common foot arthritis, affecting the big-toe base joint; more frequent after age 30 and somewhat more common in women.
Symptoms & causes: Pain and stiffness while walking or even standing. Triggers include repetitive overload (sports, frequent squatting), or inflammatory diseases like rheumatoid arthritis or gout.
Management: Roomy shoes and stiff-soled/rocker-bottom inserts to limit joint motion, NSAIDs for pain/swelling, corticosteroid injections for flares. If pain or stiffness significantly limits life, surgical options can restore function.
Smart Foot-Care Habits (Everyday Checklist)
-
Footwear: Choose supportive, well-fitted shoes with adequate toe room; replace worn-out pairs.
-
Socks: Wear moisture-wicking socks; change if damp.
-
Skin & nails: Moisturize heels and cuticles; trim nails straight across.
-
Hygiene: Dry well between toes; use antifungal powder if prone to sweating.
-
Training loads: Increase activity gradually; cross-train to reduce repetitive stress.
-
Listen to pain: Persistent pain, numbness, burning, color/temperature changes, or nonhealing sores warrant prompt medical attention—especially if you have diabetes, vascular disease, or neuropathy.
Bottom Line
Your feet are biomechanical powerhouses—but they’re also first in line for overuse. Support them with smart footwear, good hygiene, and early attention to symptoms. Doing so not only prevents many common problems but may also uncover systemic health issues early, when treatment is most effective.
News in the same category

Why Do I Cough When Taking a Deep Breath?

Taking the Stairs Could Help You Live Longer

Purple Veins on Your Legs: When to Worry

Signs Your Cortisol Is Dangerously High

The Sleep Saboteur: The One Thing You Should Never Do When You Wake Up at Night
Nightly Habits That Could Increase Your Risk of Stroke

11 Secret Baking Soda Tricks for Women That Will Change Your Life!

World’s deadliest cancer: 8 early warning signs every older adult should know
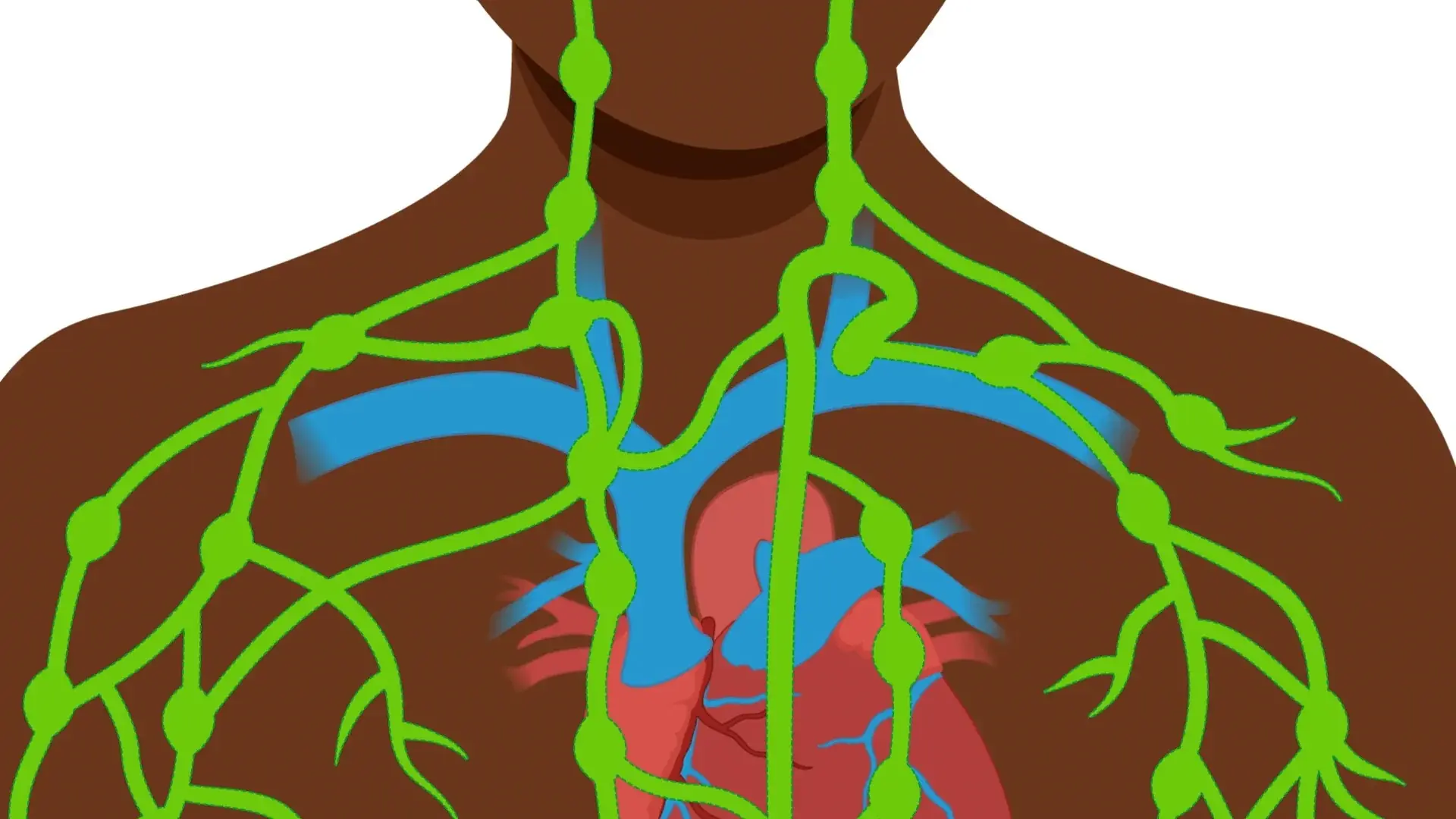
The Fastest Natural Way to Cleanse Your Lymphatic System That No One Talks About

5 Potential Risks of Eating Avocados You Should Know

Top Essential Oils That Instantly Ease Pain and Inflammation
These Are the Early Warning Signs of Diabetes No One Talks About
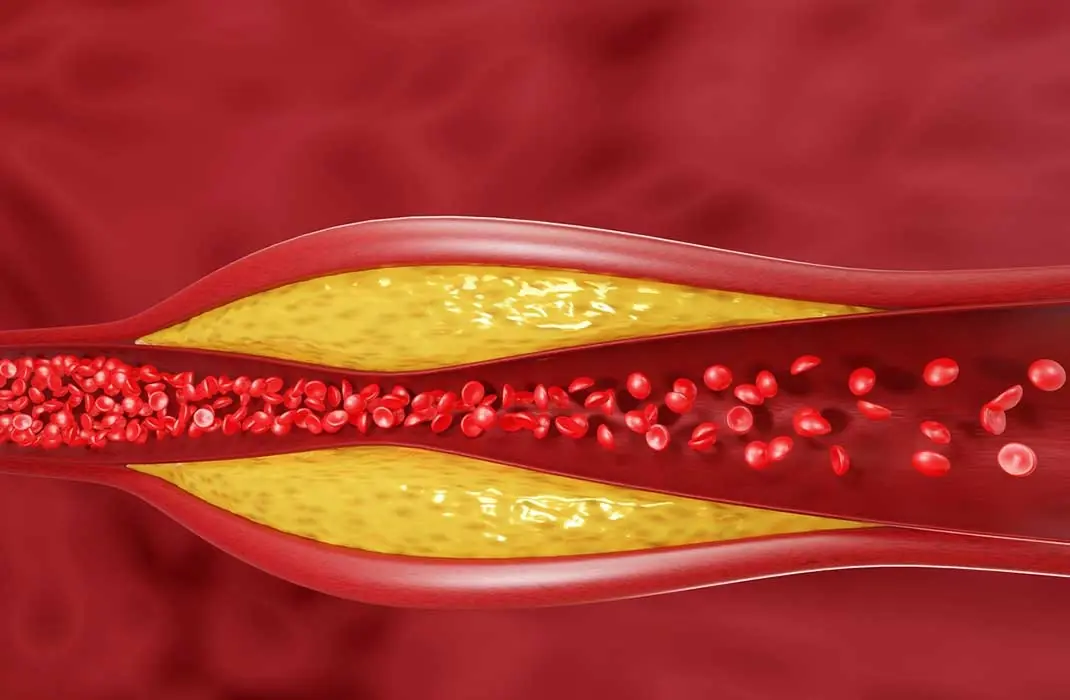
Cholesterol Meds Linked With Heart Attacks, Fast Aging And Brain Damage. Eat These Foods Instead

Food Suddenly Tastes Different? Here’s What Your Body’s Trying to Tell You

Is Your Gel Manicure To:xic?
Understanding Eye Floaters: Causes and When to Seek Help

9 Convincing Reasons to Consume More Dates

Early-Stage Cancer May Not Hurt at First, But If You Notice These 8 Signs When Using the Bathroom, See a Doctor Immediately: Don’t Be Negligent
News Post

Firefighter reveals Princess Diana's last four words before she died
Nearly three decades after Princess Diana’s tragic death, a firefighter who held her hand in her final moments has shared what she said before losing consciousness. His emotional recollection sheds new light on one of the most heartbreaking nights in mo
Fans defend The Rock after he revealed 'slim' look which has left people extremely concerned
Dwayne “The Rock” Johnson stunned audiences with a dramatically leaner appearance at the Venice Film Festival, sparking a wave of divided reactions online. While some fans voiced concern for his health, others rushed to defend the Hollywood icon, remi

Elon Musk's daughter shares very honest message after cutting ties with billionaire dad who claimed she was dead
Vivian Wilson, the estranged daughter of tech mogul Elon Musk, has once again spoken out about life after severing ties with her world-famous father. In a rare and unfiltered message, she shed light on her personal struggles, her independence, and the rea

California hospital staff fired following 'dehumanizing' TikTok ridiculing their patients
What began as a short social media clip has ended in a scandal that shook a California healthcare network. A group of hospital workers recorded a TikTok mocking their patients—an act described as “dehumanizing”—and have now all been dismissed foll

Before-and-after images show effects space had on NASA astronauts after 9 months
What was supposed to be a short visit turned into nearly a year away from Earth. Now, newly released before-and-after images of two NASA astronauts show just how profoundly nine months in space can reshape the human body.

NASA just took the closest-ever images of the sun, and they are incredible
For the first time in history, humanity has peered closer into the blazing heart of our star than ever thought possible. NASA’s Parker Solar Probe has delivered astonishing images and video of the sun’s surface and atmosphere, revealing mysteries that

Rice Water: The “Liquid Gold” in Your Home That Most People Forget to Use

The Shocking Truth Behind “Bleach” Stains on Underwear – What Your Body Is Really Telling You
Many people are startled when they notice pale or bleach-like patches on their underwear and immediately assume something must be wrong. But far from being a sign of poor hygiene, this natural occurrence is actually one of the strongest indicators of a he
There Is One Sound A Person Makes That Means They Have Less Than 24 Hours To Live
As the body approaches its final hours, loved ones may hear a sound known as the “death rattle,” a sign that often causes deep concern. Though unsettling, this natural process is not painful for the person and understanding it can bring comfort to fam

Add This Simple Ingredient When Mopping – Your Floors Will Shine Like New and Stay Clean All Week!
5 Delicious Eating Habits That Put the Whole Family at Risk of C:ancer – Extremely Dangerous and Should Be Avoided Immediately

Be careful — one single action at the airport could ruin your en:tire life.
Condolences to those who are using these 4 types of electric kettles: Throw them away while you still can, thousands of people have already developed c:ancer.
How Magnesium Keeps Your Heart Rhythm Healthy

Why Do I Cough When Taking a Deep Breath?

Taking the Stairs Could Help You Live Longer

Purple Veins on Your Legs: When to Worry

Man develops 'pork worms' in his brain after years of doing this specific cooking habit

Signs Your Cortisol Is Dangerously High