Looks like a infection between my toes. Can’t get medical advice for now. Any over-the-counter remedies?

Fungal infections between the toes, most commonly known as athlete’s foot or tinea pedis, are caused by dermatophytes—a group of fungi that thrive in warm, damp environments. These infections are especially common among people who wear tight or non-breathable footwear for long periods or whose feet sweat frequently. Because the condition is contagious, it can easily spread through skin-to-skin contact or by touching contaminated surfaces such as gym floors, locker rooms, swimming pool areas, or shared showers.
Although toe fungal infections are rarely serious, they can be uncomfortable, persistent, and frustrating if not treated properly. Understanding the symptoms, causes, and treatment options is key to managing the condition effectively and preventing recurrence.
Common Symptoms of Fungal Infections Between the Toes
The symptoms of a fungal infection between the toes can range from mild to severe, depending on how advanced the infection is. Typical signs include itching, burning, or stinging sensations, especially after removing shoes and socks. The affected skin may become red, flaky, scaly, or cracked, and in some cases, painful fissures may develop.
Blisters or oozing skin can also appear in more severe cases. The space between the toes is particularly vulnerable because moisture tends to accumulate there, and limited air circulation creates ideal conditions for fungal growth. If left untreated, the infection may spread to other areas of the foot or even to the toenails.
Causes and Risk Factors
Several factors increase the likelihood of developing a fungal infection between the toes. These include wearing damp socks or shoes, failing to dry the feet properly after bathing, and walking barefoot in communal environments. People with weakened immune systems, diabetes, or circulation problems are at greater risk and may experience more severe or recurring infections.
Athletes and individuals who engage in frequent physical activity are also more susceptible due to increased sweating and the possibility of small cuts or abrasions that allow fungi to enter the skin. Poor foot hygiene and prolonged use of tight-fitting footwear further raise the risk.
Over-the-Counter Treatments for Toe Fungal Infections
Mild to moderate fungal infections between the toes can often be treated successfully with over-the-counter (OTC) antifungal products. These include creams, ointments, powders, and sprays containing active ingredients such as clotrimazole, miconazole, terbinafine, or tolnaftate.
These medications work by stopping fungal growth and gradually eliminating the infection. Most OTC treatments are effective when used consistently and according to the instructions provided on the packaging.
How to Properly Apply Antifungal Creams and Ointments
Before applying any antifungal cream or ointment, it is essential to wash the feet thoroughly and dry them completely, especially between the toes. Moisture can reduce the effectiveness of treatment and encourage fungal growth.
Apply a thin, even layer of the medication to the affected area and slightly beyond its edges, usually once or twice daily. Even if symptoms improve quickly, treatment should continue for the full recommended duration to ensure the fungus is completely eliminated and to prevent recurrence.
The Role of Antifungal Powders and Sprays
Antifungal powders and sprays are particularly useful for managing moisture and preventing reinfection. They help keep the feet dry and can be applied both to the skin and inside shoes. These products are often used alongside creams or ointments to enhance treatment effectiveness.
Regular use of powders or sprays can be especially helpful for people who sweat heavily or wear closed footwear for long hours.
Home Remedies and Natural Approaches
Some individuals choose to try home remedies or natural alternatives to manage fungal infections between the toes. Common options include soaking the feet in diluted vinegar or saltwater, applying tea tree oil, or using garlic due to its natural antifungal properties.
While some people may experience symptom relief, the effectiveness of these remedies varies, and they are not always supported by strong scientific evidence. Natural treatments should be used cautiously and should not replace proven antifungal medications, especially in persistent cases.
Preventing Future Toe Fungal Infections
Prevention plays a crucial role in avoiding repeated fungal infections. Good foot hygiene is essential—wash feet daily, dry them thoroughly, and change socks regularly. Moisture-wicking socks and breathable shoes help reduce sweat buildup and limit fungal growth.
Avoid walking barefoot in public areas, disinfect shoes regularly, and consider using antifungal sprays or powders as a preventive measure, particularly if you are prone to infections.
When to See a Healthcare Professional
If OTC treatments fail to improve symptoms after two to four weeks, or if the infection worsens, spreads, or becomes painful, medical advice should be sought. Persistent infections may require prescription-strength antifungal medications or further evaluation to rule out other skin conditions.
People with diabetes, circulation problems, or compromised immune systems should consult a healthcare provider early, as fungal infections can lead to complications if untreated.
Conclusion: Managing Toe Fungal Infections Successfully
Fungal infections between the toes are common but manageable with the right approach. Early treatment, consistent use of antifungal products, and proper foot care can effectively clear the infection and reduce discomfort. Equally important are preventive measures that help keep feet clean, dry, and protected.
When treated promptly and appropriately, most toe fungal infections resolve without complications. However, if symptoms persist or recur, professional medical guidance is the safest and most effective path to long-term relief.
News in the same category

Soaking bananas in vinegar: 4 amazing uses recognized by experts, everyone loves it

Ants, cockroaches, mosquitoes… will gradually leave their homes thanks to these tips

Ripe bananas spoil quickly after being bought; preserve them this way so they stay bright yellow, fragrant, and firm for a whole week

Don't do these 5 things in the morning if you don't want your cancer cells to grow rapidly.
Unbelievable: Adding a few drops of menthol oil to onions is ten times more effective at repelling mosquitoes and promoting better sleep than pure gold.

How to preserve cilantro so it stays fresh, vibrant, and fragrant for up to a month.

How to use menthol balm to effectively and safely eliminate odors in your home: An inexpensive tip every household needs.
That’s brand new info

You are doing it all wrong. Here's the right way to use vapo rub

Soaking garlic in honey – a remedy more precious than gold, preventing a multitude of diseases
This type of leaf is called ginseng, detoxifying, and liver-cooling: it grows when you plant a cutting

6 ways to use menthol oil to repel mosquitoes effectively: Mosquitoes won't dare come near, and your house will smell fresh

Eating plenty of these 5 vegetables during the cold season helps boost immunity and effectively fight inflammation
Discovery of a substance that triples the risk of cirrhosis: Present in many household items

I keep finding bright orange dust collecting along my baseboards, and I can’t get pest control out anytime soon. What could this even be?
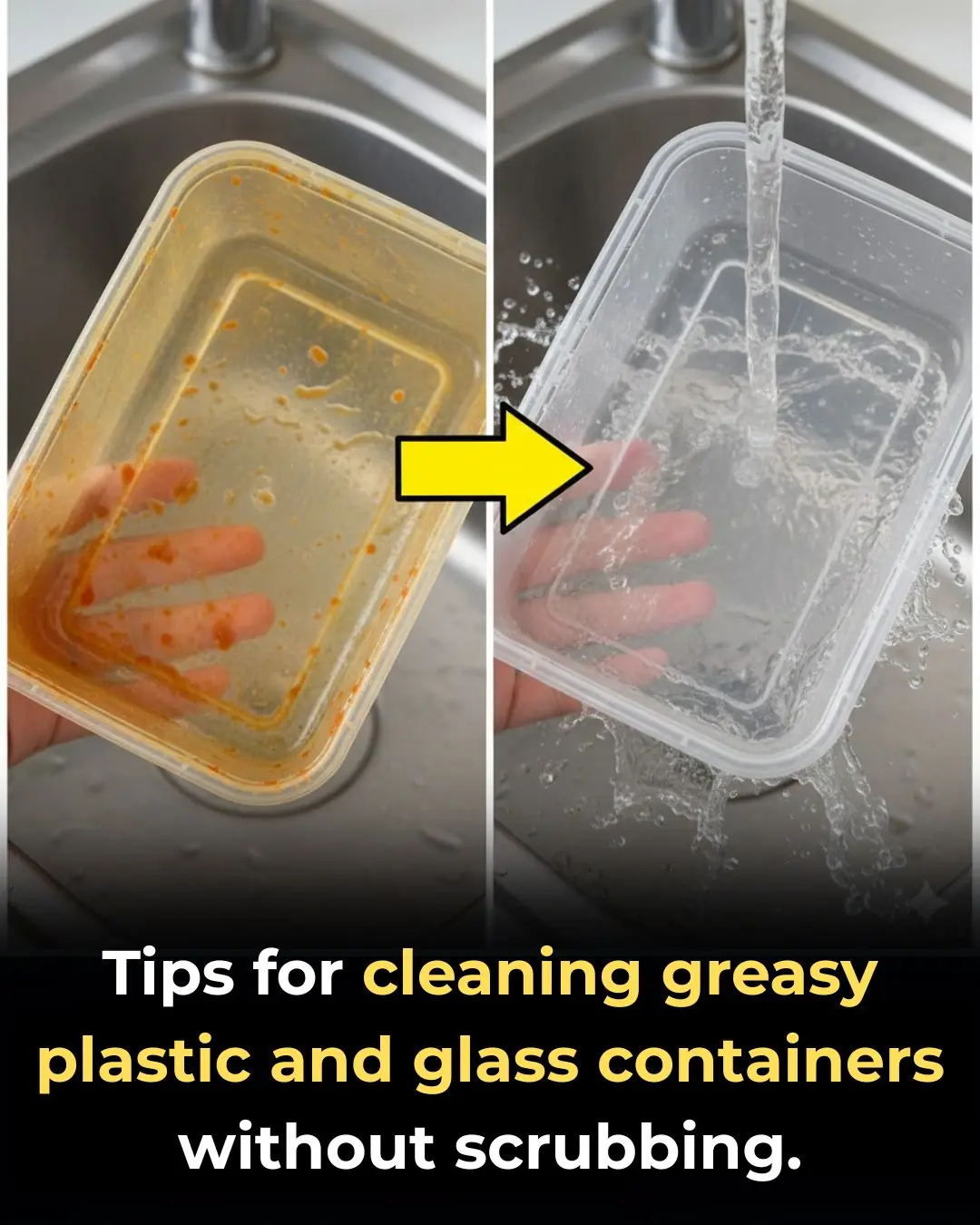
Tips for cleaning plastic containers and glass containers full of grease, without scrubbing

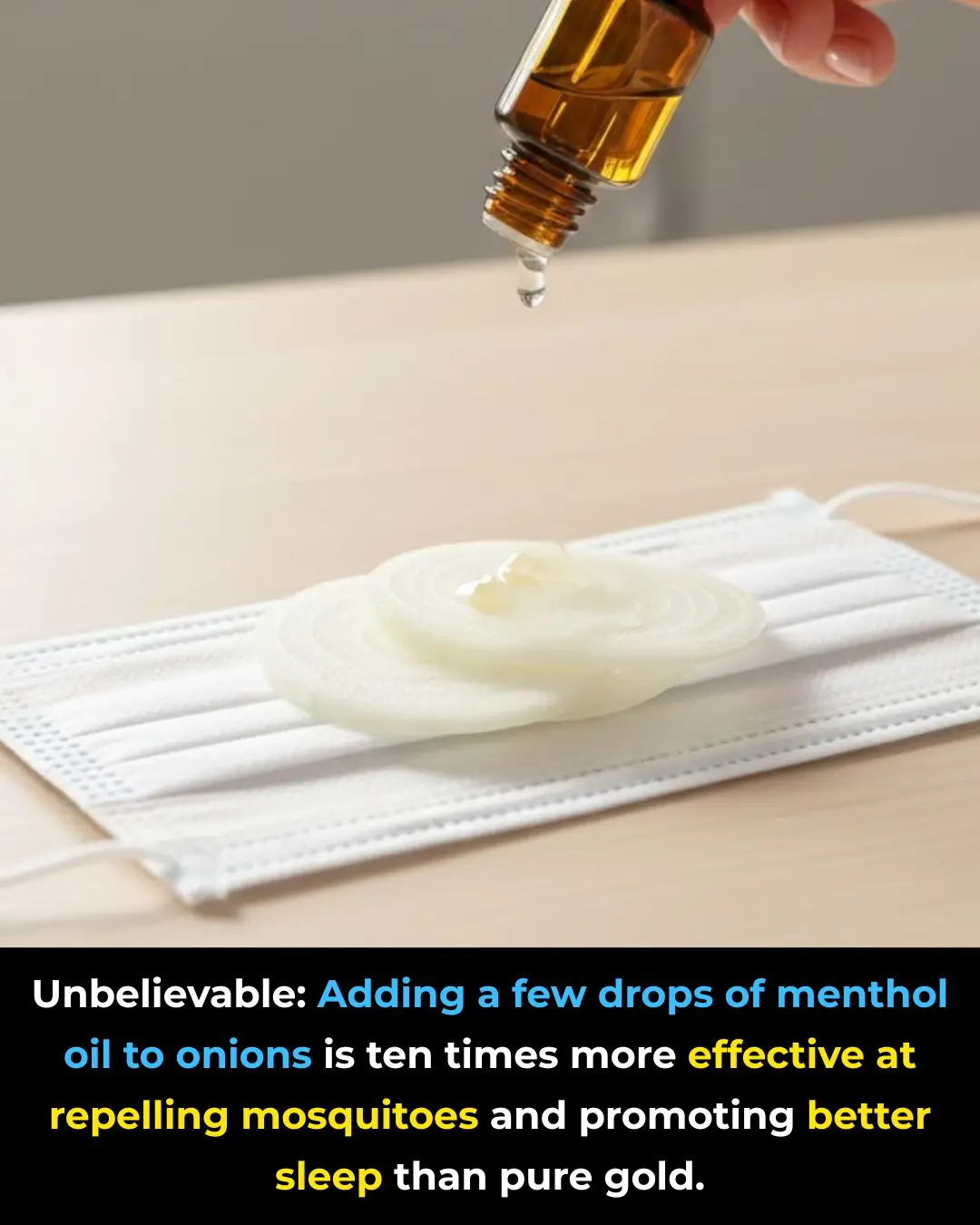
Purple blotches keep showing up on my arms. Doctor isn’t available for weeks. What should I do?

Ugh, got a crusty looking bump on my elbow. Can I remove this myself at home, or do I need to see a doc? Looks so bad
News Post
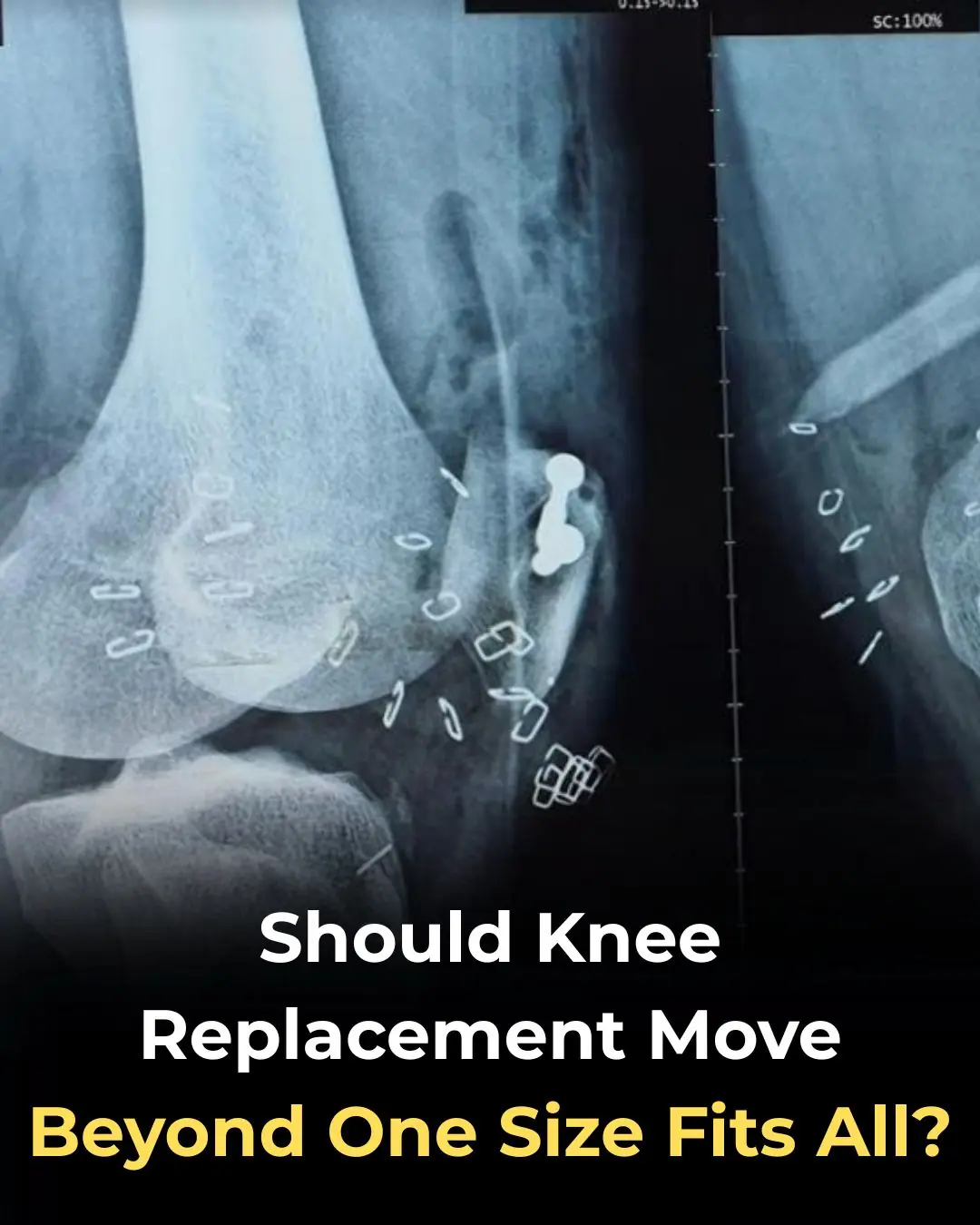
Should Knee Replacement Move Beyond One-Size-Fits-All Alignment?
Shingles Vaccination Associated With Reduced Cardiovascular and Dementia Risk Despite Breakthrough Infections
Early Use of Glucocorticoids Reduces Mortality in Community-Acquired Pneumonia in Low-Resource Settings

At thirty-seven, I walked into the Grand Westbrook Hotel in downtown Chicago wearing a simple black dress and a wool coat I’d owned for years.

I worked abroad for 5 years to buy a house for my mother – When I returned, meeting my mother was not like I imagined.

THE MORNING AFTER THE WEDDING, MY HUSBAND AND I WERE ALREADY PACKING FOR HONEYMOON WHEN I GOT A CALL FROM THE REGISTRY OFFICE: ‘SORRY, WE CHECKED YOUR DOCUMENTS AGAIN… YOU NEED TO COME IN & SEE THIS IN PERSON. COME ALONE — AND DON’T TELL YOUR HUSB

I quit my career because my husband said, “A real wife stays home.” I did—ten years of silence and sacrifice. Then he filed for divorce. His lawyer smirked, “She has no skills.

“Just the thought of sleeping with that fat pig makes me sick.” I heard my son-in-law say this about my daughter the night before their wedding. He and his friends laughed like it was nothing… But in the end, I was the one who had the last laugh.

I Was Seven Months Pregnant, Carrying Groceries Up Three Flights Of Stairs While My Husband Sat On The Couch Playing Video Games.
Boiling chicken without tap water
8 Early Signs of Diabetes That Many People Overlook

Bad Habits After Washing Clothes That Can Make the Whole Family Sick! Many People Overlook This Detail

Soaking bananas in vinegar: 4 amazing uses recognized by experts, everyone loves it
How do people who take naps and those who don't? Experts reveal surprising truth

Ants, cockroaches, mosquitoes… will gradually leave their homes thanks to these tips

Ripe bananas spoil quickly after being bought; preserve them this way so they stay bright yellow, fragrant, and firm for a whole week
Of particular note, these four unusual pains occurring every morning may be a warning sign of a tumor in the body

Don't do these 5 things in the morning if you don't want your cancer cells to grow rapidly.
Unbelievable: Adding a few drops of menthol oil to onions is ten times more effective at repelling mosquitoes and promoting better sleep than pure gold.
