mRNA Vaccines Show Early Evidence of Slowing Cancer Progression
Scientists have now offered the first strong evidence that messenger-RNA (mRNA) vaccines — best known for preventing COVID‑19 — might also play a role in slowing cancer progression. Early studies show these vaccines can train the immune system more effectively to recognise and destroy cancer cells, thereby offering a promising new approach in oncology.
This discovery has the potential to transform cancer therapy, and to provide hope to millions of patients worldwide. By reducing or slowing tumour growth, mRNA vaccines may help improve survival rates, and enhance the effectiveness of existing cancer treatments.
Today, researchers are actively conducting clinical trials to explore the full potential of mRNA technology in cancer care. Although further studies are required to establish how broadly and consistently the benefit applies, this breakthrough marks a significant step-forward in the fight against one of the deadliest diseases globally.
The scientific community is increasingly optimistic that mRNA vaccines could soon play a critical role beyond infectious diseases, reshaping the future of cancer care.
What the research shows
The mechanism behind this concept is that mRNA vaccines provide instructions to cells to produce proteins (antigens) characteristic of either a virus or — in the cancer context — tumour-specific proteins (neo-antigens). When the immune system learns to recognise those proteins, it becomes better able to identify and attack the corresponding cells. MD Anderson Cancer Center+3Công đoàn Phòng chống Ung thư+3ScienceDirect+3
For example, one retrospective study by MD Anderson Cancer Center and University of Florida found that people with advanced lung or skin cancer who received an mRNA COVID-19 vaccine lived significantly longer when the vaccine was administered in close proximity to the start of immunotherapy. The authors suggest the vaccine acted like an “alarm bell” for the immune system, waking it up so it could better see and attack tumour cells. PBS+1
Another review published in PubMed states that more than 120 clinical trials of mRNA-based cancer vaccines have now been initiated, testing the approach in lung, breast, prostate, melanoma, pancreatic and brain cancers. While early, many of the signals are promising. PubMed+1
One concrete example: In a phase 1 trial for pancreatic cancer, a personalized mRNA vaccine (autogene cevumeran) induced tumour-specific T-cells that persisted up to four years after treatment in some patients; and those patients showed lower risk of recurrence compared with those whose immune systems did not mount a strong vaccine-induced response. Memorial Sloan Kettering Cancer Center
Why this matters
Traditionally cancer vaccines have been difficult because tumours are derived from the body’s own cells — meaning the immune system often doesn’t recognise them as “foreign.” mRNA vaccines offer a faster, more customizable method (via neoantigens) than older vaccine technologies. Công đoàn Phòng chống Ung thư+1
If mRNA injections can boost immune recognition of cancer cells, then we may not only treat cancer but also slow its progression, give patients more time and improve the outcomes of other therapies (like checkpoint inhibitors). The MD Anderson/Florida work suggests that even vaccines developed for COVID-19 may inadvertently contribute to cancer immunotherapy when properly timed. MD Anderson Cancer Center+1
Present limitations & what’s ahead
Despite the excitement, there remain important caveats:
-
Many trials are still early-phase, with small numbers of patients. Robust, large-scale evidence is still forthcoming. PubMed+1
-
Delivery of mRNA vaccines, optimisation of the immune response, avoidance of side-effects, and durable responses remain technical and clinical hurdles. ScienceDirect
-
We must determine which cancers, patient populations, and tumour-microenvironment conditions are most likely to benefit.
Researchers are designing phase III trials (or planning them) to validate whether mRNA vaccines should become part of standard care in combination with other immunotherapies. MD Anderson Cancer Center+1
Global implications for cancer care
If mRNA vaccines can be proved effective against cancer, the implications are wide-ranging:
-
They could become adjunctive therapies, used alongside surgery, chemotherapy, radiation and immunotherapy to improve outcomes.
-
They may enable more personalised cancer treatment, tailored to an individual’s specific tumour neoantigens — enhancing precision medicine approaches. Công đoàn Phòng chống Ung thư+1
-
They could help reduce treatment resistance and relapse by “priming” the immune system earlier and more robustly.
Conclusion
In summary, the evidence that mRNA vaccines might help slow cancer progression is tính mới and significant. While more evidence is needed before routine adoption in oncology, the data so far suggest an exciting new direction: vaccines not only for infection prevention but as part of the cancer-treatment arsenal. If this promise is fulfilled, we may soon see mRNA technologies playing a central role in the battle against cancer.
References (additional):
-
American Cancer Society. “mRNA Vaccines for Cancer Treatment.” 2025. Công đoàn Phòng chống Ung thư
-
“Clinical advances of mRNA vaccines for cancer immunotherapy.” Elsevier/ScienceDirect. 2024. ScienceDirect
-
“mRNA COVID vaccines may be helping some cancer patients fight tumours, researchers say.” PBS NewsHour, October 2025. PBS
News in the same category

When your non-stick pan loses its coating, don’t throw it away—do this and it will look new again
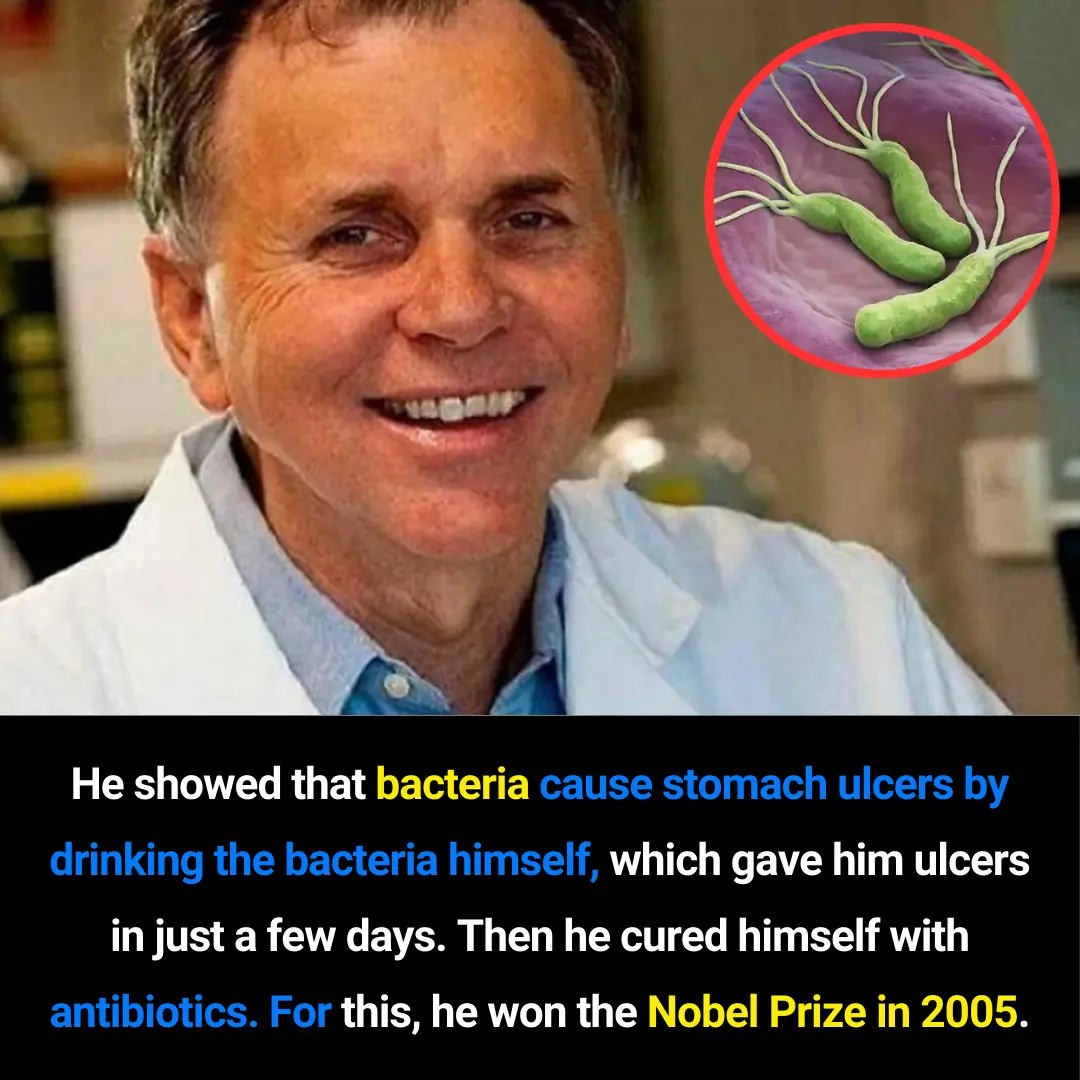
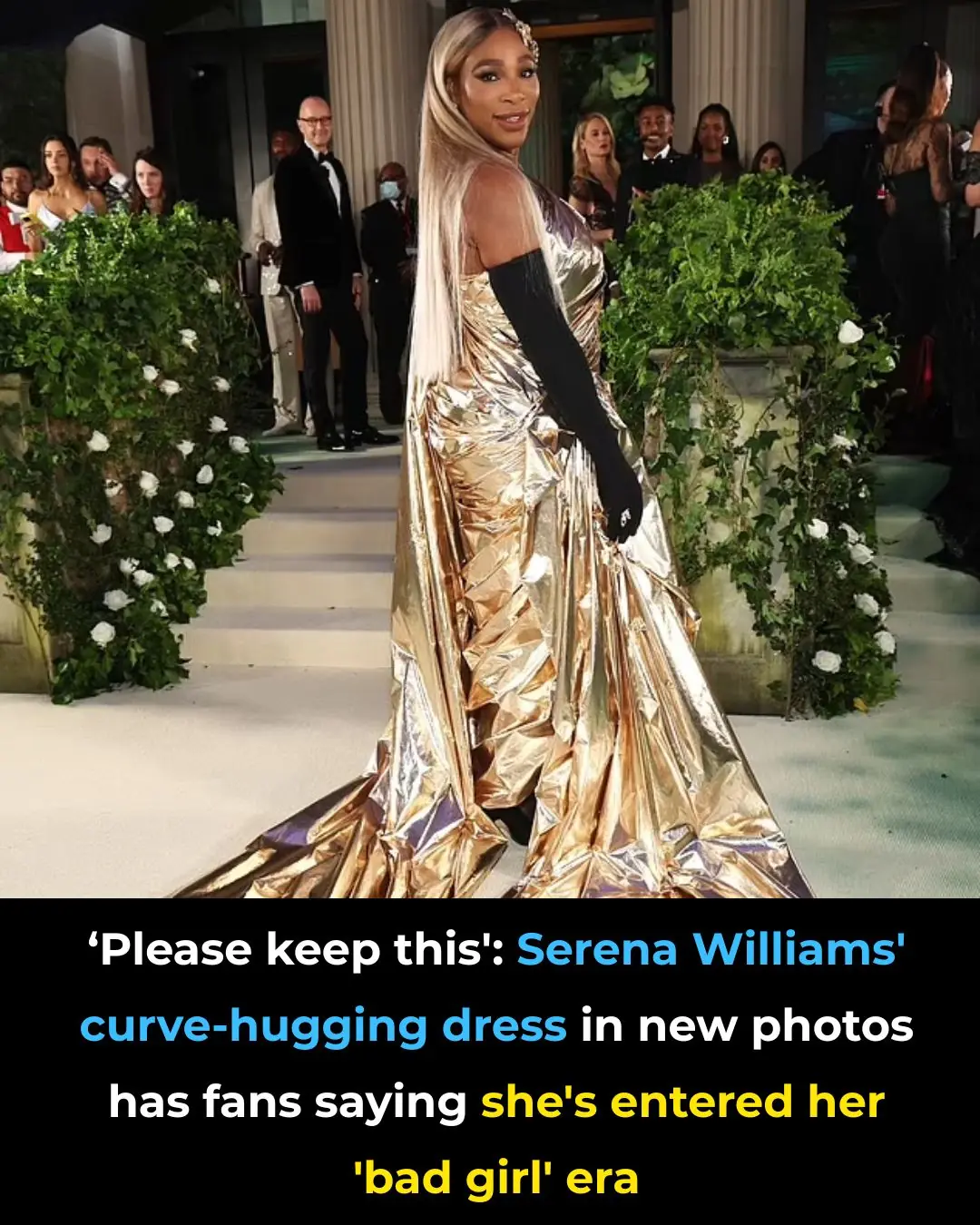
Dr. Barry Marshall: The Scientist Who Transformed Ulcer Treatment and Changed Modern Medicine

Dr. Paulo de Valdoleiros: The South African Doctor Redefining Accessible Healthcare
Gwada Negative: The 48th Human Blood Group and an Extraordinary Genetic Discovery

Incredible Survival Story: The Man Who Turned His Broken Car Into a Motorcycle in the Moroccan Desert

A Heartfelt Moment in Morristown: The Viral Message That Honors Healthcare Heroes and Celebrates Human Kindness

Boyan Slat and the Journey to Create The Ocean Cleanup: From a 16-Year-Old’s Idea to a Global Mission to Clean the Oceans

Scientists Reactivate the Brain’s Self-Cleaning System, Hinting at a Breakthrough for Alzheimer’s

The Real Crime Is Hunger: A Judge’s Moral Verdict on a Child’s Desperation
Injectable Gel Breakthrough Brings New Hope for Nerve Regeneration

Goodbye Synthetic Dyes: Doritos Join the Push for Cleaner, Transparent Ingredients
Breakthrough Research Suggests Kidney Damage May Be Reversible After All

How Intermittent Fasting Protects the Heart: New Evidence on Blood Clots and Cardiovascular Health
New Evidence Links Hepatitis C to Brain Pathways in Mental Illness

If You See a Woman Wearing a Wedding Ring On Her Pinky, Here's What It Means

Reinventing Renewable Energy: Germany Launches Compact Turbine for Off-Grid Power

Rethinking Depression: New Brain-Imaging Research Reveals It’s More Than a Chemical Imbalance

Seventeen Years Lost: How a Look-Alike Helped Free an Innocent Man
News Post
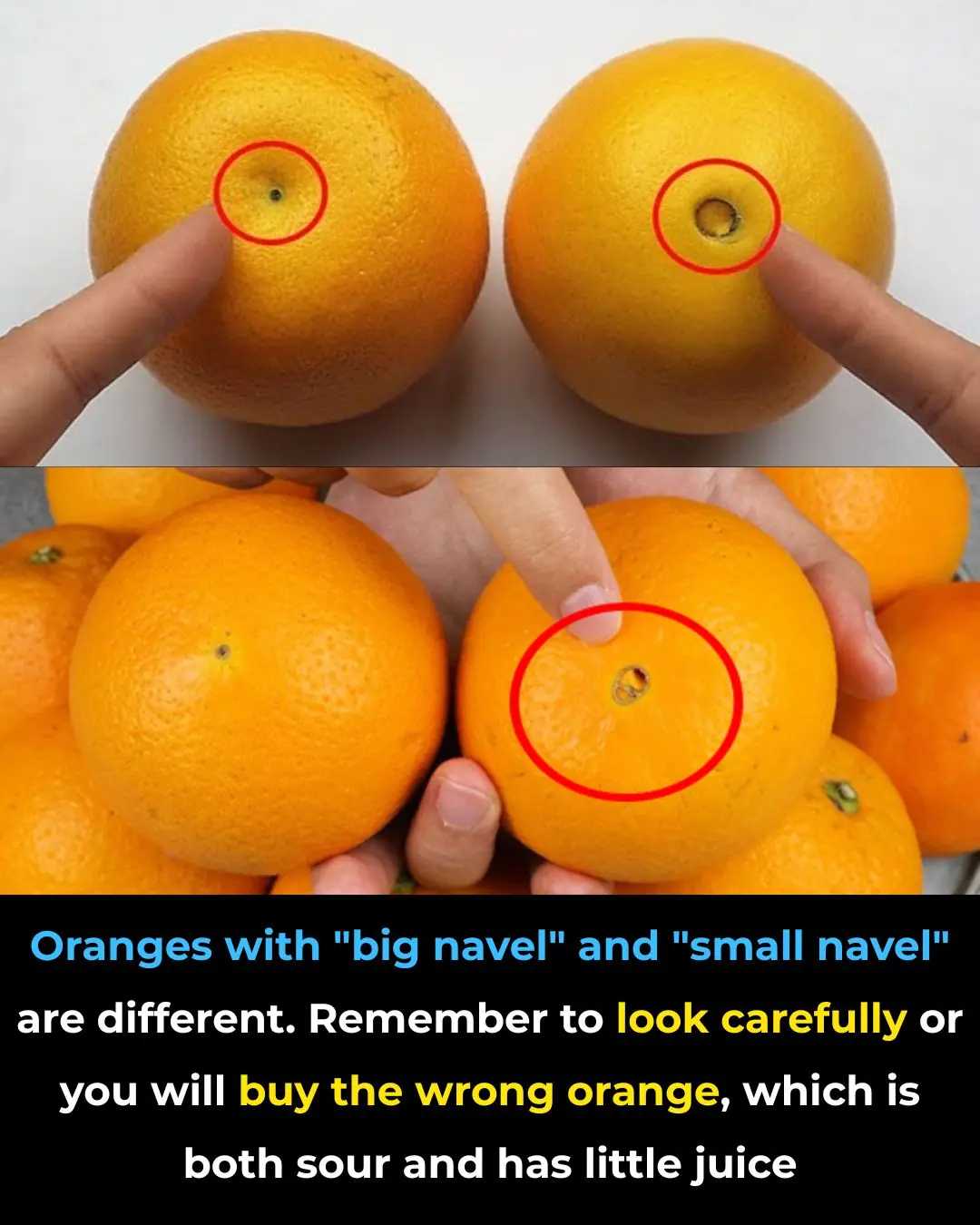
Large Navel Oranges vs Small Navel Oranges

🩺 Be Aware: If You Notice This Skin Change, It Could Be Skin Cancer — Here’s What to Look For

Gastroenterologist says this is the #1 drink for gut health
What your body does when you drink coffee every day

The 5 best supplements to soothe nerve pain and tingling

Doctor says this is the #1 supplement to take if you have arthritis
Good to know!

I had no idea

Works like a charm
Stop blood sugar spikes—enjoy carbs without the crash!

Gastroenterologist says this is the #1 drink for gut health

6 Types of Warts (Signs, Symptoms, Home Remedies, and Treatment)

Educational Summer Camp ‘HBCYouth’ Is Bringing the Next Generation to HBCU Campuses
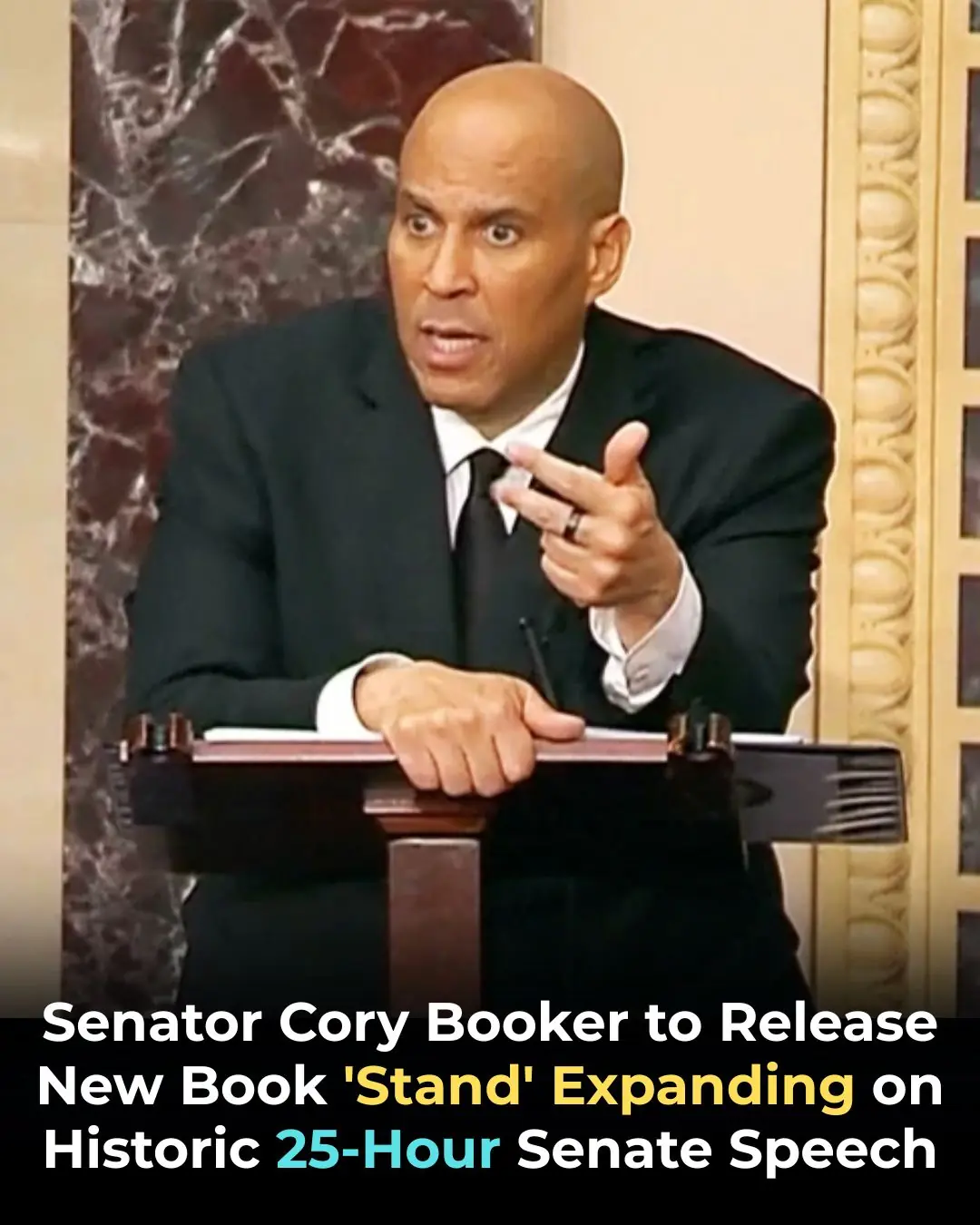
Senator Cory Booker to Release New Book ‘Stand’ Expanding on Historic 25-Hour Senate Speech

18-Year-Old Brandon Moss Makes History as Youngest Mayoral Candidate in Fairfield, Alabama

Many experts warn that this food may increase health dangers — stop eating it now!
Gentle Stretches to Relieve Sciatica Pain
Think Twice Before Putting Parchment Paper in the Oven

Georgia Teen Accepted to 53 Colleges With $1.8M in Scholarships, Inspired by Her Parents’ Legacy