New Drug That Protects the Blood-Brain Barrier Shows Promise Against Alzheimer’s Disease
Cracks in the Brain’s Defenses: A New Path in the Fight Against Alzheimer’s
It often begins so quietly you’d never notice. Picture the brain as a walled city, guarded by vigilant sentries at its gates. For most of our lives, these gates hold firm—blocking out harmful intruders while carefully admitting nutrients and oxygen needed to sustain life. But in Alzheimer’s disease, those defenses start to weaken. Tiny breaches form. Toxins slip through. The walls that once seemed impenetrable slowly crumble from within.
Today, more than 7 million Americans live with Alzheimer’s, and projections suggest that number could nearly double within 25 years. Behind these statistics are families watching memories fade, personalities change, and independence erode. For decades, research has zeroed in on one main suspect: sticky clumps of amyloid plaques that accumulate between brain cells. Even as new drugs have been developed to reduce those plaques, their benefits remain modest, their risks substantial, and their costs enormous.
Now, scientists are turning to another suspect—one that has long worked quietly in the background: the blood–brain barrier (BBB). This thin but powerful shield may prove to be just as important to protect as removing plaques. Early findings suggest that keeping the barrier strong could reduce brain inflammation, preserve memory, and delay decline. At the center of this new approach is an enzyme called 15-PGDH, which in animal studies has shown a surprising ability to dictate whether the barrier stands or falls. If these results hold true in humans, it could transform how we treat not only Alzheimer’s but also brain injuries and other conditions that raise dementia risk.
The Brain’s Hidden Guardian
Deep within the body’s most complex organ lies a security system so critical that life without it would be unrecognizable. This is the blood–brain barrier—a tightly woven mesh of cells lining the brain’s blood vessels. It acts as both sentinel and gatekeeper, deciding moment by moment what may enter and what must stay out. Nutrients, hormones, and chemical messengers pass through. Toxins, pathogens, and misdirected immune cells are turned away.
When the barrier works well, it operates with the efficiency of an experienced border agent, scanning and approving cargo in fractions of a second. But in Alzheimer’s, research shows that these guards weaken early—sometimes before the first memory lapses appear. Microscopic gaps allow inflammatory molecules and rogue immune cells to infiltrate brain tissue. The results are devastating: swelling, oxidative stress, and ultimately neuron death. Over years, these silent assaults erode the brain’s circuits much as rust eats away at steel.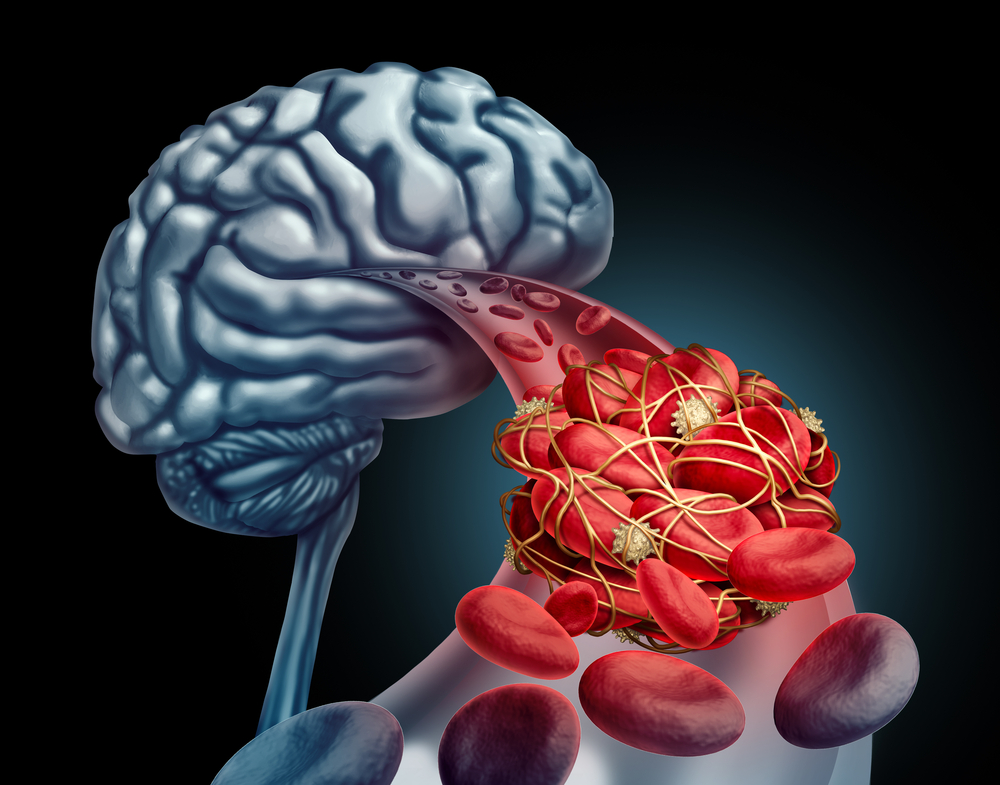
The weakening of the BBB does not occur in isolation. Aging itself makes the barrier more fragile, especially in the hippocampus, the brain’s memory center and one of Alzheimer’s first targets. Traumatic brain injury (TBI) from falls, car accidents, or repeated concussions in sports also accelerates this decline. Notably, TBI is among the strongest risk factors for later dementia, and scientists now believe that BBB damage may be the missing link.
For decades, the barrier was largely ignored in Alzheimer’s research, overshadowed by the high-profile hunt for amyloid plaques and tau tangles. But evidence is mounting that BBB collapse may not just be a side effect of the disease—it could be a driving force. Protecting it might slow, or even prevent, the destructive chain reaction that transforms subtle memory lapses into full-blown dementia.
A New Target: The Enzyme 15-PGDH
In this search for answers, researchers have identified a surprising culprit: the enzyme 15-hydroxyprostaglandin dehydrogenase (15-PGDH). Normally, 15-PGDH helps break down lipid-based compounds. But unfortunately, some of its targets are anti-inflammatory molecules that support blood vessel health and keep brain tissue calm.
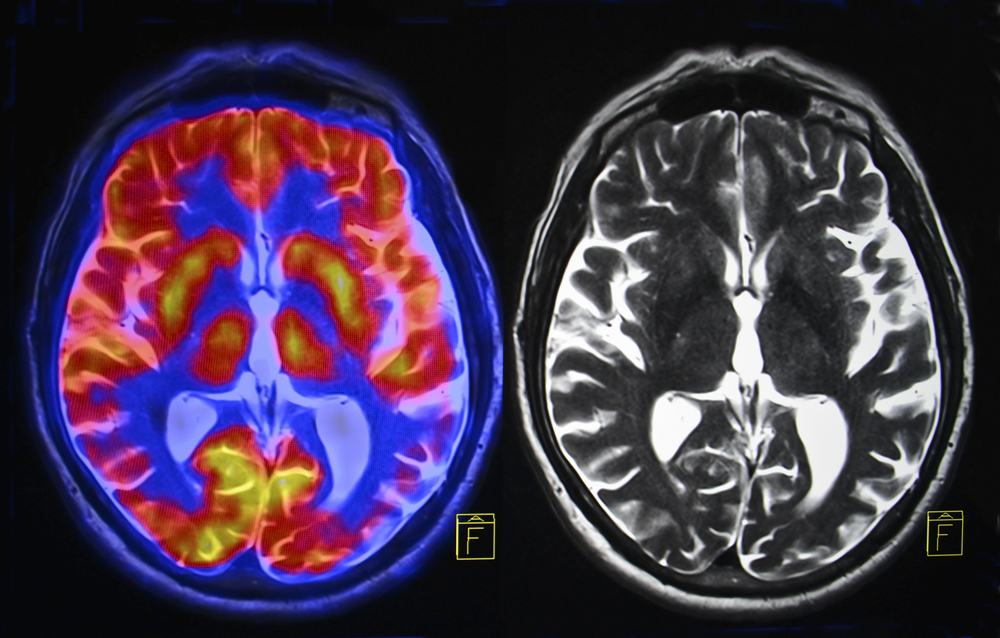
When scientists studied brain tissue from Alzheimer’s patients, as well as animal models, they found abnormally high levels of this enzyme—especially in microglia and perivascular macrophages, immune cells that cluster near the BBB. The pattern was clear: as disease severity increased, so did 15-PGDH activity. Instead of protecting the brain, these cells stripped away anti-inflammatory defenses, leaving vessel linings weaker and inflammation unchecked.
This insight raised a bold question: What if the enzyme could be blocked? Could suppressing 15-PGDH preserve barrier strength and safeguard memory?
Blocking 15-PGDH: Animal Evidence
To test this, scientists turned to the widely used 5xFAD mouse model of Alzheimer’s, which develops amyloid buildup and cognitive decline similar to humans. Beginning at two months old—before symptoms appeared—some mice received a small-molecule inhibitor called (+)-SW033291, while others received a placebo.
By six months, untreated mice showed clear memory problems. Yet treated mice performed as well as healthy controls in maze tests, remembering hidden platform locations with ease. Importantly, these gains were not due to improved motor skills or energy levels, but genuine preservation of brain function.
Genetic studies confirmed the results. Mice engineered to produce less 15-PGDH were similarly shielded from cognitive decline. Remarkably, this protection occurred without reducing amyloid plaques, directly challenging the long-standing belief that plaque removal is the only path to slowing Alzheimer’s.
Closer examination revealed that in treated mice, the BBB remained intact. In untreated animals, the barrier was visibly degraded: astrocyte “endfeet” were swollen, vessel linings had gaps, and immune proteins had leaked into brain tissue. Blocking 15-PGDH preserved structure, reduced oxidative stress, and supported the survival of newborn neurons in the hippocampus.
Even beyond Alzheimer’s, the findings held. In TBI models, mice treated with the inhibitor within 24 hours showed no typical memory deficits and avoided the BBB breakdown that often follows head trauma.
Where This Fits Into the Bigger Picture
For decades, the amyloid hypothesis has dominated Alzheimer’s research, spawning costly antibody drugs such as lecanemab and donanemab. While these treatments can reduce plaques and sometimes slow decline, they carry serious risks like brain swelling and bleeding, require frequent infusions, and work best only at the earliest stages.
By contrast, 15-PGDH inhibition represents a different philosophy—not attacking what has already invaded but fortifying the defenses from the start. This strategy may prove effective not only for amyloid-driven disease but also for cases influenced by tau tangles, vascular issues, or chronic inflammation.
The implications are far-reaching:
-
Combination therapies may emerge, pairing BBB protection with amyloid-clearing drugs, much as cancer care combines multiple approaches.
-
Prevention strategies could become possible, protecting high-risk individuals (such as those with TBI or strong family histories) before symptoms begin.
-
Early detection tools, such as new blood-based biomarker tests, may identify candidates for BBB-protective treatment long before memory loss sets in.
What It Could Mean for Patients and Families

If the benefits seen in animals translate to humans, 15-PGDH inhibition could dramatically change the Alzheimer’s landscape. By keeping the blood–brain barrier intact, patients might retain independence longer, continue working, engage socially, and preserve their sense of self for years beyond current expectations.
The impact would ripple outward. Alzheimer’s reshapes the lives of caregivers—currently about 12 million Americans, many of whom experience overwhelming stress and financial strain. A therapy that delays decline could ease that burden, allowing families more time together with less disruption. Economically, slowing progression could save billions annually in care costs, both for families and public health systems.
Perhaps most exciting, BBB protection might also help those not yet showing symptoms—older adults with head trauma histories, or people whose biomarker tests reveal early warning signs. Shifting treatment from late-stage reaction to early prevention could redefine how we approach brain health altogether.
Of course, challenges remain. Human trials must confirm safety, establish dosage, and demonstrate long-term benefit. But for families weary of treatments offering only incremental relief, the possibility of strengthening the brain’s defenses is a welcome new direction.
Holding the Line
Alzheimer’s has long been portrayed as a battle fought inside the brain, against plaques, tangles, and memory’s slow erosion. But the story of 15-PGDH reframes the fight: perhaps the most powerful move is not chasing what has already infiltrated, but holding the line at the gates.
The research is still early, but its promise is undeniable. Protecting the blood–brain barrier could slow decline, reduce the impact of brain injuries, and give patients more precious years of independence. In a field where time is the most valuable resource, even delaying symptoms by a few years could mean the difference between living freely and relying on full-time care.
The BBB has always worked quietly, almost invisibly, as the brain’s guardian. Now, at last, it is stepping into the spotlight—perhaps as one of our strongest allies in preserving the memories and identities that make us who we are.
News in the same category

Right-Side Abdominal Pain in Women: Could It Be Gallstones?

It Looks Like I Had Cosmetic Surgery”: The At-Home Routine People Use to Improve the Look of Wrinkles and Dark Spots on Hands and Arms
Everything You Need To Know About Nail Pitting
🧠 8 Strange (But Real) Signs Your Body Is Begging for More Vitamin B12 – Don’t Ignore These Red Flags

How To Identify Skin Tags and When To Remove Them
14 Visible Signs of Cancer Most Women Ignore
Reducing Prostate Discomfort Naturally with a Tomato and Garlic Drink
Never Throw Away the Avocado Seed Again — Here’s Why

Guava Leaves Benefits: The Underrated Natural Remedy You Shouldn’t Ignore 🍃💪

Herbal Tea for Swollen Legs: Natural Diuretic & Anti-Inflammatory Recipe, How to Use It, and Precautions
Avocado Seed Benefits: The Overlooked Natural Remedy for Joint and Back Pain
How Garlic and Lemon Can Gently Support Your Eye Comfort and Vision Wellness

The Overlooked Tree With Powerful Health Benefits

Discover How Incorporating Fresh Parsley into Your Daily Routine Can Support Knee Joint Comfort and Mobility Naturally

Woman reveals 3 overlooked symptoms before her stage 4 cancer diagnosis at 28
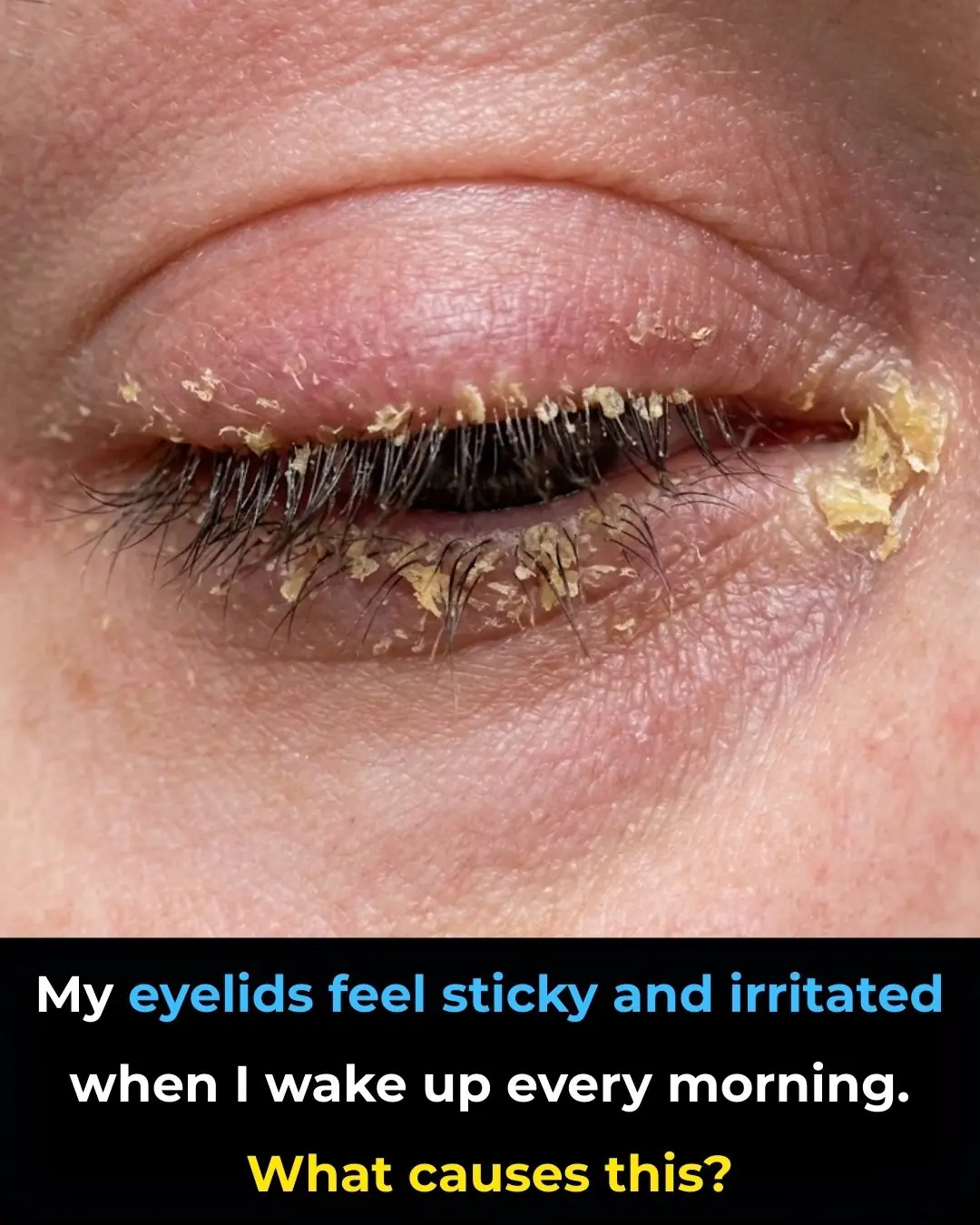
My eyelids feel sticky and irritated when I wake up every morning. What causes this?

One Spoon a Day for Stronger Vision – A Simple Daily Habit to Support Eye Comfort

A Gentle Herbal Infusion to Support Blood Sugar, Cholesterol & Circulation Naturally
Home Remedies for Varicose Veins with Onion, Garlic, and Apple Cider Vinegar
News Post

He Crashed the Wedding With a Smile—She Raised a Shield and Ended the Nightmare

“He Smashed My Violin in Front of Everyone… Then a Black Sedan Stopped the Street.”

She Accused a Cruise Dishwasher of Stealing Her Diamond Ring — What Happened Next Froze the Entire Ship

8 Foods You Should Eat Instead of Taking a Vitamin C Supplement
Right-Side Abdominal Pain in Women: Could It Be Gallstones?

It Looks Like I Had Cosmetic Surgery”: The At-Home Routine People Use to Improve the Look of Wrinkles and Dark Spots on Hands and Arms
The Last Five Dollars
The Forgotten Backpack
Everything You Need To Know About Nail Pitting
🧠 8 Strange (But Real) Signs Your Body Is Begging for More Vitamin B12 – Don’t Ignore These Red Flags

How To Identify Skin Tags and When To Remove Them
14 Visible Signs of Cancer Most Women Ignore
Reducing Prostate Discomfort Naturally with a Tomato and Garlic Drink
Never Throw Away the Avocado Seed Again — Here’s Why

Guava Leaves Benefits: The Underrated Natural Remedy You Shouldn’t Ignore 🍃💪

Herbal Tea for Swollen Legs: Natural Diuretic & Anti-Inflammatory Recipe, How to Use It, and Precautions
Avocado Seed Benefits: The Overlooked Natural Remedy for Joint and Back Pain
How Garlic and Lemon Can Gently Support Your Eye Comfort and Vision Wellness
Was He Really Jesus?