
What To Know About Chronic Kidney Failure
Chronic kidney failure, also known as end-stage kidney disease (ESKD), is the most advanced stage of chronic kidney disease (CKD). It occurs when the kidneys permanently lose nearly all their ability to function properly. At this stage, kidney function falls below 15% of normal capacity, making it impossible for the body to effectively filter waste products and excess fluid from the bloodstream.
Kidney failure is a life-threatening condition that requires ongoing medical treatment. Without dialysis, a kidney transplant, or appropriate supportive care, the buildup of toxins and fluid in the body can become fatal.
According to the Centers for Disease Control and Prevention (CDC), approximately 37 million adults in the United States are living with chronic kidney disease, and more than 800,000 people have kidney failure. While not everyone with CKD progresses to kidney failure, those who do require specialized treatment to survive and maintain quality of life.
What Happens in Chronic Kidney Failure?
The kidneys perform several essential functions, including:
-
Filtering waste and excess fluids from the blood
-
Balancing electrolytes such as sodium, potassium, and phosphorus
-
Regulating blood pressure
-
Supporting red blood cell production
-
Maintaining bone strength
When the kidneys become severely damaged over time, they lose the ability to carry out these critical roles. As a result, toxins accumulate in the bloodstream, fluid retention occurs, and multiple organ systems are affected.
Symptoms of Kidney Failure
Symptoms typically develop gradually as kidney function declines. Because early kidney disease often causes no noticeable signs, many people are unaware of the condition until it becomes advanced.
Common symptoms include:
-
Little to no urination
-
Swelling in the legs, ankles, arms, or face
-
Persistent itching or dry, discolored skin
-
Fatigue and weakness
-
Nausea and vomiting
-
Loss of appetite
-
Shortness of breath
-
Difficulty concentrating
-
Sleep disturbances
-
Muscle cramps and lower back pain
-
Frequent headaches
-
Excessive thirst
-
Foul-smelling breath (fishy or urine-like odor)
-
Easy bruising, nosebleeds, or bloody stools
-
Sexual dysfunction
These symptoms occur because waste products and excess fluids interfere with the normal function of vital organs, including the heart, lungs, brain, and digestive system.
What Causes Chronic Kidney Failure?
Kidney failure develops after years of progressive kidney damage. Several underlying conditions significantly increase the risk.
1. Diabetes
Diabetes is the leading cause of kidney failure. Chronically high blood sugar levels damage the small blood vessels in the kidneys, impairing their ability to filter waste effectively.
2. High Blood Pressure (Hypertension)
Long-term high blood pressure narrows and stiffens kidney blood vessels, reducing blood flow and accelerating kidney damage. In turn, fluid buildup further worsens hypertension, creating a harmful cycle.
3. Glomerulonephritis
This condition involves inflammation of the glomeruli—the tiny filtering units inside the kidneys. If untreated, it can lead to irreversible scarring and kidney failure.
4. Autoimmune Disorders
Conditions such as lupus nephritis and IgA nephropathy cause the immune system to attack kidney tissues, leading to progressive damage.
5. Polycystic Kidney Disease (PKD)
This inherited disorder causes fluid-filled cysts to grow in the kidneys, enlarging them and gradually reducing function over time.
Other contributing factors include recurrent kidney infections, prolonged use of certain medications, and severe urinary tract blockages.
How Is Kidney Failure Diagnosed?
Diagnosis involves a combination of medical history review, physical examination, laboratory testing, and imaging studies.
Estimated Glomerular Filtration Rate (eGFR)
The eGFR blood test is the primary tool used to assess kidney function. It estimates how much blood the kidneys filter per minute by measuring creatinine—a waste product from muscle metabolism.
-
Normal eGFR: 90 or higher
-
Moderate to severe kidney damage: Below 60
-
Kidney failure: 15 or lower for three months or more
An eGFR of 15 or below indicates that the kidneys are functioning at less than 15% of normal capacity.
Urine Tests
Urine tests help detect abnormalities such as protein leakage, blood, or waste accumulation.
Common tests include:
-
Urinalysis
-
Urine albumin-to-creatinine ratio (uACR)
-
24-hour urine collection
These tests evaluate how effectively the kidneys remove waste and maintain proper protein balance.
Imaging and Biopsy
Doctors may also order:
-
Ultrasound
-
CT scan
-
MRI
These imaging tests detect structural problems, cysts, or blockages.
A kidney biopsy may be performed to determine the exact cause of kidney damage. During this procedure, a small tissue sample is removed and examined under a microscope.
Treatment Options for Kidney Failure
There is currently no cure for kidney failure. Treatment focuses on replacing lost kidney function or managing symptoms.
Dialysis
Dialysis artificially removes waste and excess fluid from the blood.
There are two main types:
Hemodialysis:
Blood is filtered through a machine (dialyzer) at a dialysis center or sometimes at home.
Peritoneal Dialysis:
The lining of the abdomen (peritoneum) acts as a natural filter. A cleansing fluid is inserted through a catheter to absorb waste, which is later drained.
Dialysis typically requires lifelong treatment unless a transplant is performed.
Kidney Transplant
A kidney transplant surgically places a healthy donor kidney into the body. Transplants can come from living or deceased donors.
On average:
-
Living donor kidneys last 15–20 years
-
Deceased donor kidneys last 8–12 years
A successful transplant can significantly improve quality of life and eliminate the need for dialysis, though lifelong anti-rejection medications are required.
Conservative Management
Some individuals choose conservative management instead of dialysis or transplantation. This approach focuses on:
-
Managing symptoms
-
Controlling complications like anemia
-
Following a kidney-friendly diet
-
Maintaining comfort and quality of life
This option may be considered for older adults or those with additional serious medical conditions.
Can Kidney Failure Be Prevented?
Although not all cases are preventable, many risk factors can be managed.
Preventive strategies include:
-
Regular medical checkups
-
Monitoring blood sugar and blood pressure
-
Eating a balanced, kidney-friendly diet
-
Staying physically active
-
Avoiding smoking
-
Limiting excessive use of over-the-counter pain medications
Early detection of kidney disease significantly improves outcomes and can slow progression.
Related Complications
Kidney failure increases the risk of several serious health conditions, including:
-
Heart disease
-
Anemia
-
Bone disease and fractures
-
Gout
-
High potassium levels
-
Metabolic acidosis
-
Secondary hyperparathyroidism
Because the kidneys influence nearly every body system, failure can have widespread consequences.
Living With Chronic Kidney Failure
Although kidney failure is a serious condition, many people live for years with proper treatment and medical support. Dialysis and transplantation have greatly improved survival rates and quality of life.
Managing kidney failure requires:
-
Close collaboration with healthcare providers
-
Adherence to treatment plans
-
Emotional and psychological support
-
Strong family and community support systems
With appropriate care, lifestyle adjustments, and ongoing monitoring, individuals with kidney failure can maintain meaningful, productive lives despite the challenges of the condition.
News in the same category


4 Fruits You Should Eat in Moderation After 60 — And How to Enjoy Them Without Losing Muscle
15 Strange Early Signs of Liver Failure That Even Doctors Often Miss

Why Your Cat Chooses to Sleep With You

10 Conditions Ginger Can Help Manage Naturally
Harvard Doctor Reveals Foods You Should Avoid to Prevent Inflammation
Silent Cancer Signs: 3 Persistent Pains Your Body Uses as Early Warnings

Natural Remedies for Prostate Health: How to Protect Yourself from Prostate Cancer

It Looks Like I Had a Cosmetic Procedure”: The At-Home Remedy People Are Using to Improve the Appearance of Wrinkles and Dark Spots on Hands and Arms

The Best-Kept Secret of Natural Medicine Revealed! Goodbye Diabetes and High Blood Pressure
Say Goodbye to Clogged Arteries With These Powerful Foods (Better Than Aspirin!)
Old Wrinkles and Drooping Mouth? Not Anymore

The Hidden Power of Guava Leaves: Why More People Are Drinking This Tea Daily 🍃

Natural Remedy with Ginger, Onion, Garlic, Lemon, and Honey: A Homemade Recipe to Boost Immunity and Ease Colds and Coughs

My Mother Couldn’t Walk from the Pain – Until We Tried This Garlic & Clove Oil Remedy

Natural Overnight Mask to Rejuvenate Your Skin Simply and Effectively

Never Broken a Bone
🌙 If You Notice These 3 Signs at Night, Your Kidneys Are Likely in Great Shape
3 Selfish Habits of Husbands That Increase Their Wives’ Risk of Cervical Cancer – Stop Them Now Before They Harm the Whole Family
News Post
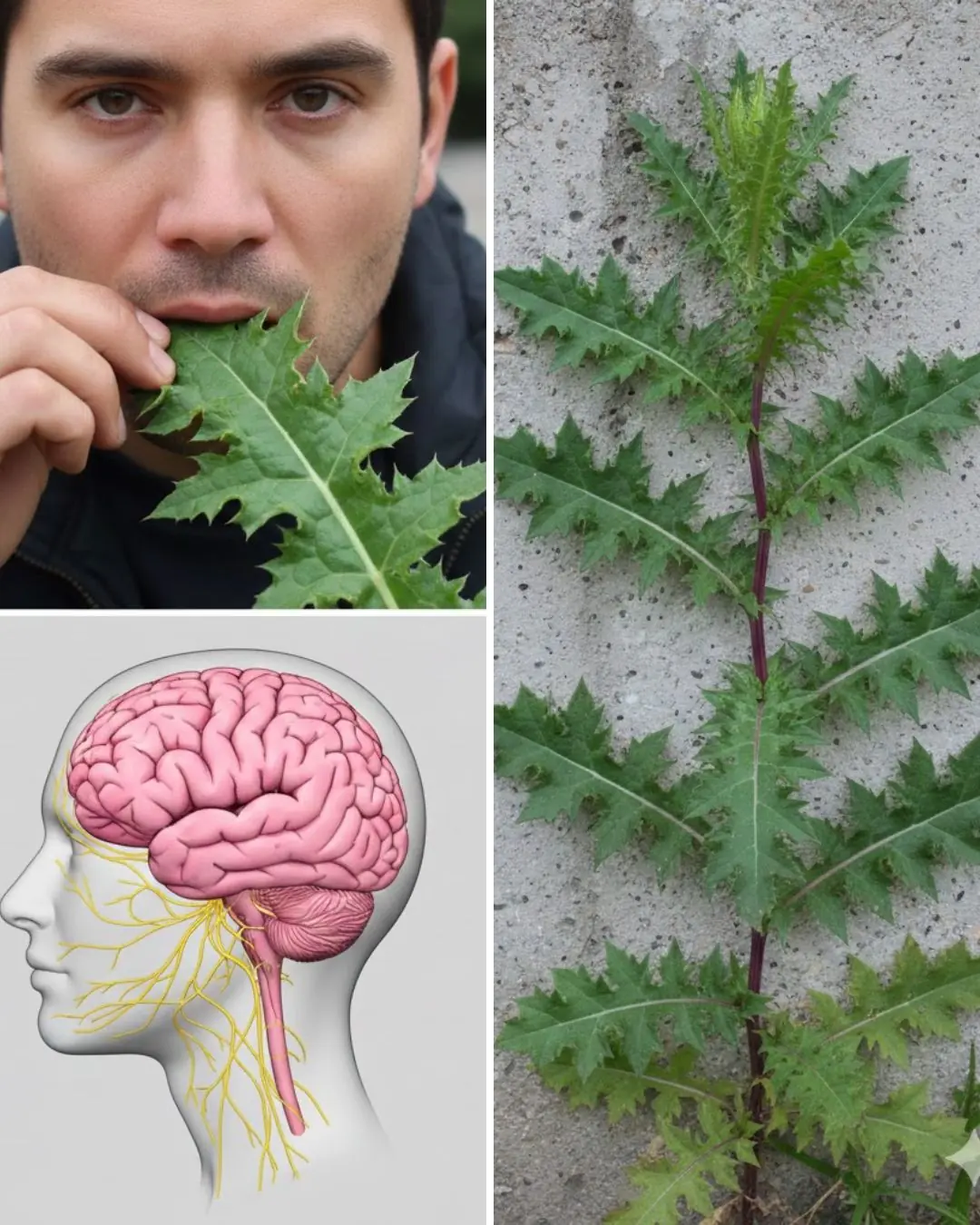
The Powerful Benefits of Eating Lactuca serriola Leaves (Prickly Lettuce)

The Desert Survivor That Preserves Cells, Fights Oxidation, and Commands Respect

The Health Benefits and Uses of Broadleaf Plantain (Plantago major)

White Clover (Trifolium repens): 15 Benefits and Homemade Uses

Stinging Nettle (Urtica dioica): The Hidden Power of Leaves and Seeds

It's a pain killer, helps relieve leg pain, varicose veins, rheumatism, and arthritis...👇

4 Fruits You Should Eat in Moderation After 60 — And How to Enjoy Them Without Losing Muscle
15 Strange Early Signs of Liver Failure That Even Doctors Often Miss

The Real Power of Dandelion Is in the Root

The Hidden Power of Puncture Vine Fruit (Tribulus terrestris)

Tradescantia zebrina: The Colorful Healer Hidden in Plain Sight

Willow Catkins – The Forgotten Spring Medicine

The Hidden Power of Goosegrass

The Hidden Power of Common Blue Violet (Viola sororia) and Its Homemade Uses

She Served Divorce Papers at His VP Party

Signs and Symptoms of Oral Cancer

The Best Time To Drink Pomegranate Juice for Better Blood Pressure and Muscle Recovery

Why Your Cat Chooses to Sleep With You
