Cancer patients in England to be first in Europe to be offered immunotherapy jab

Beating Cancer in Five Minutes: How a Simple Injection Is Transforming Care in England
What if beating cancer could start with something as simple — and as swift — as a quick jab in the arm? For thousands of patients in England, that once-unimaginable scenario is now becoming reality. In a breakthrough hailed as a “game-changer” by oncologists and healthcare leaders alike, the NHS is rolling out a five-minute injectable form of the immunotherapy drug nivolumab, offering a faster, more convenient, and equally effective way to treat some of the most aggressive and common cancers.
For years, patients have endured lengthy sessions tethered to IV drips — hours spent in infusion chairs, waiting for life-saving medications to flow into their veins. Now, with the approval of this subcutaneous formulation of nivolumab, that wait time can shrink to mere minutes. England has become the first country in Europe to make this innovative version widely available, signaling a bold shift in how modern cancer care is delivered.
But this breakthrough is about much more than speed or convenience. It represents a deeper change in the way medicine confronts cancer — empowering the body’s own immune system to detect and destroy cancer cells while reducing the physical and emotional burden of treatment.
A Game-Changer in Treatment Delivery

For decades, cancer treatment has been synonymous with long hospital visits, sterile infusion rooms, and exhausting time commitments. That narrative is now changing. With the NHS offering a five-minute subcutaneous injection, patient care is entering a new era — one defined by efficiency, accessibility, and patient-centered design.
The injectable form of nivolumab, commercially known as Opdivo, received approval from the UK’s Medicines and Healthcare products Regulatory Agency (MHRA) as a safe and effective alternative to traditional intravenous (IV) therapy. Instead of 30 to 60 minutes hooked up to an IV line, patients can now receive the drug in just three to five minutes. NHS officials estimate that roughly 1,200 patients per month will benefit from the rollout, with eligibility spanning 15 cancer types, including lung, bowel, skin, kidney, and esophageal cancers.
The efficiency gains are striking. Patients who once scheduled half-day hospital trips for infusions can now plan for a quick visit and get back to their lives. According to NHS England, the time saved across the system could free up more than a year’s worth of clinical treatment hours annually, creating additional capacity to treat other patients faster.
This isn’t just a win for patients. Oncology departments — often stretched thin — will see significant relief. Professor Peter Johnson, NHS England’s National Clinical Director for Cancer, called the innovation “a remarkable step forward,” explaining that it will allow medical teams to treat more patients in less time while reducing pressure on nursing and pharmacy staff.
Equally important: this leap in convenience does not come with a higher price tag. Thanks to a pricing agreement with Bristol Myers Squibb, the drug’s manufacturer, the injectable version will be offered at the same cost as the IV formulation — a rare instance where innovation delivers better care without inflating costs.
How the Five-Minute Jab Works

At its core, cancer is a disease of deception — a master manipulator that hides from the immune system while growing unchecked. Immunotherapy flips that script. Instead of directly targeting tumors with chemicals or radiation, it trains the body’s immune system to identify and destroy cancer cells on its own.
Nivolumab belongs to a class of drugs called immune checkpoint inhibitors, which target a protein called PD-1 (programmed death-1) found on the surface of T-cells — the immune system’s frontline soldiers. Normally, PD-1 acts as a “brake,” preventing T-cells from attacking healthy tissue. But cancer cells exploit this mechanism, effectively switching off the immune response and avoiding detection.
By binding to PD-1, nivolumab removes that molecular disguise, allowing T-cells to recognize cancer as a threat and attack it. This approach has already proven effective in treating a wide range of cancers, from advanced melanoma to lung and kidney cancers, and often provides longer-lasting results compared to chemotherapy.
The newly approved subcutaneous formulation maintains the same level of efficacy as the IV version. Powered by ENHANZE® technology, developed by Halozyme Therapeutics, the drug is rapidly absorbed into the bloodstream through the tissue just beneath the skin. Clinical trials demonstrated that the injectable form achieves equivalent drug levels and safety profiles as the traditional infusion, meaning patients sacrifice nothing in terms of effectiveness.
Looking ahead, experts believe this breakthrough could pave the way for community-based or even at-home administration, expanding access for patients who live in remote areas or have mobility challenges.
Benefits for Patients — and for the NHS

For patients, the change is nothing short of transformative. Frequent, hours-long infusions can be physically draining, emotionally taxing, and logistically challenging — especially for those balancing work, childcare, or travel from distant communities. Cutting that time down to just minutes means less disruption, less stress, and more freedom to live life beyond the hospital walls.
Clinical trial participants overwhelmingly preferred the injection over IV infusions, citing greater comfort and convenience. Many patients reported that shorter treatment times allowed them to resume work, family life, or personal activities with minimal interruption.
The NHS, too, stands to gain. With fewer infusion chairs occupied and staff time freed up, oncology teams can redirect resources toward diagnosis, follow-up care, and other critical services. Over the course of a year, this could mean thousands of hours saved, directly benefiting both patients and healthcare providers in a system already under intense pressure.
Elizabeth O’Mahony, NHS England’s Chief Financial Officer, described the rollout as “a huge boost for patient care,” emphasizing how innovations like this enhance operational efficiency while keeping costs stable.
Meeting Real-World Challenges
The timing of this innovation is critical. Cancer rates are climbing worldwide, with troubling increases among younger adults. In the UK, cancers such as bowel and skin cancer are rising sharply among people under 50, a trend that continues to baffle researchers but underscores the urgency for scalable, efficient treatments.
At the same time, the healthcare system is still grappling with pandemic-related backlogs and record-high waiting times for cancer referrals. By reducing treatment sessions by an hour or more per patient, this rollout could significantly relieve systemic strain and enable oncologists to treat more patients faster.
Importantly, this shift reflects a broader evolution in cancer care — one that values not only survival but also quality of life. Faster, more flexible treatments help restore a sense of normalcy for patients, reducing the emotional toll of repeated hospital visits.
The Future of Cancer Care

The success of the five-minute nivolumab jab is opening the door for similar formulations of other biologic and immunotherapy drugs, potentially transforming care for a wide range of cancers and chronic diseases. Researchers are already exploring how other checkpoint inhibitors might be reformulated for subcutaneous delivery, making treatments faster and more accessible than ever before.
Experts emphasize, however, that continued innovation requires sustained investment and strategic planning. From supporting clinical trials to strengthening the NHS workforce, building the infrastructure to support next-generation care will be essential to fully realize the potential of such advancements.
Public Health Minister Ashley Dalton, herself a cancer survivor, called the rollout a testament to Britain’s leadership in medical innovation but stressed the need for continued momentum: “Our National Cancer Plan will not only improve survival rates but also redefine the experience of care for patients across the country.”
Hope, Progress, and the Quiet Power of Innovation
For patients facing cancer, time is everything. The five-minute nivolumab injection is more than a clinical milestone — it’s a human one. By shrinking treatment time without compromising results, it gives patients something priceless: more moments with loved ones, less time in hospitals, and renewed hope in the face of uncertainty.
This innovation is also a reminder that progress in healthcare isn’t always about discovering brand-new drugs. Sometimes, it’s about finding smarter, more compassionate ways to deliver the tools we already have — making life a little easier, and a lot more hopeful, for those in the fight of their lives.
As other nations watch England’s rollout, one message is clear: faster, more humane cancer care isn’t a dream of the future. In England, it’s already here — and it’s setting the standard for what modern medicine can and should be.
News in the same category

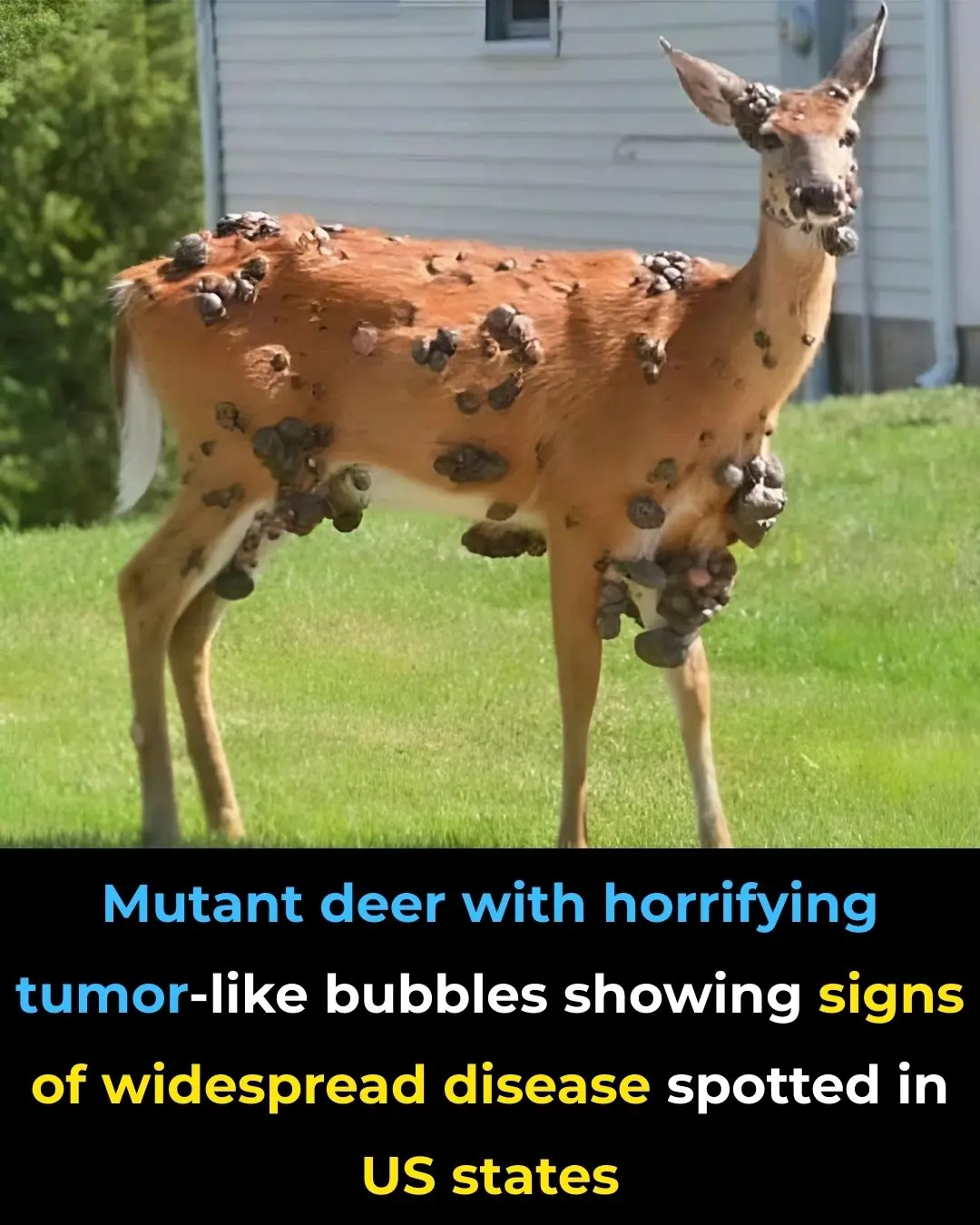
Mutant deer with horrifying tumor-like bubbles showing signs of widespread disease spotted in US states

'Frankenstein' creature that hasn't had s3x in 80,000,000 years in almost completely indestructible

Angelina Jolie’s ‘Zombie Lookalike’ Revealed As She Leaves Jail After Fooling Everyone

US assassin caught on CCTV faces lengthy prison sentence over failed murder plot

YouTuber shares shocking revenue earned from 1 million views on YouTube shorts

Trump makes worrying quip during Zelenskyy meeting that leaves many concerned over rising WW3 fears

Investigation into horrifying death of streamer 'tortured' for ten days before dying on camera

This New Eye Drops Could Clear Cataracts Without Surgery, Giving Millions a Safer Way to Restore Sight

Woman issues warning to MacBook users after simple mistake leaves her screen destroyed

Man trained like a professional athlete for 30 days and saw crazy changes to his body take place

ChatGPT CEO Warns: What You Tell AI Could Be Used as Evidence in Court
New Drug That Protects the Blood-Brain Barrier Shows Promise Against Alzheimer’s Disease

Firefighters Reveal the Worst Place to Keep Your Phone

Shocking new study reveals how long it takes to regain weight after stopping Ozempic

Elon Musk's estranged daughter shares her iconic reaction to 'woke mind virus tweet' claiming she was dead

Homeowner finds chilling note with terrifying warning left by previous owner after moving into new house

People are just discovering what 'proper poop position' is after seeing bizarre toilet design
News Post

14 hidden causes of tingling feet (and what to do)
At last — how to detox the brain naturally

5 Blood Clot Facts Doctors Want You to Know

8 Foods That Help Lower Your Cholesterol
6 Harmful Foods That Weaken Calcium Levels

8 Common Reasons For Waking Up at Night

How to Use Castor Oil to Regrow Eyelashes and Eyebrows

Scientifically Proven Health Benefits of Avocado and Avocado Seeds
Experts Say They’ve Pinpointed the Cause of Autism—And It Could Lead to New Treatments
Scientists Say Cancer Can Now Be Detected Years in Advance with Simple Blood Test

You Can Adopt Puppies That Were ‘Too Friendly’ to Become Police Dogs

A Nigerian Scientist Developed a High-Tech Cancer-Detecting Goggles That Help Surgeons Spot Cancer Cells More Accurately.

Final straw that led to billionaire CEO's desperate escape from Japan inside 3ft box
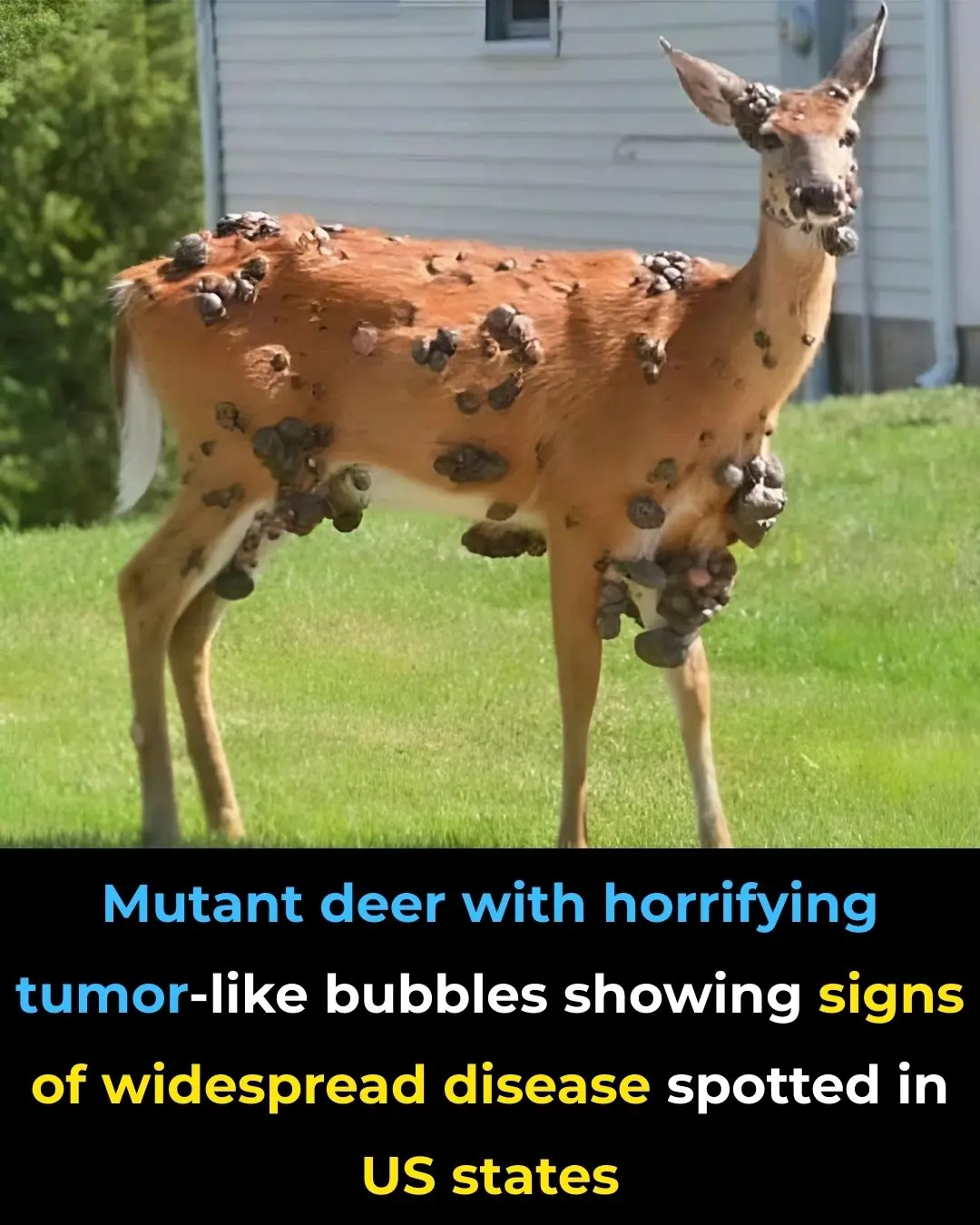
Mutant deer with horrifying tumor-like bubbles showing signs of widespread disease spotted in US states

'Frankenstein' creature that hasn't had s3x in 80,000,000 years in almost completely indestructible

Scientists discover ultra-massive 'blob' in space with a mass of 36,000,000,000 suns
When a Washing Machine Shows 7kg, 8kg, or 10kg, Is That the Weight of Dry or Wet Clothes? The Real Meaning Behind These Numbers Is Something That Few People Know

Place a Bowl of Salt in the Fridge: A Small Trick, But So Effective — I Regret Not Knowing It for 30 Years

If Your White Walls Are Dirty, Don’t Clean Them with Water — Use This Trick for a Few Minutes, and Your Wall Will Be as Clean as New