Daily Step Counts Combined With Genetic Risk Can Better Predict Type 2 Diabetes

A person’s daily step count, when analyzed alongside genetic susceptibility, can provide a more accurate assessment of type 2 diabetes (T2D) risk than either measure alone, according to new research. The findings suggest that individuals with a high genetic predisposition to T2D may need to achieve higher levels of daily physical activity to obtain the same protective benefits seen in those with lower genetic risk.
Understanding Type 2 Diabetes Risk
Type 2 diabetes is a chronic metabolic disease characterized by insulin resistance and impaired glucose regulation. Its development is influenced by a complex interaction between genetic factors and lifestyle behaviors, particularly physical activity, diet, and body weight. While regular exercise is widely known to reduce diabetes risk, this study highlights that the amount of activity required for meaningful risk reduction may differ from person to person based on genetic makeup.
Step Count Thresholds Vary by Genetic Susceptibility
Researchers found that step count thresholds associated with reduced T2D risk were not uniform across the population. Instead, they varied significantly according to an individual’s polygenic risk score (PRS), a measure that aggregates the effects of many genetic variants associated with diabetes susceptibility.
Individuals with low genetic risk experienced substantial reductions in T2D risk at relatively moderate daily step counts. In contrast, those with high polygenic risk needed to accumulate significantly more daily steps to achieve a comparable reduction in risk. This finding underscores that genetic susceptibility can modify how the body responds to lifestyle interventions such as physical activity.
The Role of Wearable Devices in Risk Assessment
The study leveraged wearable devices to objectively measure daily step counts, providing a more accurate representation of habitual physical activity than self-reported data. Wearable-derived metrics offer continuous, real-world insights into movement patterns and can capture subtle differences in activity levels that may influence metabolic health.
When researchers incorporated wearable-based step data into prediction models alongside polygenic risk scores, the models demonstrated improved accuracy in identifying individuals at elevated risk for type 2 diabetes. This combined approach outperformed models that relied solely on traditional clinical risk factors.
Why Genetics Matters
Polygenic risk scores reflect inherited susceptibility to metabolic dysfunction, including insulin resistance and impaired beta-cell function. For individuals with a high PRS, these underlying biological vulnerabilities may blunt the protective effects of lower levels of physical activity, making higher step counts necessary to counterbalance genetic risk.
Importantly, the findings do not suggest that physical activity is ineffective for those at high genetic risk. Rather, they emphasize that more intensive or sustained activity may be required to achieve meaningful protection.
Implications for Personalized Prevention
The results support a shift toward more personalized approaches to diabetes prevention. Instead of a single, universal step-count recommendation, future guidelines may benefit from incorporating genetic risk profiles to tailor physical activity targets.
For example:
-
Individuals at low genetic risk may achieve protection with moderate increases in daily steps.
-
Those at high genetic risk may benefit from higher step goals combined with additional lifestyle interventions such as dietary changes and weight management.
Such precision prevention strategies could improve adherence, motivation, and long-term outcomes by aligning recommendations more closely with individual risk profiles.
Public Health and Clinical Significance
Type 2 diabetes continues to rise globally, placing enormous strain on healthcare systems. Early identification of high-risk individuals is critical for effective prevention. The integration of wearable technology and genetic data offers a scalable and data-driven approach to risk stratification.
Clinicians may eventually use this combined information to guide personalized counseling, monitor progress over time, and intervene earlier in individuals most likely to benefit from targeted lifestyle modifications.
Conclusion
Combining daily step counts from wearable devices with polygenic risk scores significantly enhances the prediction of type 2 diabetes risk. The study demonstrates that genetic susceptibility influences the amount of physical activity required to reduce diabetes risk, with individuals at higher genetic risk needing higher daily step counts to achieve comparable benefits. These findings mark an important step toward personalized, precision-based strategies for preventing type 2 diabetes and improving metabolic health across diverse populations.
News in the same category
How to Naturally Increase Estrogen Levels

Evidence-Based Health Benefits of Honey (Raw, Pure, Natural) + Turmeric Golden Honey Recipe
Foamy Urine: Here’s Why You Have Bubbles in Your Urine
Why Almonds Are So Good for You: Health Benefits of Almonds Backed by Science
No Reset: When a Clinical Mindset Takes Over Your Whole Life

Dermatology Data Reinforce the Relative Safety of JAK Inhibitors
Can Cuffless Blood Pressure Devices Transform Cardiovascular Disease Prevention and Treatment?
Early-stage stomach cancer is often accompanied by these 6 symptoms

6 Things People Who Live to 100 Do Every Week to Stay Healthy

Seven Foods That Rarely Spoil: Still Safe to Eat Even After the Expiration Date

Five Parts of Fish That Are Dirty and Potentially Toxic — The First One Is Often Mistaken as Healthy but Can Be Fatal

Health Benefits of Boiled Green Bananas

How to Drink Lemon Turmeric Water in the Morning to Support Liver and Kidney Detox Without Harming the Stomach

Can Relative Fat Mass Replace BMI in Assessing Obesity?
When Women Target Other Women: The Hidden Wounds of Bullying in Medicine

Most Doctors Won’t Tell You, But This Can Cut Heart Attack & Stroke Risk By 80%

The Best Proven Ways to Heal Scars Naturally (Evidence Based)

16 Warning Signs of Poor Blood Circulation and How to Treat It

The Best Home Remedies For Getting Rid of Ear Infection
News Post

Tata Sierra vs Mahindra XUV 7XO: A Mid‑Size SUV Showdown 🚙🔥

This red, scaly patch won’t go away. It's all over my forehead and doctor isn't answering me. What is it?
I keep wondering why this happens to me
The Impressive Health Benefits of Guava Fruit and Leaves & How to Eat Guava (Evidence Based)
How to Naturally Increase Estrogen Levels

Evidence-Based Health Benefits of Honey (Raw, Pure, Natural) + Turmeric Golden Honey Recipe
Foamy Urine: Here’s Why You Have Bubbles in Your Urine
Why Almonds Are So Good for You: Health Benefits of Almonds Backed by Science
When Garlic Turns Harmful: Common Mistakes That Can Make a Healthy Food Risky
The Most Affordable Food That Supports Bone Health and Helps Fight Osteoporosis

Onion Water for Hair Growth: What It Can Do, What It Can’t, and What Science Really Says

A Cardiac Surgeon’s Warning: Why Many Elderly Patients Should Be Cautious About This Common Medication
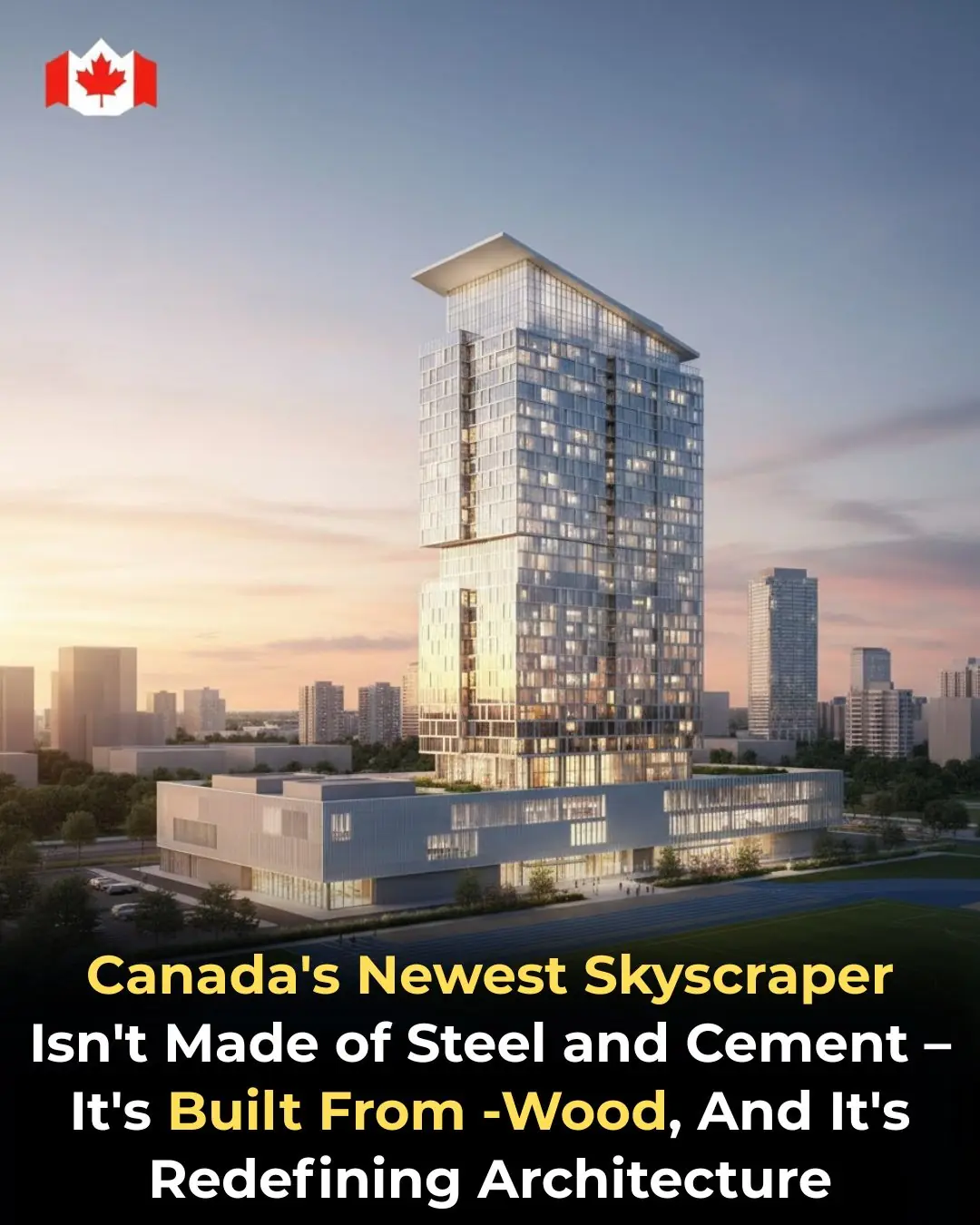
Canada Builds the Future in Wood: Inside Toronto’s Groundbreaking Timber Skyscraper

The Woman Who Refused to Quit: How Jacklyn Bezos Changed Her Life—and Helped Shape the Future of the World
San Francisco Establishes Reparations Fund Framework to Address Historical Racial Inequities

From Prison Food to Fine Dining: How Lobster Became a Luxury in America
No Reset: When a Clinical Mindset Takes Over Your Whole Life

India’s Olympic Ambition vs. Football’s Struggle ⚽🏟️🇮🇳

Brishti Gupta: Turning a Home Kitchen into Global Inspiration 👩🍳❤️🌍
