
The Brain’s Backup Plan: Neuroplasticity and Rehabilitation
When the brain is injured by trauma, stroke, or other forms of neurological damage, it does not simply regenerate lost nerve cells in the way skin or bone tissue can. Neurons in the central nervous system have a very limited capacity to divide and regrow, which is why brain injuries were once considered largely irreversible. However, modern neuroscience has shown that the brain possesses an extraordinary adaptive ability known as neuroplasticity. Rather than replacing damaged cells, the brain can reorganize itself by forming new neural connections and rerouting signals around injured areas, allowing lost functions to be partially or even substantially recovered.
Neuroplasticity works best when it is guided through structured and purposeful rehabilitation. Recovery is not an instant process; it depends heavily on time, repetition, and consistent training. Physical therapy plays a vital role by restoring movement, strength, balance, and coordination. Through repeated motor exercises, unaffected brain regions can gradually take over functions that were once controlled by damaged areas. Occupational therapy focuses on retraining everyday skills such as dressing, eating, writing, and cooking, helping patients regain independence in daily life. Cognitive rehabilitation targets mental abilities, including memory, attention, problem-solving, and language, which are often affected after brain injury or stroke.
Equally important is psychological and emotional support. Depression, anxiety, and loss of motivation are common after neurological injury and can significantly slow recovery if left untreated. Mental health counseling and social support help maintain engagement in therapy and encourage long-term perseverance, which is essential for harnessing neuroplastic changes. According to the World Health Organization (WHO), comprehensive rehabilitation that addresses both physical and psychological needs leads to better functional outcomes and quality of life.
Several medical and technological tools can further enhance recovery. Non-invasive brain stimulation techniques, such as transcranial magnetic stimulation (TMS), have shown promise in activating neural circuits and improving motor and cognitive outcomes when combined with therapy. Medications must also be carefully managed to avoid interfering with neural recovery. In addition, lifestyle factors such as adequate sleep, proper nutrition, and overall cardiovascular health play a crucial role in stabilizing new neural connections. Research from Harvard Medical School and the National Institute of Neurological Disorders and Stroke (NINDS) highlights that sleep and nutrition are essential for learning, memory consolidation, and brain repair.
The brain is especially responsive to rehabilitation in the early stages following injury, when neuroplasticity is at its peak. During this period, progress often occurs rapidly. However, scientific evidence confirms that meaningful improvements can still happen months or even years later, as long as therapy remains consistent and challenging. This understanding shifts the focus of recovery away from what is permanently lost and toward what can still be rebuilt.
Ultimately, brain recovery is not a fixed outcome but a dynamic process. By deliberately harnessing neuroplasticity through focused, repeated effort and comprehensive care, the brain can create new pathways that restore skills, function, and independence once thought to be gone.
News in the same category


Scientists Have Finally Figured Out What Causes ‘Hoarding’

Lab Study Shows Dandelion Root Kills Over 90% of Colon Cancer Cells In Just Two Days

Your Cat Might Love You More Than You Think—Here’s How to Tell
Woman Declared Dead for 8 Minutes Says She Discovered Death Is An Illusion

Reviving Italy’s Old Barns: Creative Studios Where Pottery and Bread Bring Generations Together

Sweden's Kindness Drawers: A Quiet Act of Sharing Fresh Bread with Those in Need

Urban Gardens in Italy: Transforming into Nighttime Sanctuaries for the Homeless

Modular Sleep Pods in Germany: A Subtle Solution for Refuge and Dignity in Public Spaces
A Month in Space Can Rapidly Age Human Stem Cells, Scientists Find
Hyperactive Brain Cells May Trigger Schizophrenia Symptoms—and Point to a Critical Window for Early Intervention
Even a month in space can leave your cells looking older.

Solar Flares Are Growing Hotter and More Powerful, Scientists Warn

12 Things That Seem Rude But Are Secretly Signs of Wisdom

Japan Just Hit 100,000 Citizens Over 100-Years-Old — Their Longevity Secret Isn’t What You’d Think
Why Highly Intelligent People Enjoy What Most People Avoid

12 Statements That Protect Your Self-Respect and Emotional Boundaries
Your Social Brain Starts Working Before You Can Smile
11 Polite Phrases Intelligent People Use to End Pointless Arguments
News Post

The Gut-Liver Connection: How Alcohol Impairs Immune Defenses and Exacerbates Liver Damage

Scientists Have Finally Figured Out What Causes ‘Hoarding’

Lab Study Shows Dandelion Root Kills Over 90% of Colon Cancer Cells In Just Two Days

Your Cat Might Love You More Than You Think—Here’s How to Tell
Woman Declared Dead for 8 Minutes Says She Discovered Death Is An Illusion

Reviving Italy’s Old Barns: Creative Studios Where Pottery and Bread Bring Generations Together

Sweden's Kindness Drawers: A Quiet Act of Sharing Fresh Bread with Those in Need

Urban Gardens in Italy: Transforming into Nighttime Sanctuaries for the Homeless

Modular Sleep Pods in Germany: A Subtle Solution for Refuge and Dignity in Public Spaces
A Month in Space Can Rapidly Age Human Stem Cells, Scientists Find
Hyperactive Brain Cells May Trigger Schizophrenia Symptoms—and Point to a Critical Window for Early Intervention

Tips for freezing tomatoes to enjoy year-round, keeping them fresh and delicious like they were just picked.

'You'll regret it if you throw away the water used to boil eggs: 4 clever ways to use it that you already know?'

Place this bunch of leaves in the bathroom: No unpleasant odors for a whole week, and it will repel mosquitoes and gnats.

Clever tip to get all the sand out of clams in a flash: No need to soak them for a long time, they'll be sparkling clean.
Even a month in space can leave your cells looking older.

Solar Flares Are Growing Hotter and More Powerful, Scientists Warn
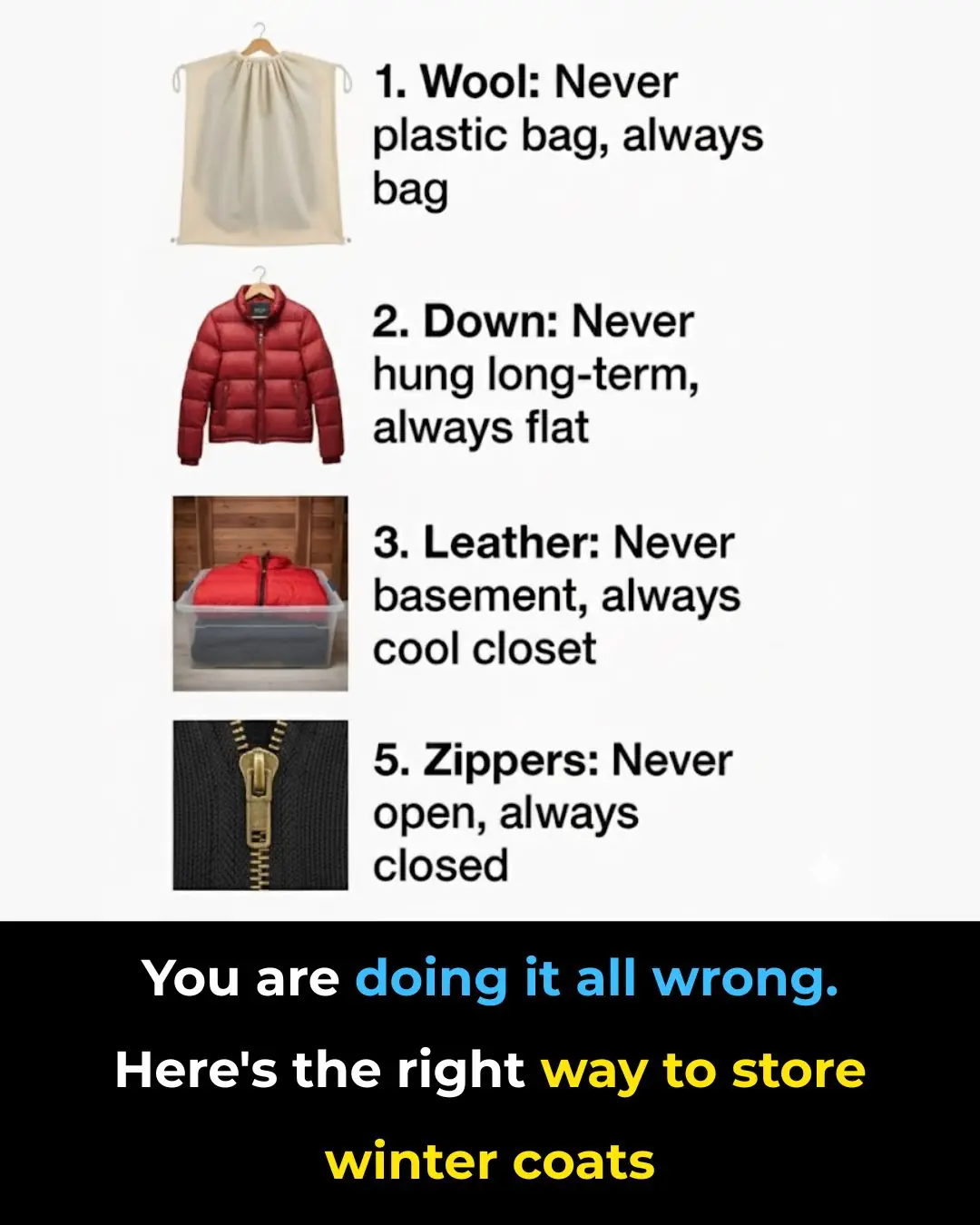
You’re Doing It All Wrong: The Right Way to Store Winter Coats
