Can Anti-Inflammatory Topical Therapy Fill the Treatment Gap in Mild Hidradenitis Suppurativa?
Hidradenitis suppurativa (HS) is a chronic, inflammatory skin disease characterized by recurrent painful nodules, abscesses, and sinus tract formation, most commonly affecting intertriginous areas such as the axillae, groin, and inframammary folds. Even in its mild forms, HS can significantly impair quality of life due to pain, scarring, and the unpredictable nature of flares.
Current management of mild HS often relies on repeated cycles of systemic or topical antibiotics and short courses of corticosteroids. While these treatments can reduce inflammation and control acute flares, they are associated with notable adverse effects and long-term limitations. This has prompted growing interest in alternative approaches—particularly anti-inflammatory topical therapies that may offer symptom control with fewer risks.
Limitations of Current Treatments for Mild HS
For patients with mild HS (Hurley stage I), first-line therapy typically includes topical clindamycin, oral antibiotics, or intermittent corticosteroids. However, these strategies present several challenges.
Repeated antibiotic use raises concerns about antimicrobial resistance, disruption of the skin and gut microbiome, and diminishing effectiveness over time. Systemic corticosteroids, although effective in rapidly suppressing inflammation, are not suitable for long-term use due to well-known adverse effects such as immunosuppression, metabolic disturbances, and rebound flares after discontinuation.
As a result, many patients with mild but persistent HS experience a cycle of temporary improvement followed by recurrence, without a sustainable long-term management option.
Rationale for Anti-Inflammatory Topical Creams
HS is increasingly understood as an inflammatory disorder rather than a purely infectious one. Dysregulation of the innate immune system, follicular occlusion, and elevated levels of proinflammatory cytokines such as TNF-α, IL-1, and IL-17 play a central role in disease pathogenesis.
This evolving understanding supports the potential role of targeted anti-inflammatory topical therapies that can directly modulate inflammation at the skin level without systemic exposure. Such treatments may reduce lesion activity, alleviate pain and tenderness, and potentially prevent progression when used early in the disease course.
Emerging Evidence From Case Series
Recent case series have reported promising results with the use of nonsteroidal anti-inflammatory topical creams in patients with mild HS. In these reports, patients applied the topical agent to active lesions once or twice daily over several weeks.
Improvements were observed in key clinical outcomes, including reduced lesion size, decreased erythema, diminished pain, and fewer inflammatory flares. Importantly, these benefits were achieved without the adverse effects commonly associated with systemic steroids or prolonged antibiotic therapy.
While these findings are preliminary and based on small patient numbers, they suggest that topical anti-inflammatory therapy may address a significant unmet need in mild HS management.
Safety and Tolerability
One of the most compelling advantages of topical anti-inflammatory creams is their favorable safety profile. Reported side effects have generally been mild and localized, such as transient irritation or dryness at the application site. No serious systemic adverse events have been documented in the available case series.
This safety profile makes topical therapy particularly attractive for long-term use, maintenance treatment, or early intervention—especially in younger patients or those with contraindications to systemic medications.
Clinical Implications
If further validated in larger, controlled studies, anti-inflammatory topical creams could become an important addition to the HS treatment algorithm. They may serve as:
-
A first-line option for mild HS
-
A steroid-sparing alternative for patients with frequent flares
-
A maintenance therapy to prolong remission and reduce antibiotic dependence
Such an approach aligns with the broader goal of minimizing systemic treatment exposure while maintaining effective disease control.
Future Directions
Despite encouraging early data, randomized controlled trials are needed to confirm efficacy, identify optimal formulations, and establish standardized treatment protocols. Future research should also explore whether early topical anti-inflammatory intervention can alter disease trajectory and prevent progression to more severe HS stages.
Conclusion
Mild hidradenitis suppurativa is commonly managed with antibiotics and corticosteroids, therapies that carry significant limitations and risks when used repeatedly. Emerging evidence from case series suggests that anti-inflammatory topical creams may offer a safer, more sustainable alternative by directly targeting cutaneous inflammation. While further research is essential, topical anti-inflammatory therapy represents a promising step toward more patient-centered and long-term management of mild HS.
News in the same category

GIP Reduces Postprandial Glucose Peaks but Does Not Prevent Hypoglycaemia in Men With Type 1 Diabetes
How Swimming Rewires the Brain and Strengthens Cognitive Health

How the Right Foods Boost Immunity and Speed Up Recovery

The Science of Touch: How Hugging Improves Stress, Mood, and Immunity
How Gut Bacteria Influence Anxiety, Stress, and Emotional Well-Being
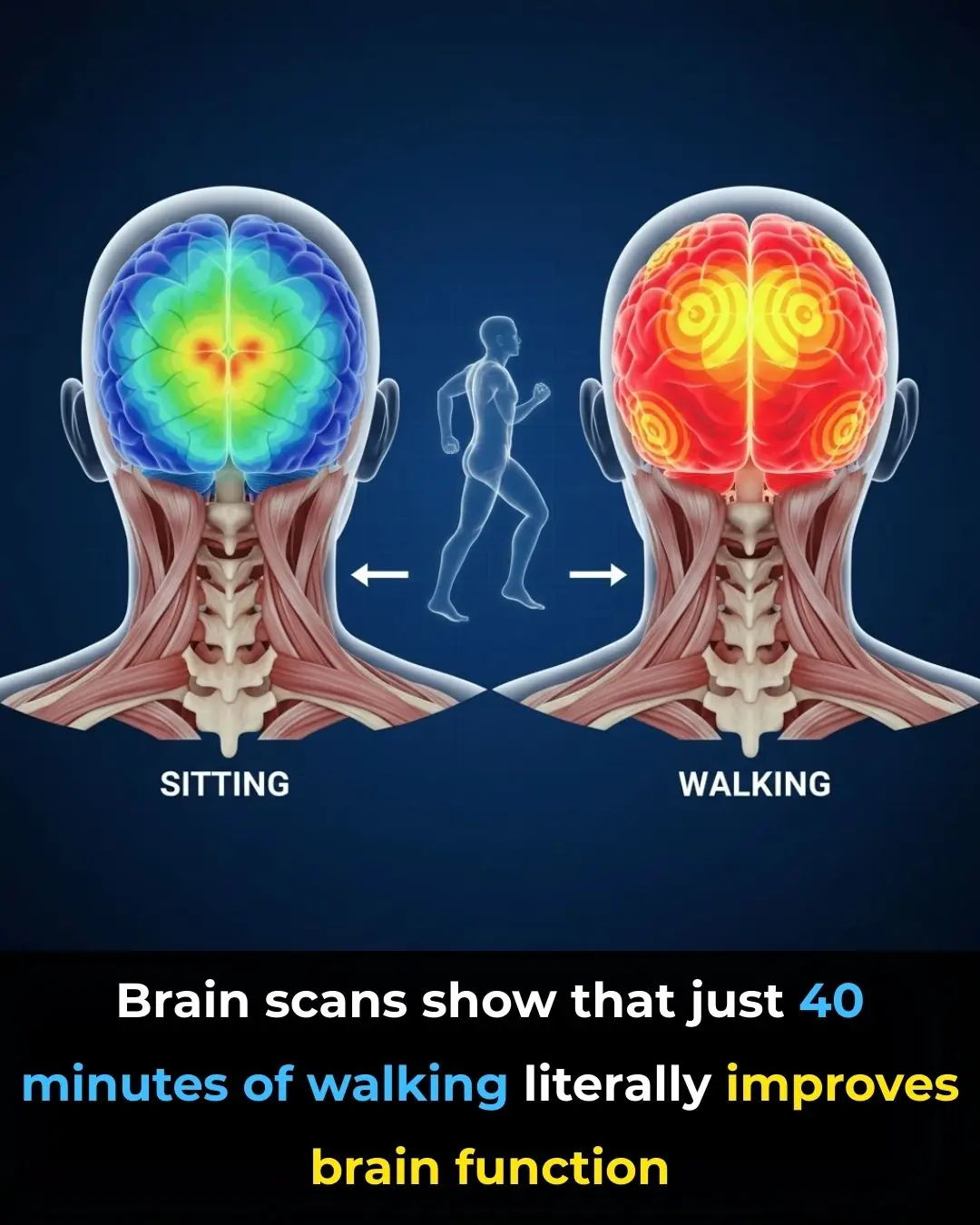
Your Brain on Walking: Why Movement Sparks Mental Clarity
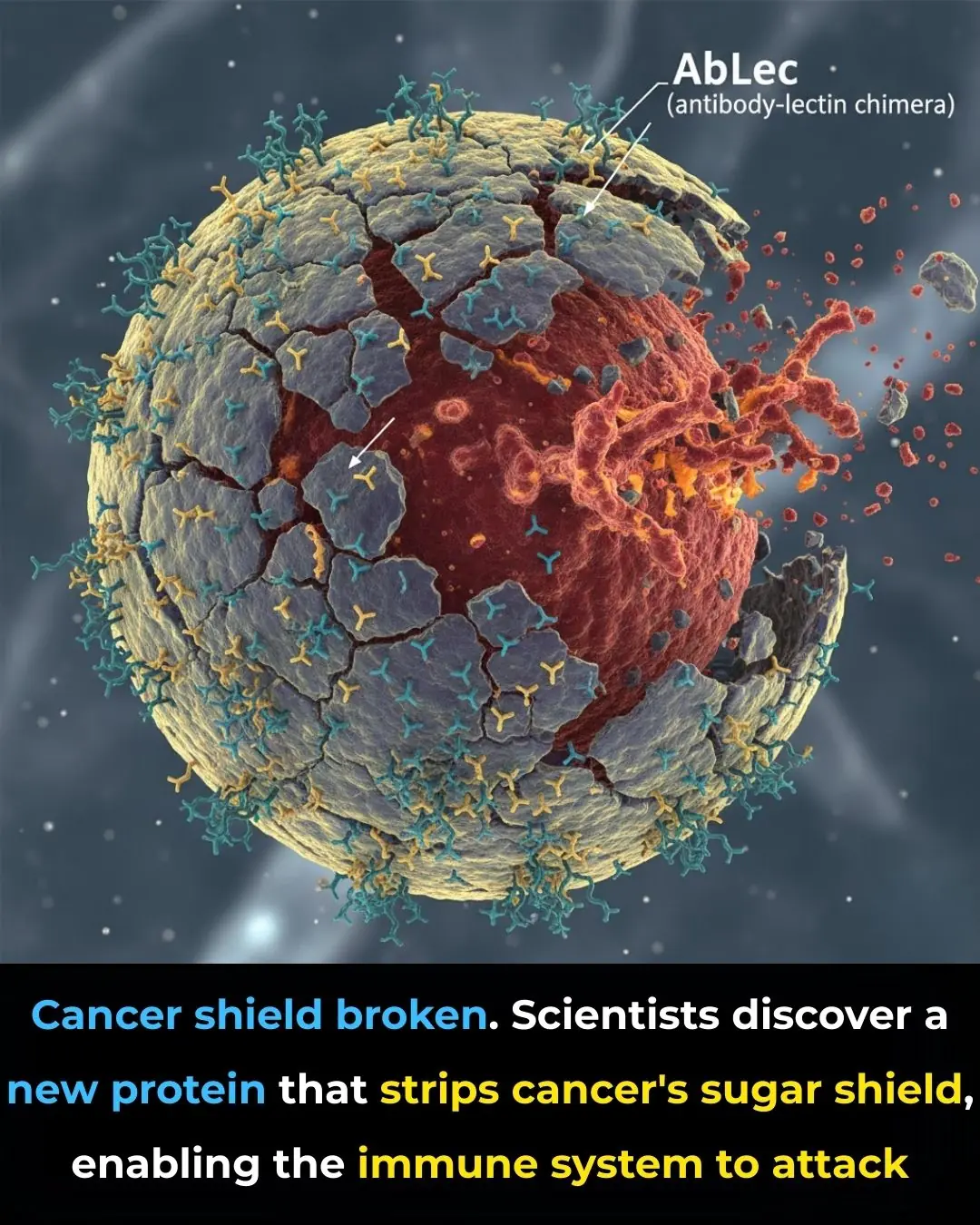
New Protein Breakthrough Helps Immune System Unmask and Destroy Cancer Cells

Using Star Apple Leaves to Treat Acid Reflux: A Traditional Remedy
Early-stage fatty liver disease: 5 obvious signs that can be noticeable on your face; ignoring them could lead to serious health consequences

Walking Barefoot at Home
Stroke and Cerebral Infarction Prevention:

If You Notice This Sign on Your Ear, Here’s What It Could Mean

5 Foods That Boost Immunity Better Than Garlic
What Is Stomach Cancer?
How the “3-2-1” Rule Can Help You
What Is the Adam’s Apple
Proven Inflammatory Foods to Avoid According to Science

14 Signs Your Blood Sugar Is Way Too High (And 14 Ways to Reduce It)
News Post
10 Scientifically Backed Reasons Why You Should Consume Ginger Everyday

He Thought I Was Doing Nothing at Home—Until I Left for a Week and Showed Him the Truth

GIP Reduces Postprandial Glucose Peaks but Does Not Prevent Hypoglycaemia in Men With Type 1 Diabetes
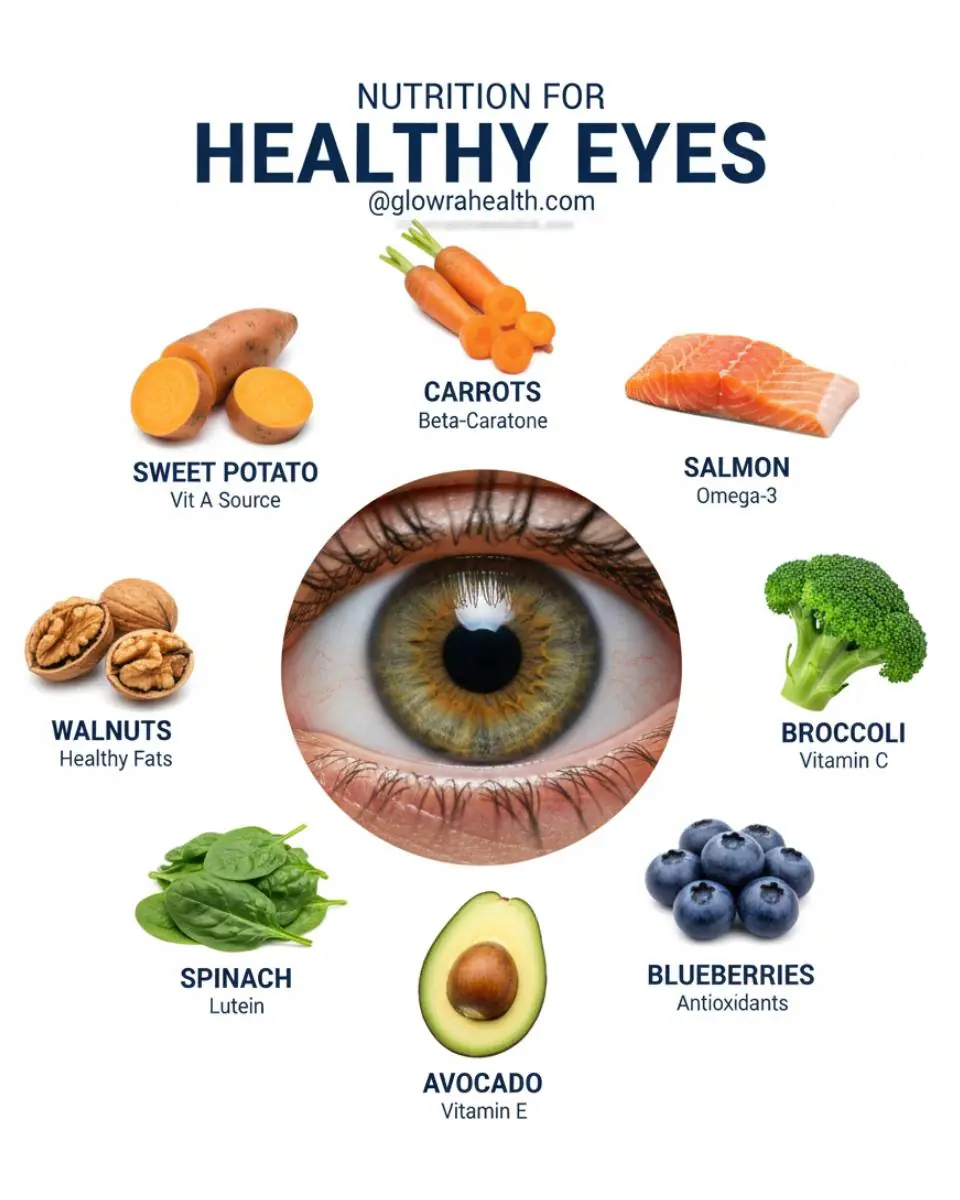
Feed Your Eyes: The Power of Nutrition for Better Vision

More Than Nutrition: Vegetables That Protect Your Cells

This Aloe Vera Recipe May Naturally Support Your Body’s Defense Against Bacteria and Fungi

Pharmacies Will Never Reveal This Secret – The Leaf That May Support Cancer Cell Defense | Exploring Soursop’s Natural Potential

7 Key things about Crabgrass
Guava Leaves: 12 Benefits and Uses

India Creates History at the Asian Para Youth Games 2025 🏅🇮🇳✨

Toxic Teaser Storm: Yash Redefines Cinematic Hype 🎬🔥

India’s Next Rail Leap: Vande Bharat Sleeper Train Aces Final High‑Speed Trial 🚆🇮🇳

Dashavatar: Marathi Cinema’s Historic Leap to the Academy Awards 🏆🌍✨
Supreme Court of India Reaffirms Merit in Public Employment ⚖️🇮🇳
The iBomma Shockwave: How Immadi Ravi’s Arrest Exposed a Cybercrime Empire 🎬🔥
Steaming crab often results in the claws falling off and a fishy smell, but a chef reveals: Just follow these steps and the crab will be sweet, the meat won't dry out, and it will be incredibly fragrant.

Don't put shrimp in the refrigerator right away after buying them; add one spoonful of this sweet seasoning and they'll stay fresh for a long time.
When simmering bones, you absolutely must add these three spices; the broth will be clearer and incredibly fragrant.
