Vitamin K2 Supplementation and Vascular Health in Chronic Kidney Disease
Vitamin K2 Supplementation and Vascular Health in Chronic Kidney Disease
Cardiovascular disease is the leading cause of morbidity and mortality in patients with chronic kidney disease (CKD), particularly in those with moderate to advanced disease. One of the key drivers of this elevated risk is accelerated vascular aging, characterized by arterial wall thickening, atherosclerosis, and pathological calcification. Conventional treatments have had limited success in slowing these processes, prompting interest in nutritional interventions that target underlying mechanisms of vascular damage. A randomized controlled trial published in Clinical Nutrition in 2015 provides important evidence that low-dose vitamin K2 supplementation may slow the progression of arterial changes in patients with CKD stages 3–5.
In this study, adults with chronic kidney disease were randomly assigned to one of two groups. The intervention group received 90 micrograms per day of vitamin K2 in the form of menaquinone-7 (MK-7), along with low-dose vitamin D, while the control group received vitamin D alone. This design allowed the researchers to isolate the specific contribution of vitamin K2, since vitamin D is commonly prescribed to CKD patients and can influence calcium metabolism. Participants were followed for nine months, during which vascular structure and biochemical markers of calcification were carefully monitored.
The primary outcome was carotid intima-media thickness (CIMT), a well-established, noninvasive measure of arterial wall thickening and early atherosclerosis. CIMT progression is strongly associated with future cardiovascular events, making it a clinically meaningful surrogate marker. After nine months, the difference between groups was striking. In the vitamin K2 group, carotid artery wall thickness increased by only 0.06 mm, compared with an increase of 0.136 mm in the vitamin D–only group. This represents a reduction in arterial thickening of more than 55%, indicating a substantially slower rate of plaque development in patients receiving vitamin K2.
In addition to structural vascular changes, the study examined biochemical markers related to arterial calcification. Vitamin K2 supplementation significantly reduced levels of dephosphorylated-uncarboxylated matrix Gla protein (dp-ucMGP), a circulating marker of vitamin K deficiency that is closely linked to vascular calcification. Matrix Gla protein is a potent inhibitor of calcium deposition in blood vessel walls, but it requires vitamin K–dependent activation to function properly. Elevated dp-ucMGP levels reflect inactive protein and are associated with increased cardiovascular risk, particularly in CKD. The observed reduction in dp-ucMGP suggests that vitamin K2 improved vascular calcification defense mechanisms at the molecular level.
Interestingly, coronary artery calcium scores did not change significantly in either group over the nine-month study period. This finding is not unexpected, as coronary calcification tends to progress slowly and may require longer follow-up to detect meaningful differences. The stabilization of coronary calcium, combined with slowed carotid thickening and improved calcification biomarkers, suggests that vitamin K2 may exert early protective effects that precede detectable changes in more advanced calcified lesions.
The biological plausibility of these findings is strong. Patients with CKD frequently exhibit functional vitamin K deficiency due to dietary restrictions, impaired metabolism, and medication use. This deficiency compromises the activation of vitamin K–dependent proteins that protect the vasculature from calcification. By restoring vitamin K2 availability, MK-7 supplementation may help normalize these protective pathways and slow vascular deterioration.
In conclusion, this randomized controlled trial published in Clinical Nutrition demonstrates that a small daily dose of vitamin K2 (90 micrograms of MK-7) significantly slowed carotid artery wall thickening and improved markers of vascular calcification in patients with CKD stages 3–5 (Clinical Nutrition, 2015). Although longer trials are needed to determine whether these effects translate into fewer cardiovascular events, the findings suggest that vitamin K2 supplementation may represent a simple, well-tolerated, and biologically targeted strategy to reduce cardiovascular risk in a highly vulnerable population.
News in the same category

Daily Prune Consumption and Bone Health in Postmenopausal Women
Montmorency Tart Cherry Juice as an Adjunctive Therapy in Ulcerative Colitis

Methylene Blue–Based Photodynamic Therapy as a Selective Strategy Against Breast Cancer Cells
Regenerating True Articular Cartilage: A Breakthrough in Joint Repair

Deuterium-Depleted Water and Long-Term Survival in Cancer Patients: Evidence from a Hungarian Population-Based Analysis

Daily cocoa extract supplements lowered cardiovascular disease deaths by 27%

Ivermectin stopped aggressive cancer cells from moving and spreading in lab tests
The Best Natural Gout Treatments: Remove Uric Acid Crystallization To Prevent Gout And Joint Pain
Quickly Drain You Lymph System Using Theses Simple Techniques to Boost Immunity and Remove Toxins

The Top 20 Essential Oils to Relieve Pain and Inflammation (Research Based)
Headache Above or Behind the Left Eye: Causes and Treatments
Root Canals May Lower Risk of Heart Disease, Diabetes

Mother-to-Infant Microbiome Transmission: Beyond Bacteria to Genes

Vitamin C Supplementation and Its Targeted Impact on the Human Gut Microbiome

Sleep and Dementia Risk: What You Should Know
Warning: 4 things to avoid when napping to prevent illness

The Amazing Benefits of Guava Leaf Water That Few People Know
Are Vaccines Doing More Than Just Preventing Infection?
News Post
Australian HPV Vaccination Marks Cervical Cancer Milestone

My outdoor faucet suddenly froze and now I’m seeing water seeping indoors — what should I do before a plumber can come?

Daily Prune Consumption and Bone Health in Postmenopausal Women
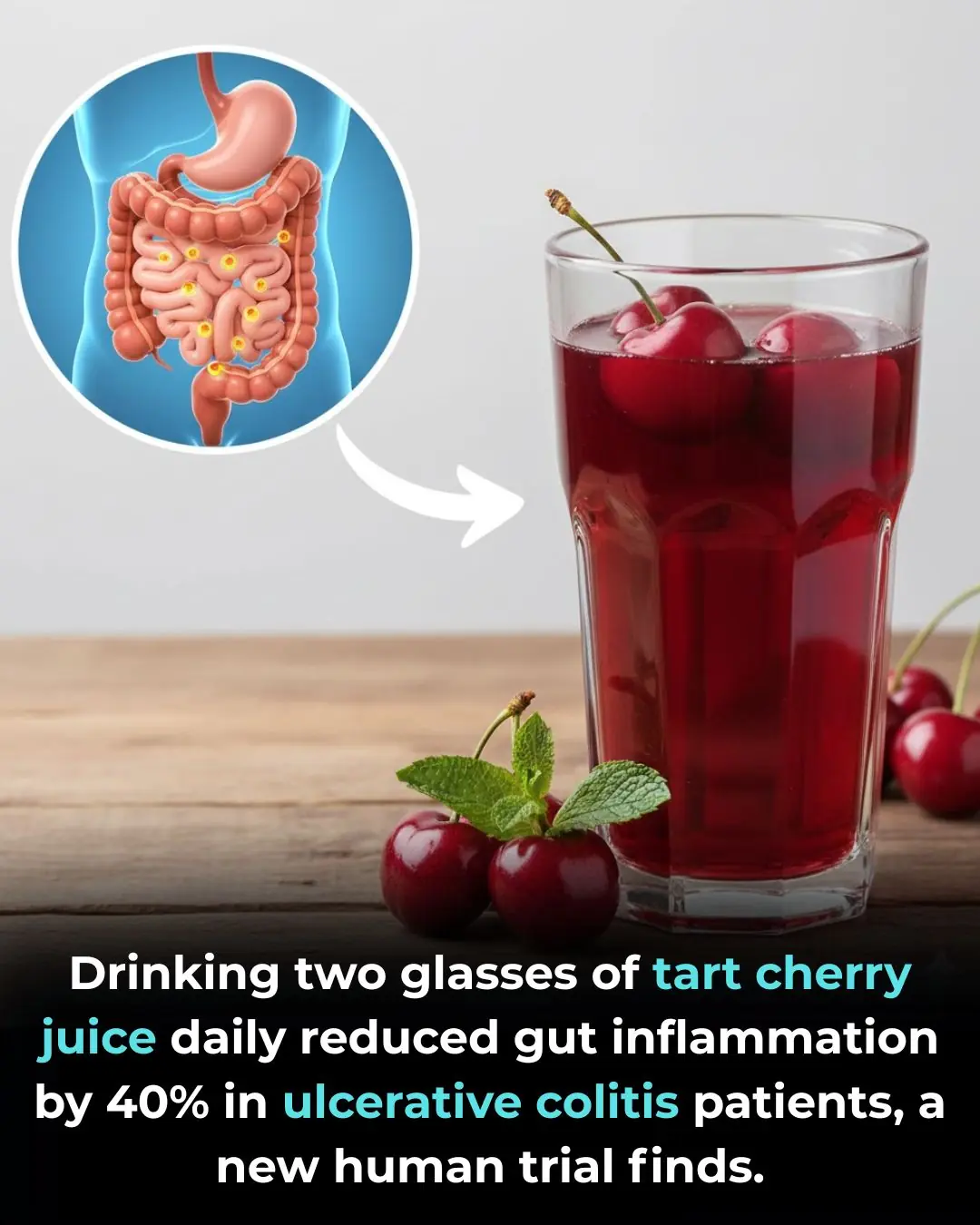
Montmorency Tart Cherry Juice as an Adjunctive Therapy in Ulcerative Colitis

Methylene Blue–Based Photodynamic Therapy as a Selective Strategy Against Breast Cancer Cells
Regenerating True Articular Cartilage: A Breakthrough in Joint Repair

Deuterium-Depleted Water and Long-Term Survival in Cancer Patients: Evidence from a Hungarian Population-Based Analysis

Daily cocoa extract supplements lowered cardiovascular disease deaths by 27%

Ivermectin stopped aggressive cancer cells from moving and spreading in lab tests
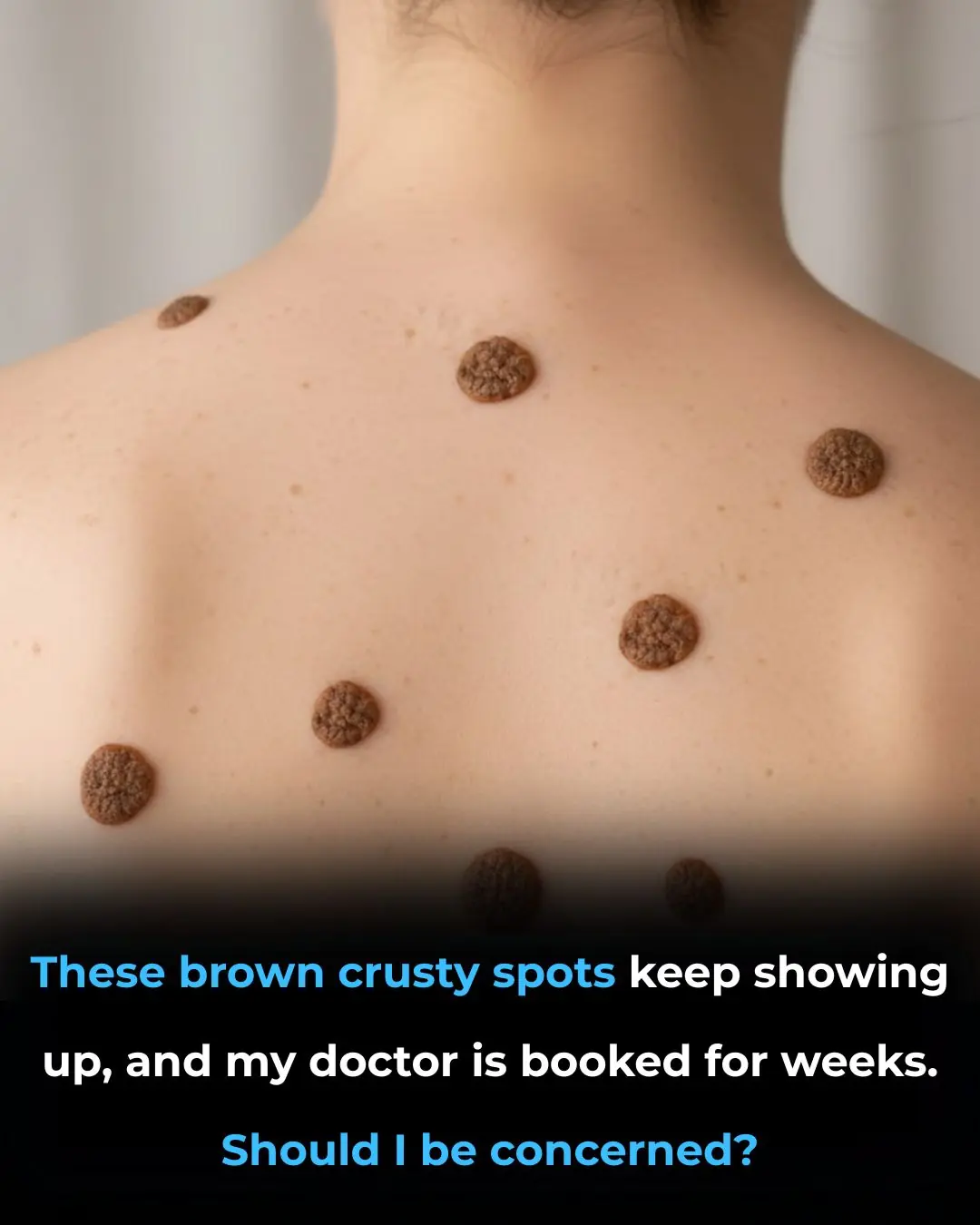
These brown crusty spots keep showing up, and my doctor is booked for weeks given Christmas. Should I be concerned?
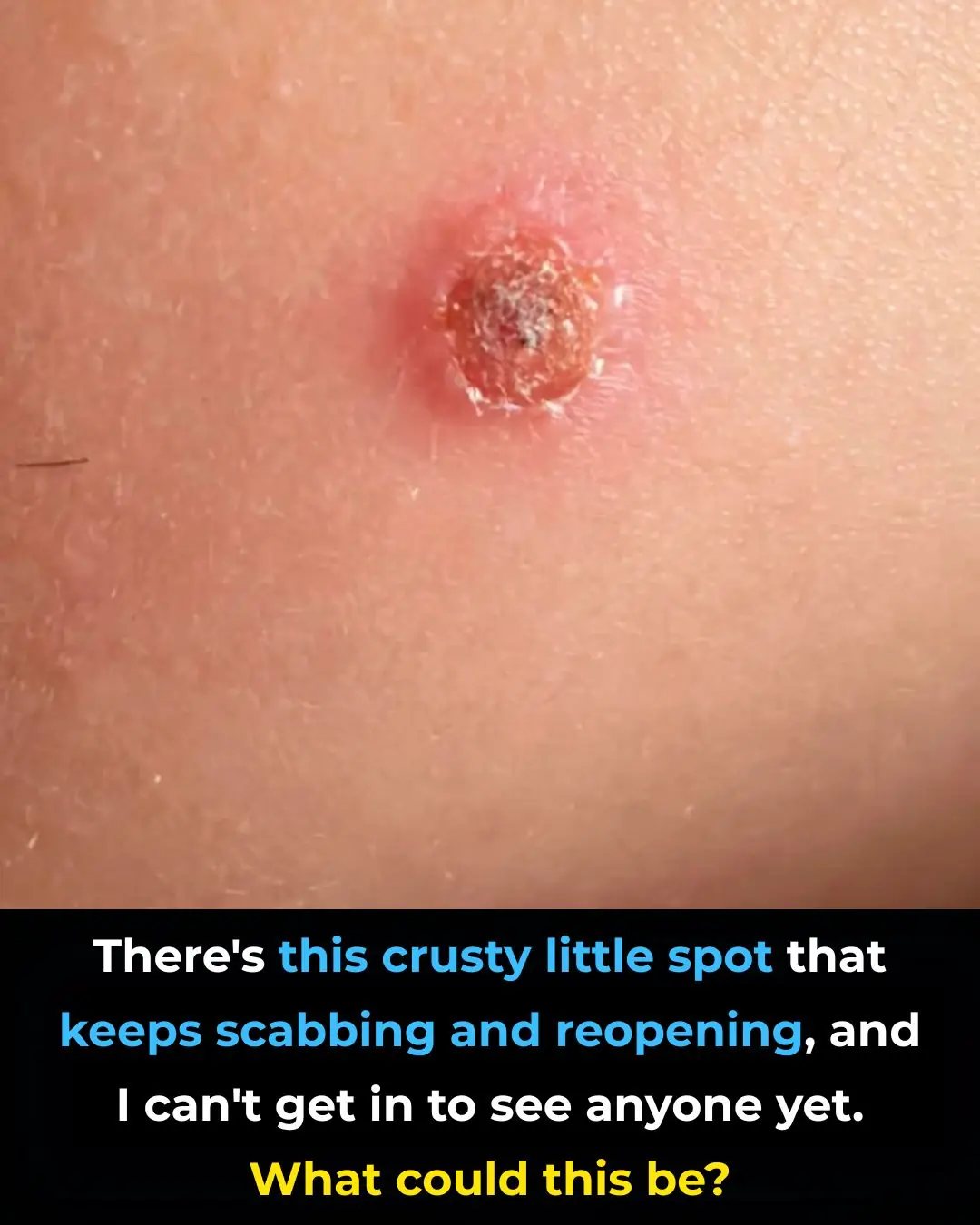
There’s this crusty little spot that keeps scabbing and reopening, and I can’t get in to see anyone yet. What could this be?

I had no clue about this

My fingertips keep splitting open in the cold, but I can’t get in to see the doctor anytime soon. What can I do now?
The Best Natural Gout Treatments: Remove Uric Acid Crystallization To Prevent Gout And Joint Pain
Quickly Drain You Lymph System Using Theses Simple Techniques to Boost Immunity and Remove Toxins

The Top 20 Essential Oils to Relieve Pain and Inflammation (Research Based)
Headache Above or Behind the Left Eye: Causes and Treatments
Root Canals May Lower Risk of Heart Disease, Diabetes